Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-219
A Challenging Case of Double Atrial Septal Defect: Used Every Tip and Trick in the Book !
By Atul Kaushik, Surender Deora, Sourabh Goswami
Presenter
Atul Kaushik
Authors
Atul Kaushik1, Surender Deora1, Sourabh Goswami1
Affiliation
All India Institute of Medical Sciences, Jodhpur, India1,
View Study Report
TCTAP C-219
Structural - Other Structural Interventions
A Challenging Case of Double Atrial Septal Defect: Used Every Tip and Trick in the Book !
Atul Kaushik1, Surender Deora1, Sourabh Goswami1
All India Institute of Medical Sciences, Jodhpur, India1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
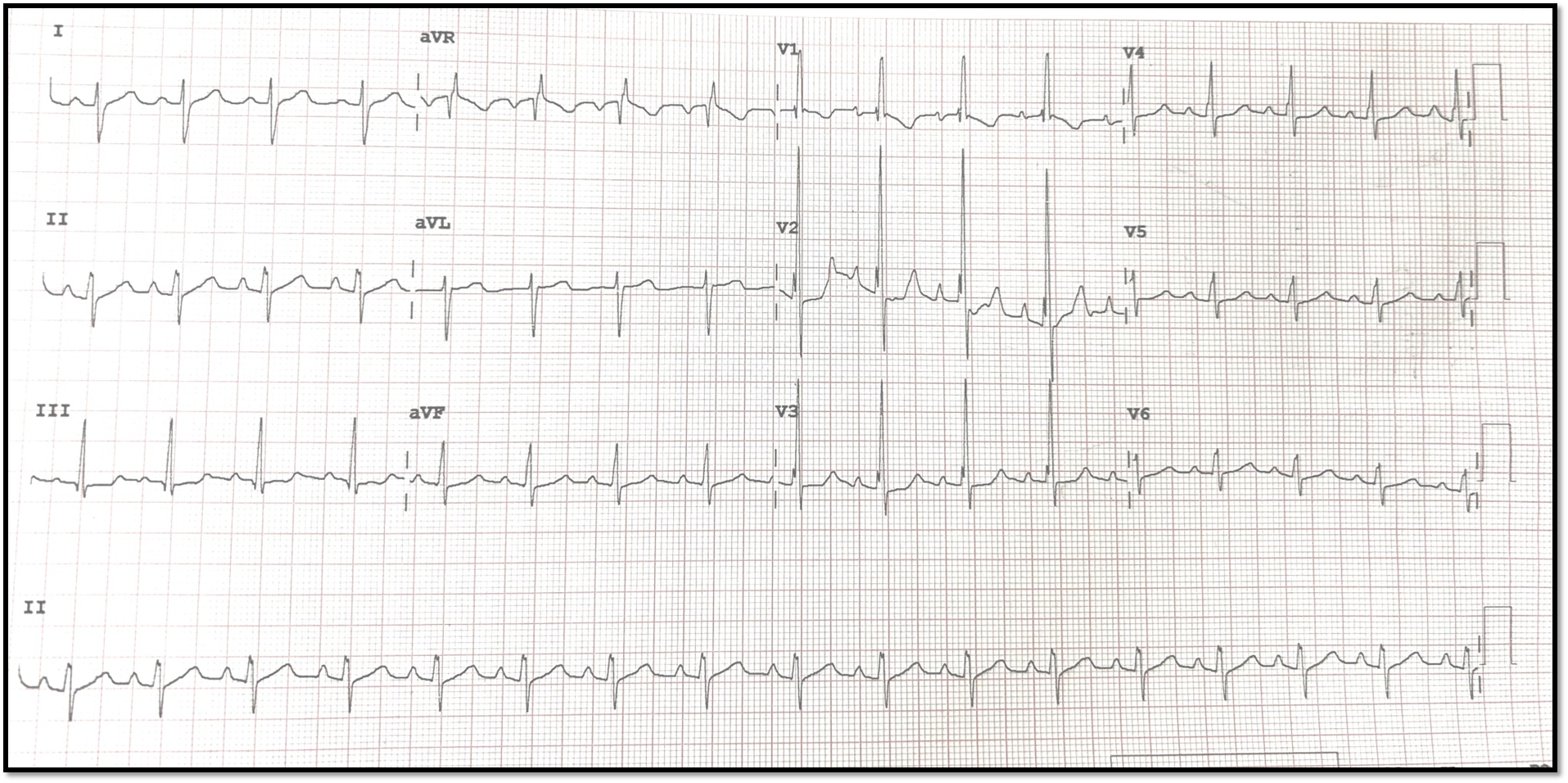
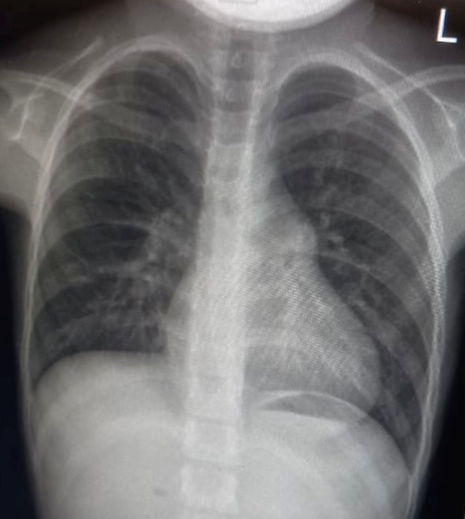
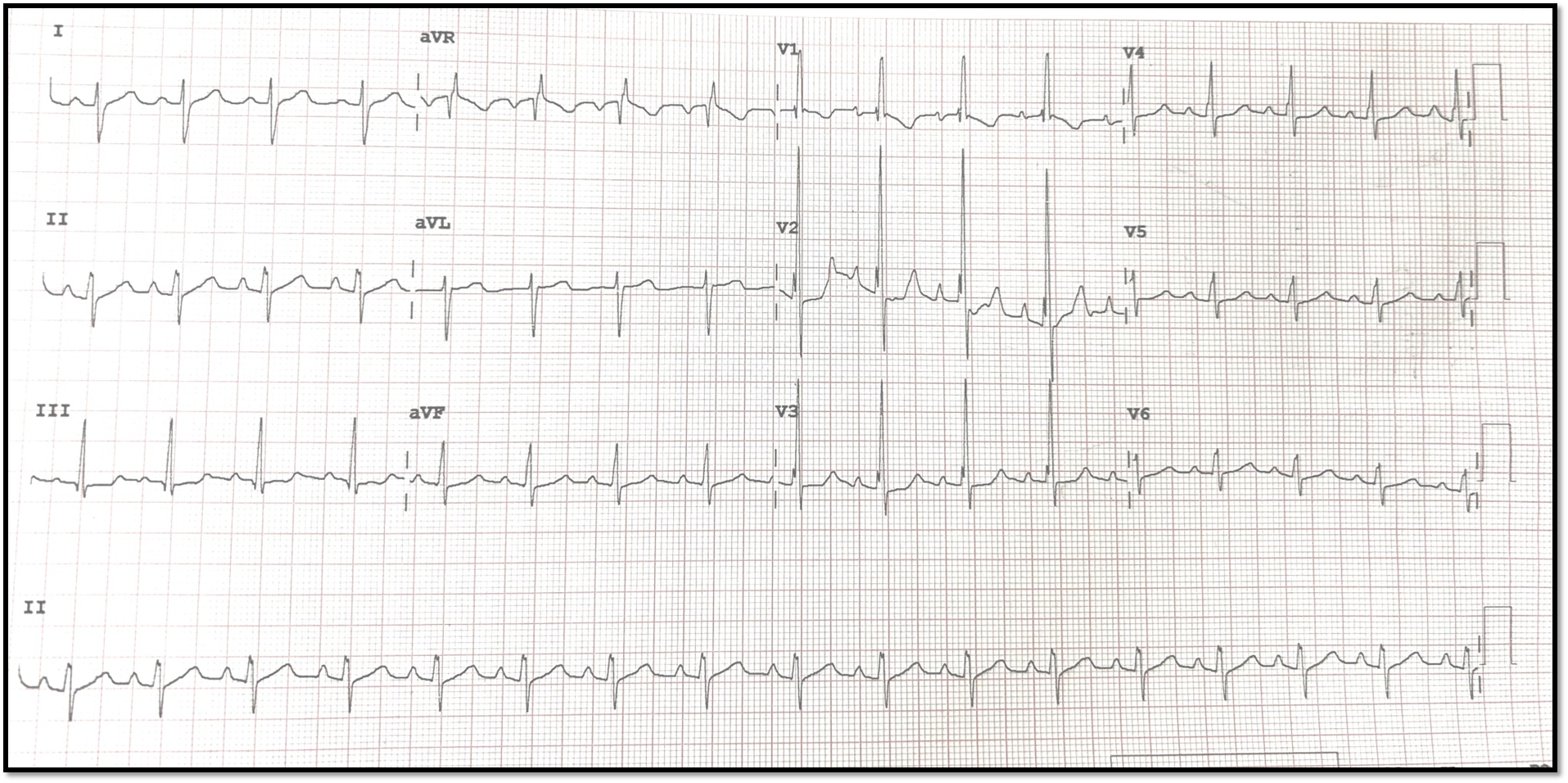
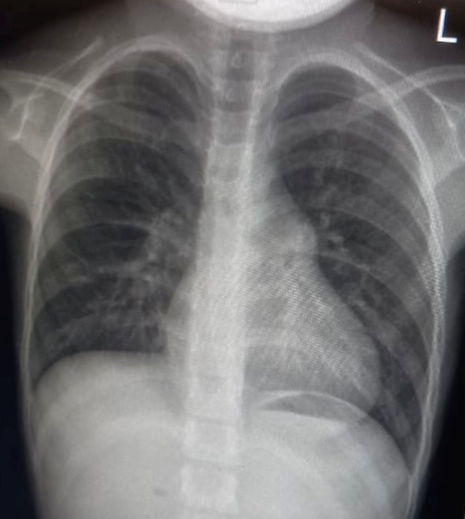
An 8-year-old girl presented with the chief complaints of dyspnea on exertion (NYHA II) for 1 year. Patient was conscious, oriented to time, place and person. BP: 98/64 mmHg. Pulse: 85/min, regular. JVP: Not raised. CVS: S1: Normal, S2: Wide and fixed spilt. Grade 2/6 Ejection Systolic murmur was heard in 2nd left intercostal