Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-117
Sandwich in the Lab
By Cliff Li, Fahim Haider Jafary
Presenter
Cliff Li
Authors
Cliff Li1, Fahim Haider Jafary1
Affiliation
Tan Tock Seng Hospital, Singapore1,
View Study Report
TCTAP C-117
Coronary - Complication Management
Sandwich in the Lab
Cliff Li1, Fahim Haider Jafary1
Tan Tock Seng Hospital, Singapore1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
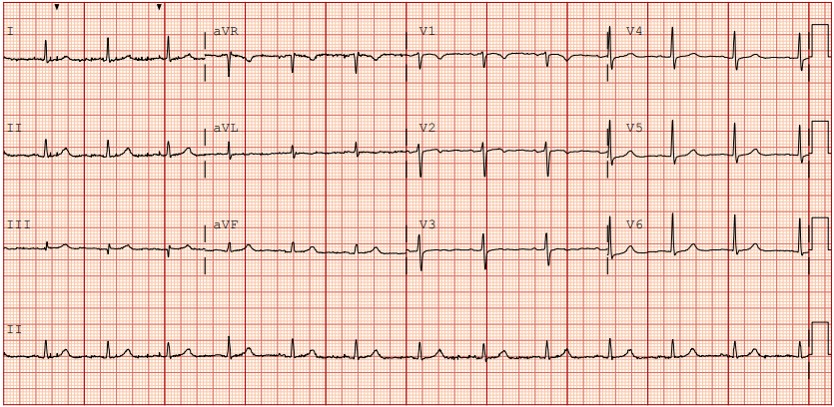
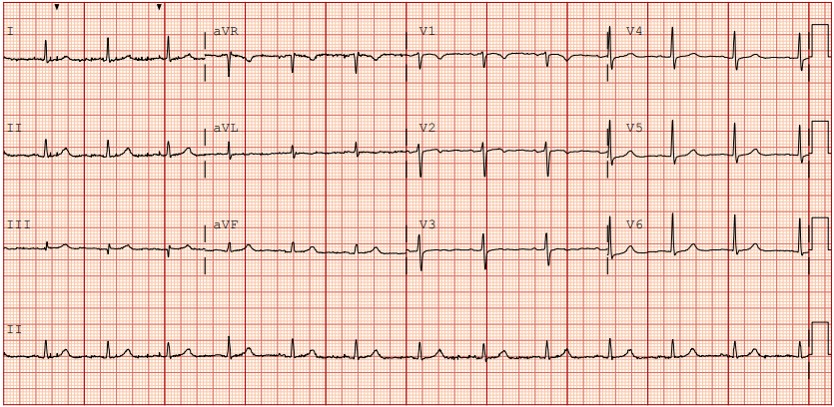
