PREVENT Supports Early PCI for Vulnerable Plaques, with Reductions in MACE
Seung-Jung Park
Asan Medical Center, Republic of Korea
At Transcatheter Cardiovascular Therapeutics Asia Pacific (TCTAP) 2024, a landmark study is to be presented, which was also published in The Lancet, providing compelling evidence supporting the efficacy of prophylactic percutaneous coronary intervention (PCI) to treat vulnerable plaques on top of optimal medical therapy (OMT) in reducing the incidence of serious cardiovascular (CV) events over a 2-year period. The findings support expanding PCI indications to encompass non-flow-limiting, high-risk vulnerable plaques, and will support a paradigm shift in the management of CV disease.
Key Insights from the PREVENT Trial
Preventive PCI or Medical Therapy Alone for Vulnerable Atherosclerotic Coronary Plaque (PREVENT) enrolled 1,606 patients at 15 centers in 4 countries who had non-flow-limiting vulnerable coronary plaques of > 50% stenosis and a negative fractional flow reserve (FFR) of > 0.80. The mean age of the patients was 64 years, and 27% were women. Vulnerable plaques were defined as lesions possessing at least two of these characteristics: a minimal lumen area (MLA) of less than 4°§0 mm©ų, a plaque burden of more than 70%, a lipid-rich plaque by near-infrared spectroscopy (NIRS) (defined as maximum lipid core burden index within any 4 mm pullback length [maxLCBI4mm] >315), or a thin-cap fibroatheroma detected by radiofrequency intravascular ultrasonography (RF-IVUS) or optical coherence tomography (OCT) (Figure 1). Ultimately, 95% of patients in the trial were assessed by grayscale intravascular imaging, not newer, more sensitive imaging modalities.
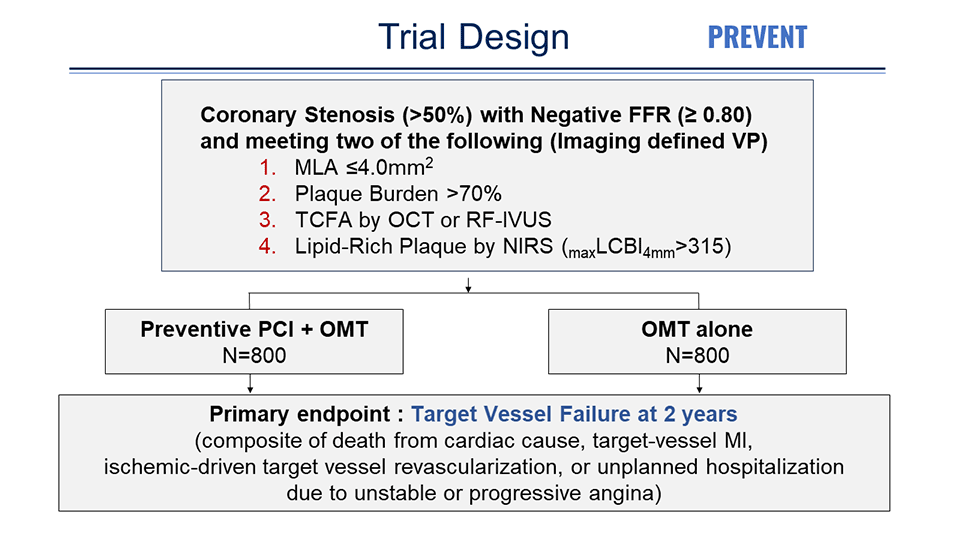
Patients were randomly assigned to PCI plus OMT or OMT alone. Although the trial was initially designed to use bioresorbable vascular scaffolds, with their removal from the market, permanent metallic everolimus-eluting stents were used instead. As a result, in the PCI group, drug-eluting stents (DESs) were used in 67% and bioresorbable scaffold in 33%. Intravascular imaging was used in all cases to optimize stent or scaffold implantation.
More than 50% of patients in both groups were on high- or moderate-intensity statins plus ezetimibe during the follow-up period. The mean low-density lipoprotein (LDL)-cholesterol level in both groups was 64 mg/dL at last follow-up, down from a median of 83 mg/dL at baseline in the preventive PCI group and 93 mg/dL in the OMT group.
In the trial, patients randomized to the preventive PCI group had an 89% lower risk of the composite primary endpoint of cardiac death, target-vessel myocardial infarction (MI), ischemia-driven target vessel revascularization, or hospitalization for unstable or progressive angina at 2 years compared with those in the OMT group (0.4% vs. 3.4%; hazard ratio [HR] 0.11; 95% confidence interval [CI] 0.03-0.36) (Figure 2).