space. No S3, S4. No other heart sounds. Rest of the systemic examination was unremarkable. ECG: Incomplete RBBB, CXR: No Cardiomegaly, PAH+
Relevant Test Results Prior to Catheterization
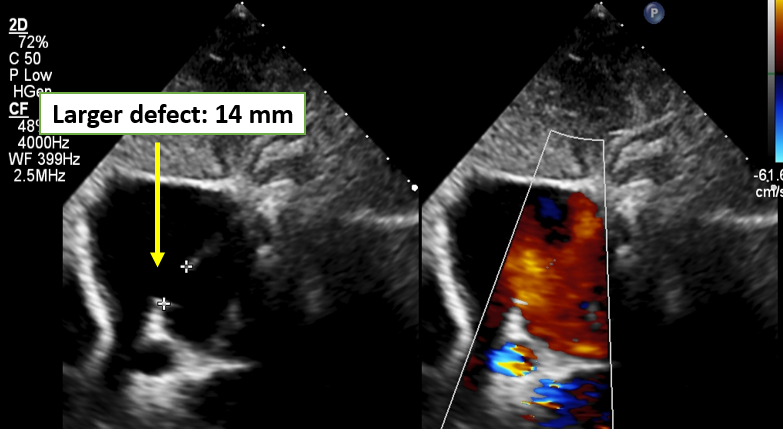
Echocardiography : Situs Solitus Levocardia, Normally related great vessels, SVC opening into RA, 4 Pulmonary vein draining into LA. Two Ostium secundum ASDs (14 mm and 9 mm){ Pic 3 and 4), > 2:1 Left to right shunt. Right atrium and right ventricle dilated. Mild tricuspid regurgitation, RVSP= 34+ RAP mm Hg, Normal Biventricular function. No PDA/VSD/CoA.