This case report presents the nuanced management of an 88-year-old male with a history of hypertension, hyperlipidemia, and diabetes mellitus. The patient presented with a one-day history of chest pain, accompanied by an unremarkable ECG and serial troponin levels. A diagnosis of unstable angina prompted the decision to conduct a coronary angiogram.
Relevant Test Results Prior to Catheterization
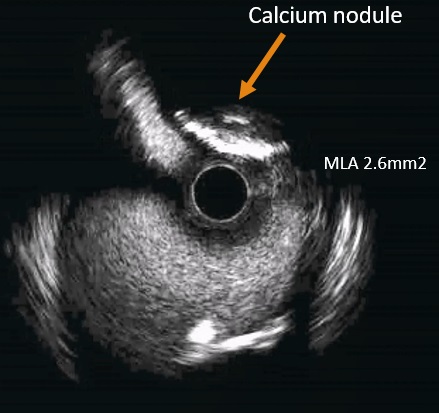
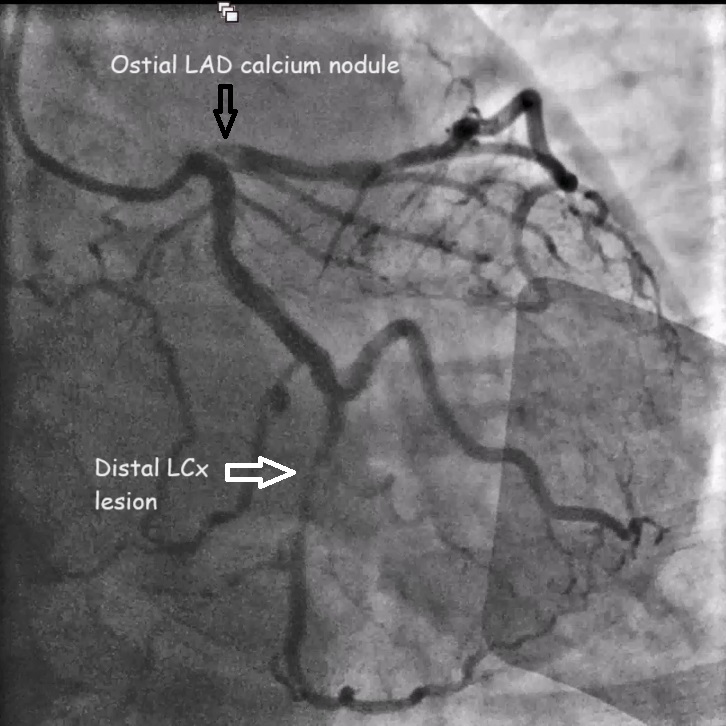
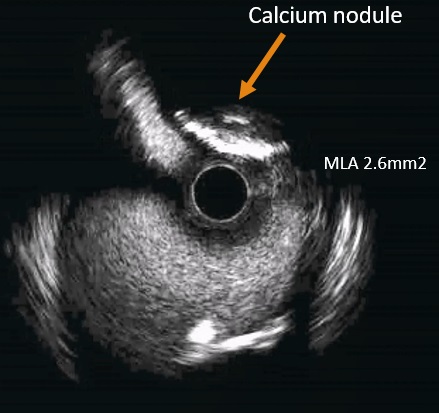
The angiogram revealed an 80% stenosis in the ostial left anterior descending artery (LAD) with a hazy appearance, and a 70% stenosis in the distal circumflex