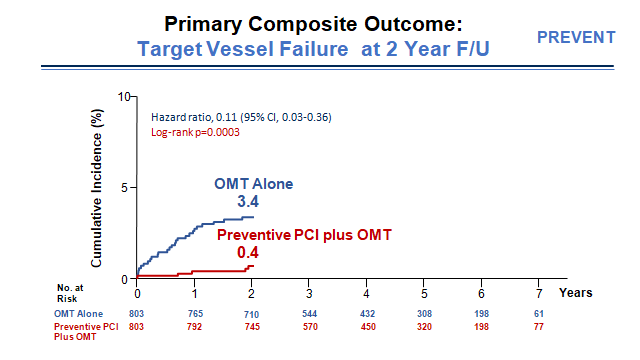
The number-needed-to-treat (NNT) to prevent one primary outcome event over 2 years in the preventive PCI group was 45.4, with a NNT of 87.7 to prevent one cardiac death or target-vessel MI.
Reduction in CV events sustained up to 7 years
Over the long-term follow-up, the primary outcome occurred less frequently in the preventive PCI group than in the medical therapy alone group (6.5% vs 9.4%; HR 0.54; 95% CI 0.33-0.87) (Figure 3). The absolute difference of 3% in the primary composite endpoint was sustained through 7 years of follow-up, with a median of 4.4 years. This study underscores the enduring impact of early intervention strategies in reducing adverse CV events associated with vulnerable plaques.
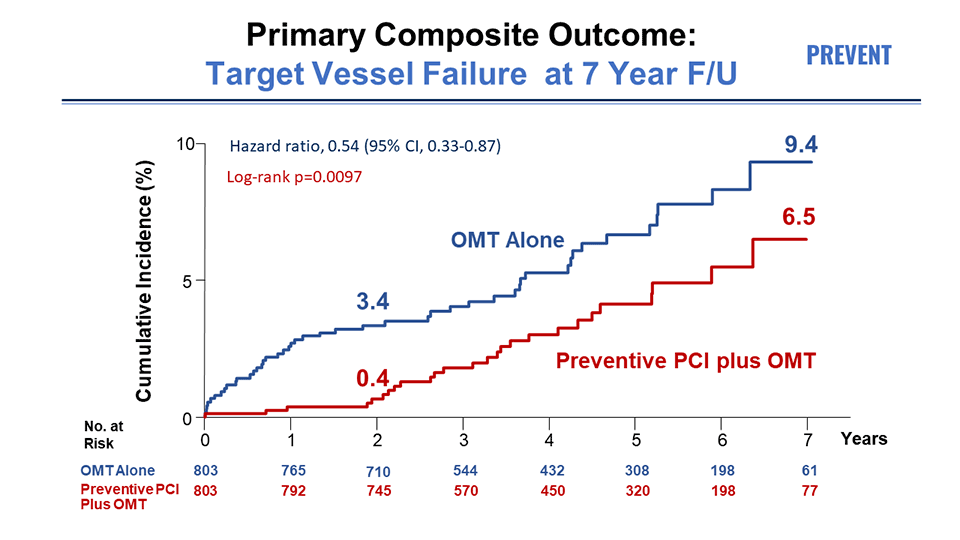
In an analysis of the patient-oriented composite outcome (death from any cause, any MI, or any repeat revascularization), the preventive PCI group had consistently lower incidence rates at 2 years and 7 years (log-rank P = 0.022).
Conflicting responses and future directions
While the PREVENT trial findings have been received with enthusiasm, they have also prompted debate and raised questions regarding the management and identification of vulnerable plaques. Some experts caution against extrapolating results, emphasizing the need for a holistic approach to managing vulnerable lesions beyond focal stenting, incorporating aggressive primary prevention strategies, such as proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors.
Challenges remain regarding accurate identification of vulnerable plaques, with some experts highlighting the limitations of grayscale IVUS in detecting these lesions. Regardless, the study provides valuable insights into preventive PCI, paving the way for future research to address remaining questions and concerns.
Conclusion
The PREVENT trial holds significance as the first large-scale, randomized controlled trial (RCT) comparing preventive PCI plus OMT versus OMT alone for non-flow-limiting vulnerable plaques. While offering valuable insights, further investigation is necessary to refine treatment strategies and optimize patient outcomes in the management of high-risk vulnerable plaques.
Hot Topics
Vulnerable Plaque Treatment 2024
Friday, April 26, 2:00 PM ~ 3:20 PM
Main Arena, Level 2
Edited by

Sang-Cheol Cho , MD
Yeosu Jeil Hospital, Korea (Republic of)