Relevant Catheterization Findings
Plan: Device Closure of the Two ASDs with two devices 18mm and 10 mm. Right heart cauterization revealed mild PAH with PASP= 39 mm Hg, RVSP= 42 mm HG, RVEDP= 3 mm Hg.
Interventional Management
Procedural Step
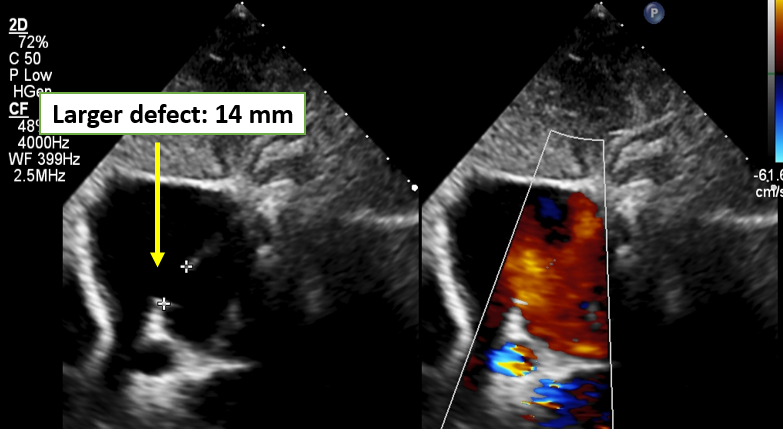
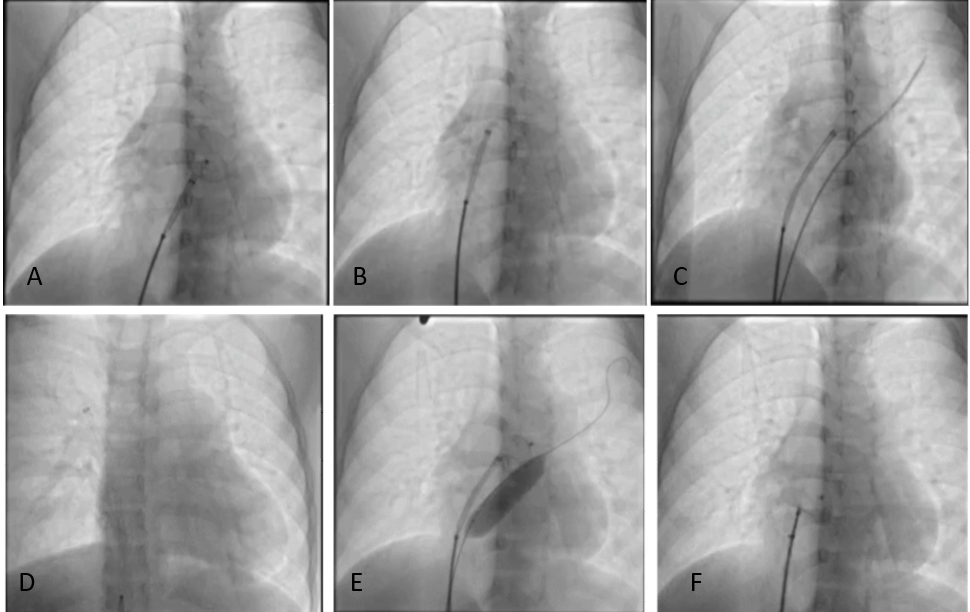
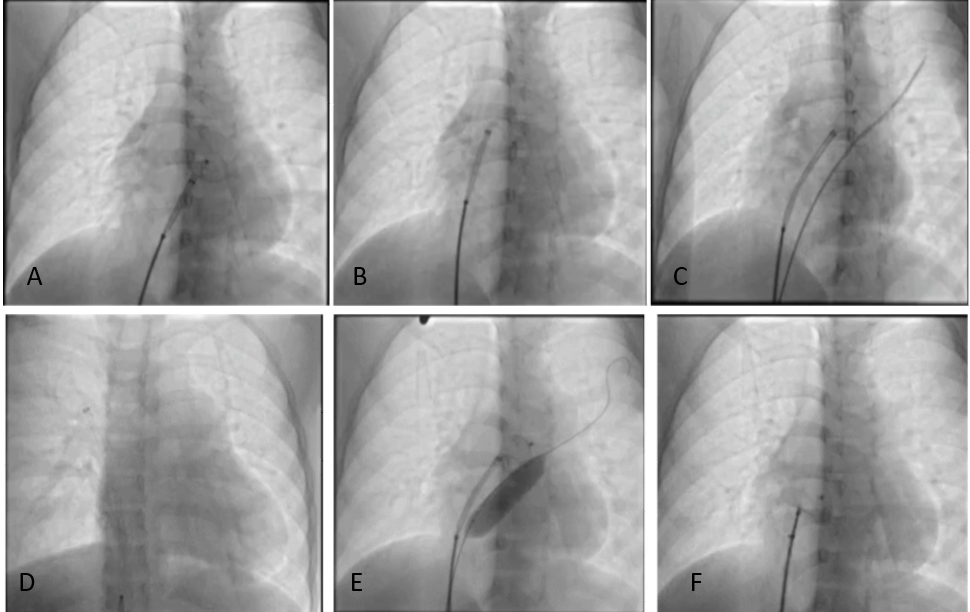
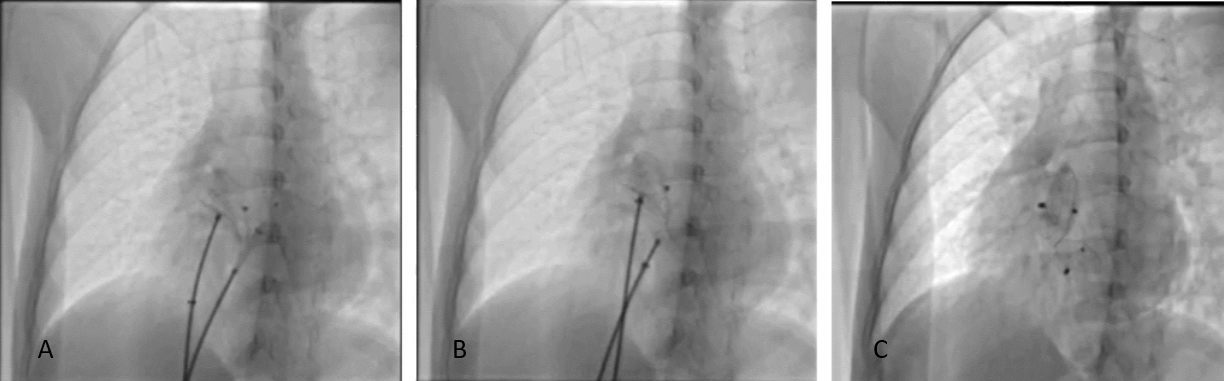
The procedure was done under general anesthesiaand Fluoroscopy and Transthoracic echocardiography (TTE) guidance. Right andleft femoral vein (FV) were accessed with 6Fr sheath. Through RFV, 6Fr MPAcatheter was introduced over 0.035”Terumo Wire and placed in LUPV. The wire was exchanged to Superstiff wire and 6FrSheath to 8Fr Mullins sheath. 18 mm ASDdevice was taken for deployment. The left disc of the device wasopened in LA and the whole system was pulled back. However, the device was notstable despite repeated attempts (Pic 5A). Then we used the technique of Guidewire Assistance((Pic 5C)) with 6Fr JR cathetersupport over amplatzar superstiff wire through left access but still the devicewas not stable. Then we used RightUpper Pulmonary Vein (RUPV) deployment (Pic 5D), however we still failed to position the device. Then, weused Balloon Assisted Technique (BAT) (Pic 5E&F) with balloon catheter (14 x40 mm) over 0.035” wire from left access. Theballoon was inflated the device was deployed first LA and then RA disc and then balloon was deflated and bothwere subsequently removed. Minnesota maneuver was done for device stability and TTE confirmed optimal device position.The smaller defect was closed with 10 mm ASD device after crossing the smaller defect through LUPV technique. After ensuring devicestability, first the smaller device was released & then larger one (Pic6).Post deployment TTE showed stable device position with no residual leak (Pic7).