artery (Cx). Intravascular ultrasound (IVUS) confirmed a calcium nodule in the ostial LAD with a minimal lumen area (MLA) of 2.6mm². Deferment of intervention allowed for thorough patient discussion. The patient, considering advanced age, declined coronary artery bypass grafting (CABG) and opted for high-risk PCI with IABP support.
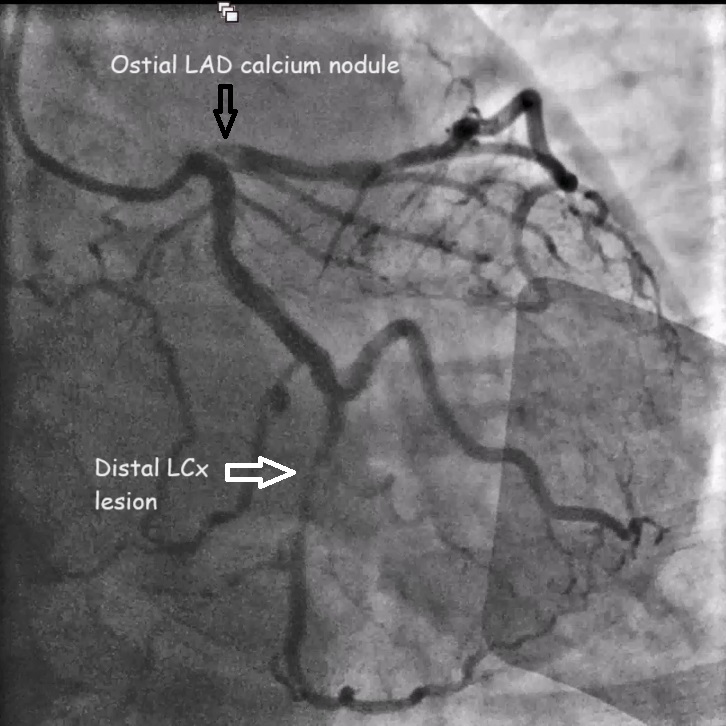


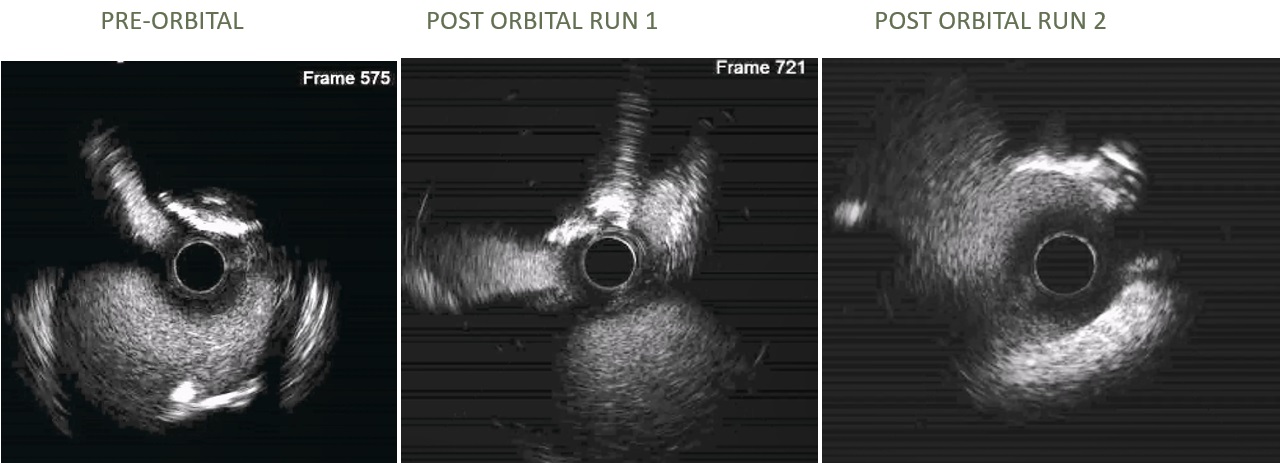
Relevant Catheterization Findings
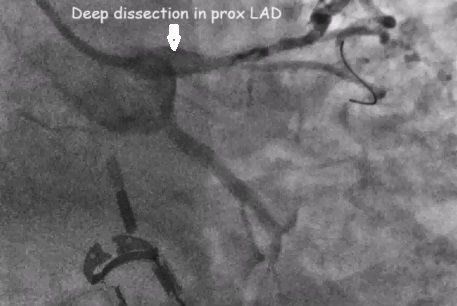
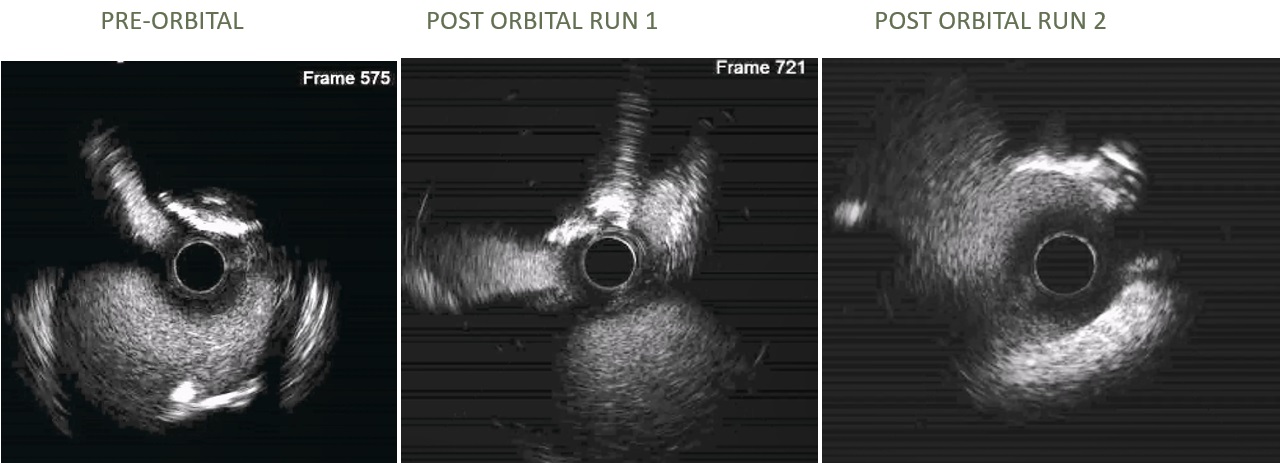
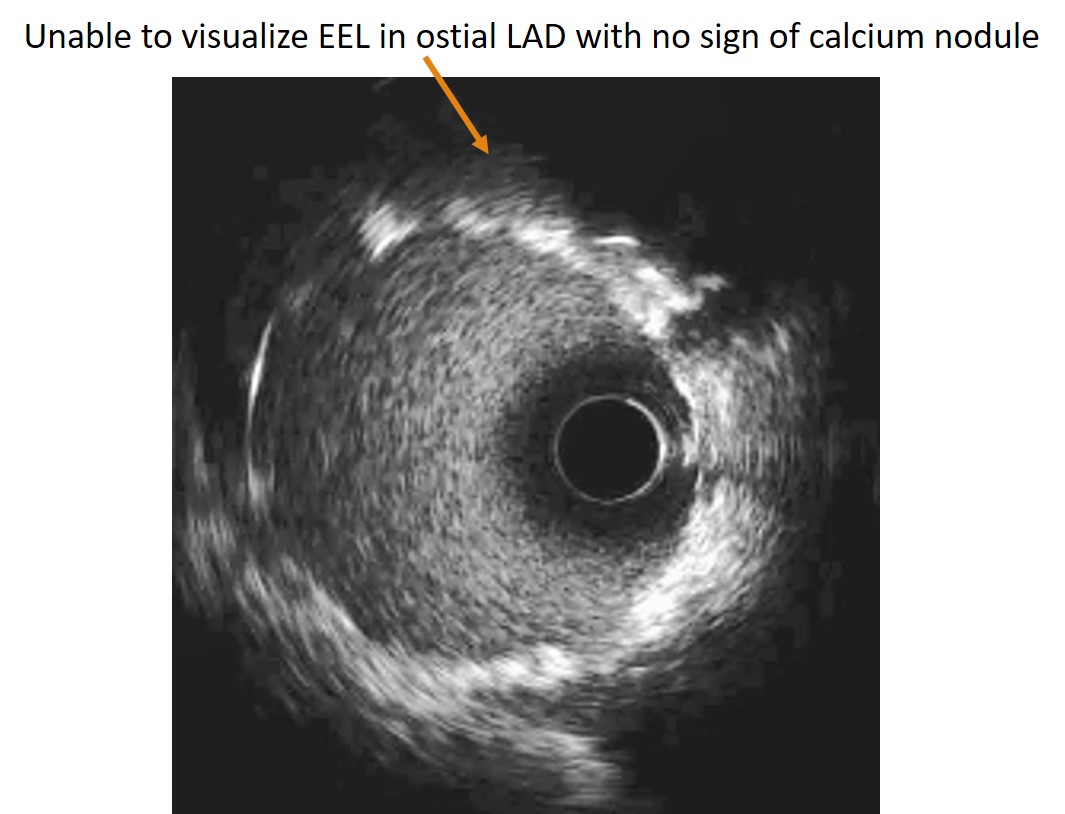
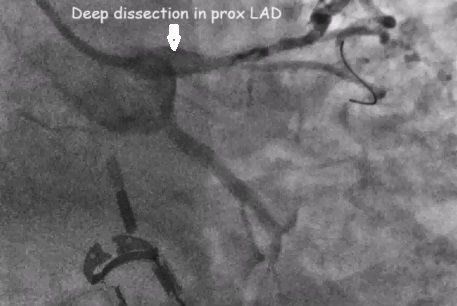
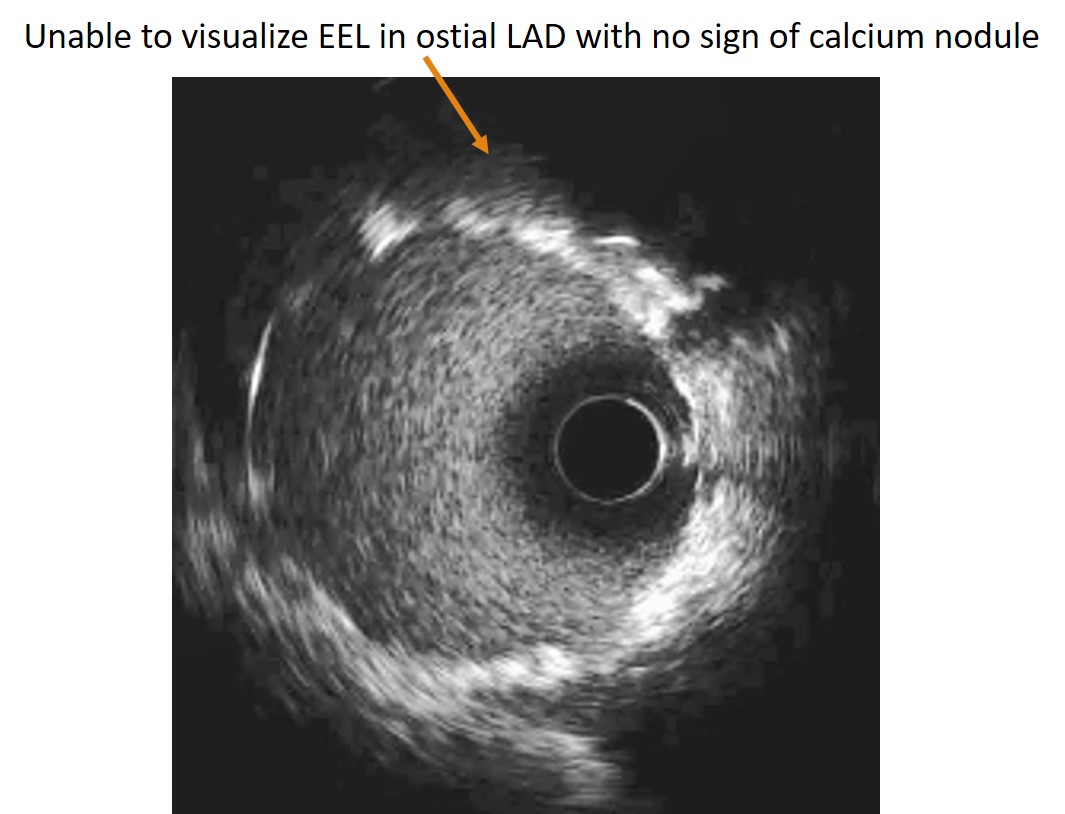
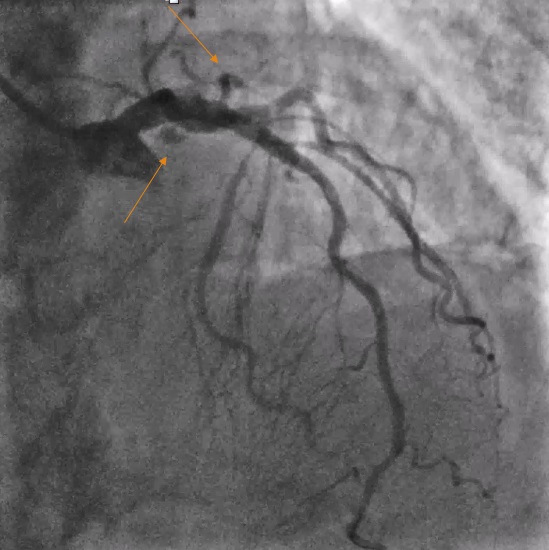
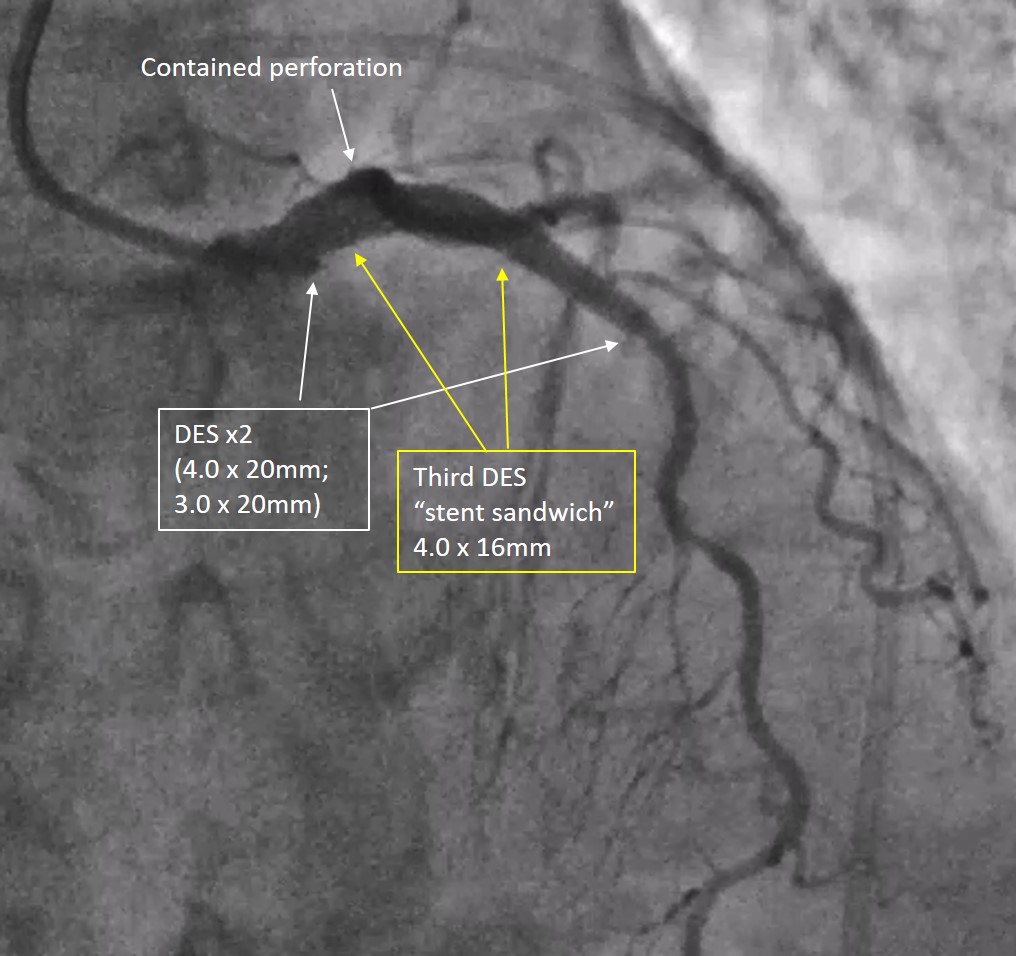
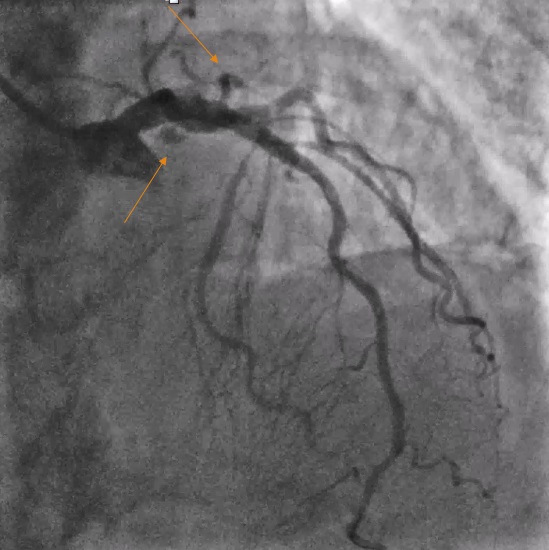
Calcium modification with orbital atherectomy, involving 3 retrograde low-speed and 1 high-speed runs, was initially performed. However, repeat IVUS indicated suboptimal modification of the calcium nodule. An additional 2 low-speed and 3 high-speed runs of orbital atherectomy were executed, resulting in good luminal gain but also a deep dissection in the proximal LAD. Two overlapping stents (4.0 x 20mm; 3.0 x 20mm) were deployed from the ostial left main to mid LAD.