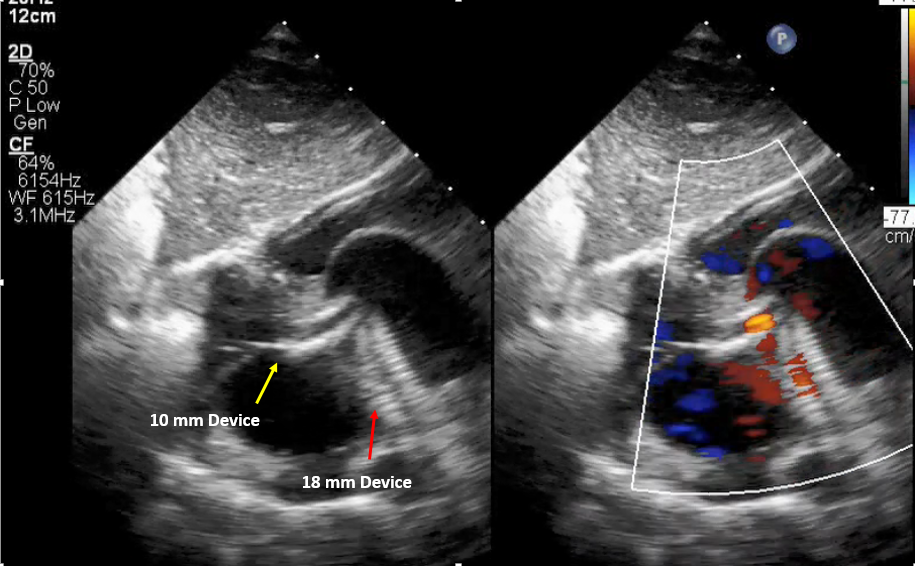
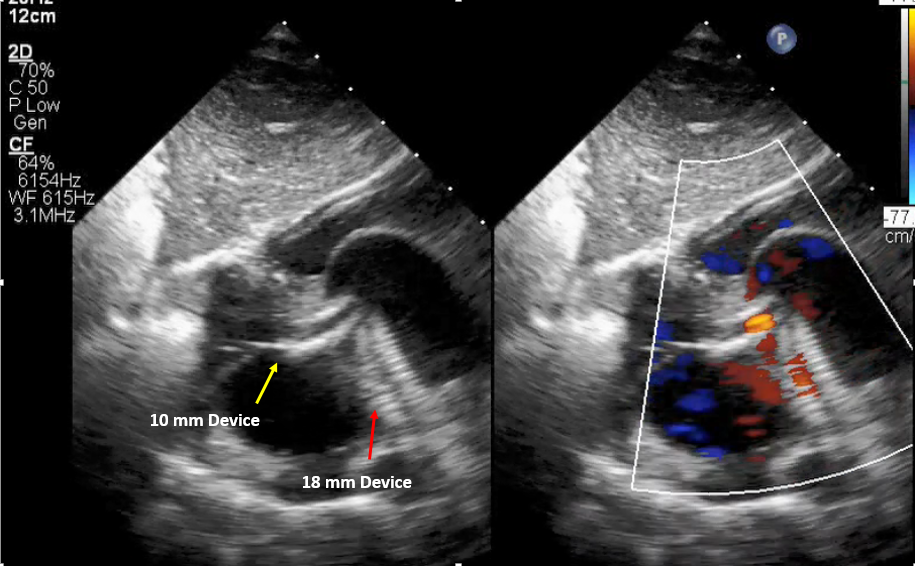
Case Summary
Transcatheter closure of multiple defects using multiple devices is feasible. Thorough preprocedural echocardiographic evaluation of defect size, adequacy of rims, number and location of defects leads to higher technical success. Two groin accesses is a commonly followed strategy for subsequent deployment with added advantage of use of assisted techniques in case of difficult anatomy. These defects may need different deployment approaches for optimum results.