Interventional Management
Procedural Step
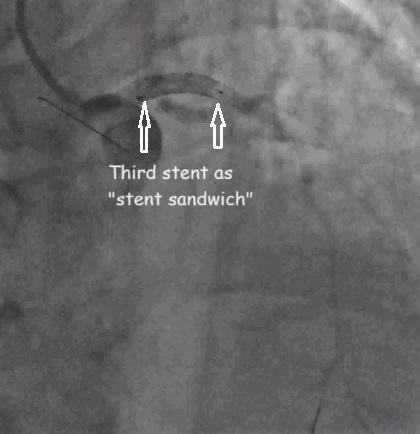
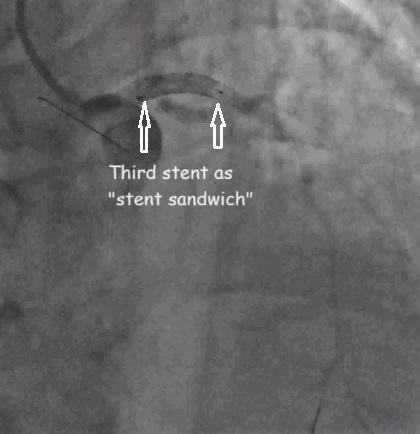
Post stenting IVUS run was unable to visualise EEL with no sign of the previously seen calcium nodule. Subsequently, an Ellis Type III perforation in the distal LM and ostial LAD emerged. A unique "stent sandwich" technique was employed, deploying a third stent (4.0 x 16mm) in mid LM-proximal LAD across both sites of perforation. This innovative approach successfully addressed the perforation, reducing it to Ellis Type I, without compromising the circumflex artery (Cx). Despite initial procedural success, the patient developed hypotension and transient pulseless electrical activity (PEA). Intubation, resuscitation, and pericardial drainage were swiftly implemented, resolving a significant pericardial effusion and tamponade physiology. Subsequent angiogram confirmed improvement to a contained perforation at the ostial LAD with IVUS imaging showing optimal stent expansion. The patient was discharged well and continued to exhibit positive outcomes at the 1-year follow-up.
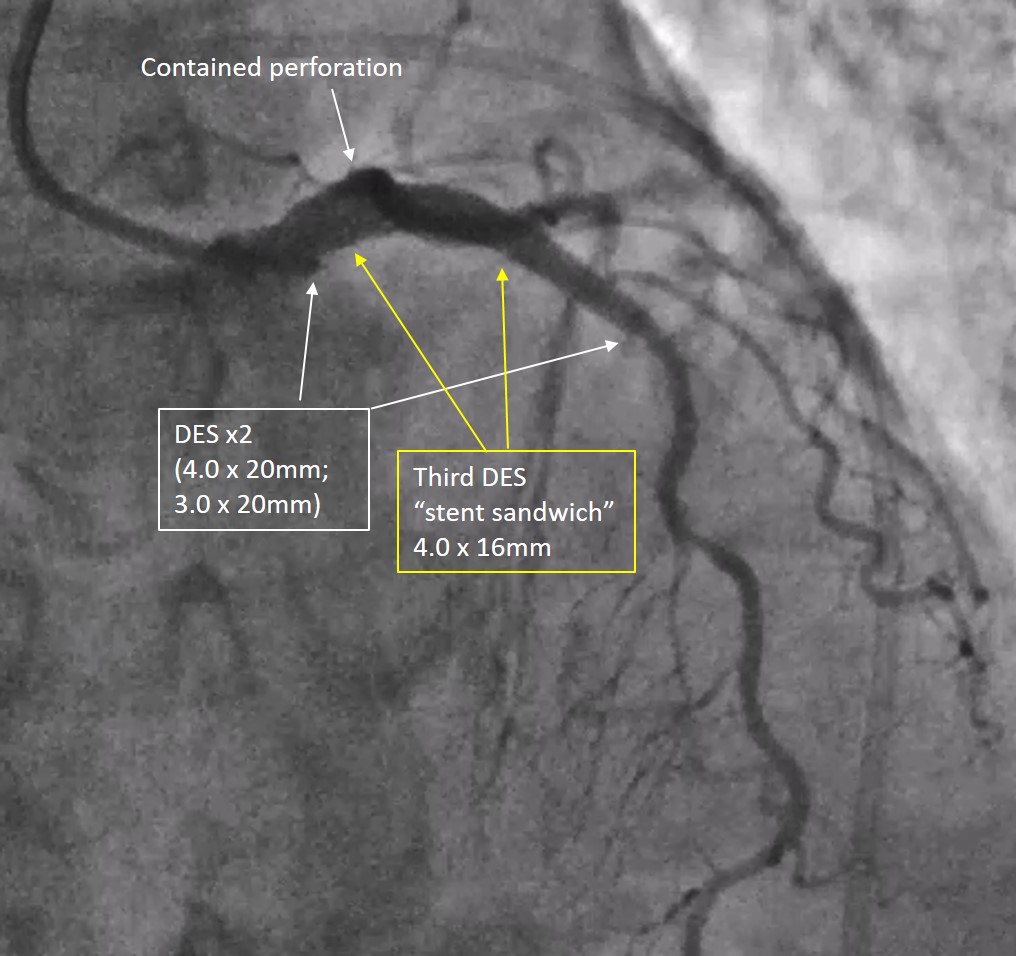
Case Summary
This case underscores the efficacy of the "stent sandwich" technique in managing a complex coronary perforation, particularly in the distal left main, showcasing its utility in preserving flow to major coronary vessels such as the circumflex artery (Cx). This technique aims to provide additional structural support and seal the perforated or dissected area. The successful outcome emphasizes the significance of adaptability and innovative strategies in high-risk interventional procedures.

