Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-076
An Imaging Guided Percutaneous Intervention to Ostial Chronic Total Occlusion of Left Anterior Descending Artery
By Chai Yih Tan, Kai Soon Liew, Huan Yean Kang, Aditya Fahmi Prianda, Yuen Hoong Phang, Kenneth Kay Leong Khoo, Kantha Rao Narasamuloo, Saravanan Krishinan, Chee Tat Liew, Dharmaraj Karthikesan
Presenter
Chai Yih Tan
Authors
Chai Yih Tan1, Kai Soon Liew1, Huan Yean Kang1, Aditya Fahmi Prianda2, Yuen Hoong Phang1, Kenneth Kay Leong Khoo1, Kantha Rao Narasamuloo1, Saravanan Krishinan3, Chee Tat Liew4, Dharmaraj Karthikesan5
Affiliation
Sultanah Bahiyah Hospital, Malaysia1, Hasna Medika Kuningan Heart Hospital, Indonesia2, Ministry of Health Malaysia, Malaysia3, Pantai Penang Hospital, Malaysia4, Hospital Sultanah Bahiyah, Malaysia5,
View Study Report
TCTAP C-076
Coronary - Complex PCI - CTO
An Imaging Guided Percutaneous Intervention to Ostial Chronic Total Occlusion of Left Anterior Descending Artery
Chai Yih Tan1, Kai Soon Liew1, Huan Yean Kang1, Aditya Fahmi Prianda2, Yuen Hoong Phang1, Kenneth Kay Leong Khoo1, Kantha Rao Narasamuloo1, Saravanan Krishinan3, Chee Tat Liew4, Dharmaraj Karthikesan5
Sultanah Bahiyah Hospital, Malaysia1, Hasna Medika Kuningan Heart Hospital, Indonesia2, Ministry of Health Malaysia, Malaysia3, Pantai Penang Hospital, Malaysia4, Hospital Sultanah Bahiyah, Malaysia5,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
The patient is a 64 years old gentleman who is known to have hypertension, dyslipidemia & history of ischaemic stroke. From 2020 to 2022, he had 3 admissions for acute coronary syndrome. Otherwise he didn’t suffer from symptoms of heart failure. On examination, he was warm and dry; jugular venous pressure was not raised; there were no pulmonary or pedal edema; precordium examination revealed heart sound 1 and 2 without cardiac murmur.
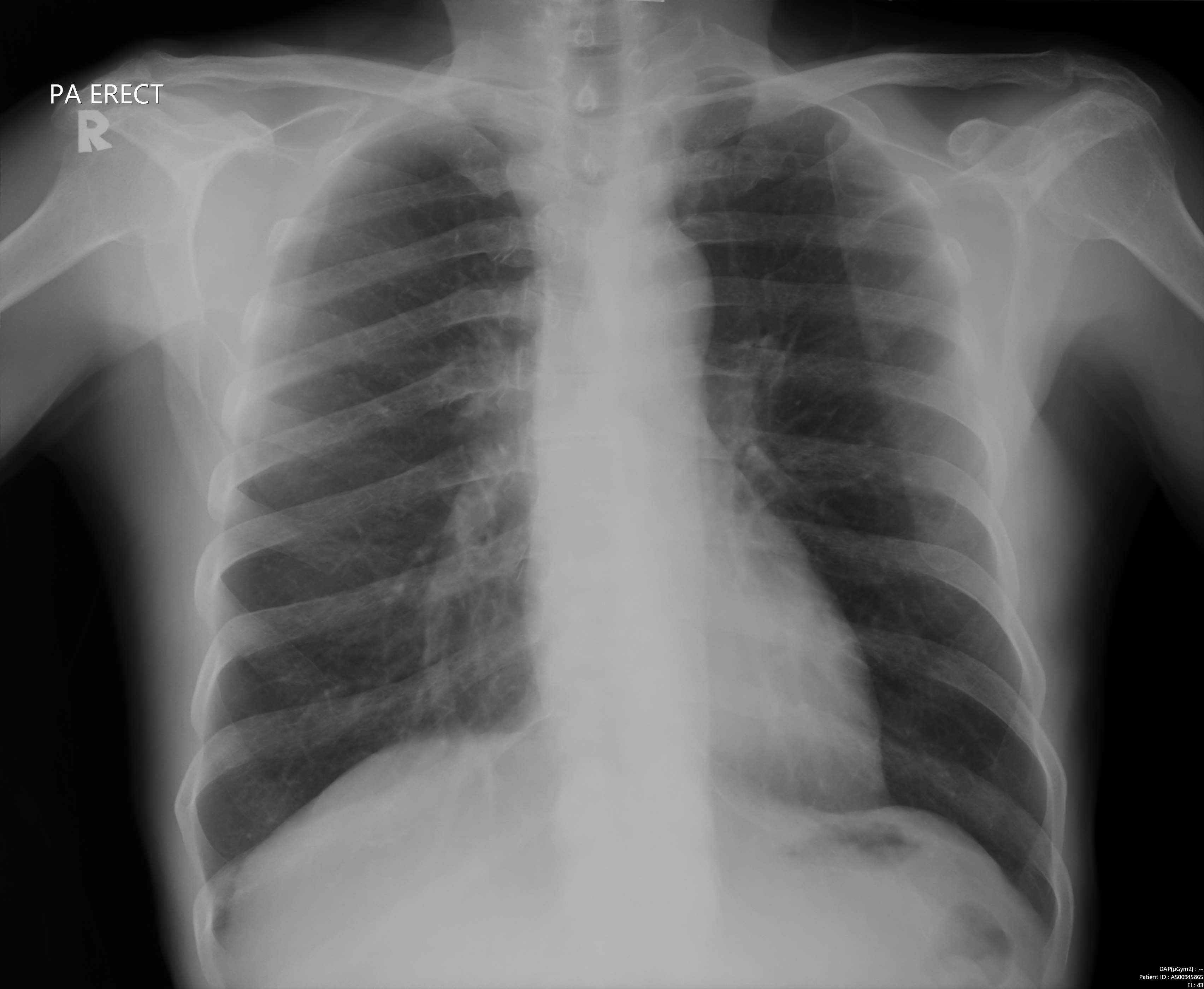
Relevant Test Results Prior to Catheterization
His baseline ECG shows sinus rhythm, normal axis, LVH with inverted T waves over leads V2-V6, I and AVL. Echocardiography showed normal chambers and valves with hypokinetic segments over the LAD territory with LVEF of 44% by Simpson’s method. This is a case of planned, stage PCI to CTO hence a cardiac MRI was ordered beforehand and viability of LAD’s myocardium is confirmed.
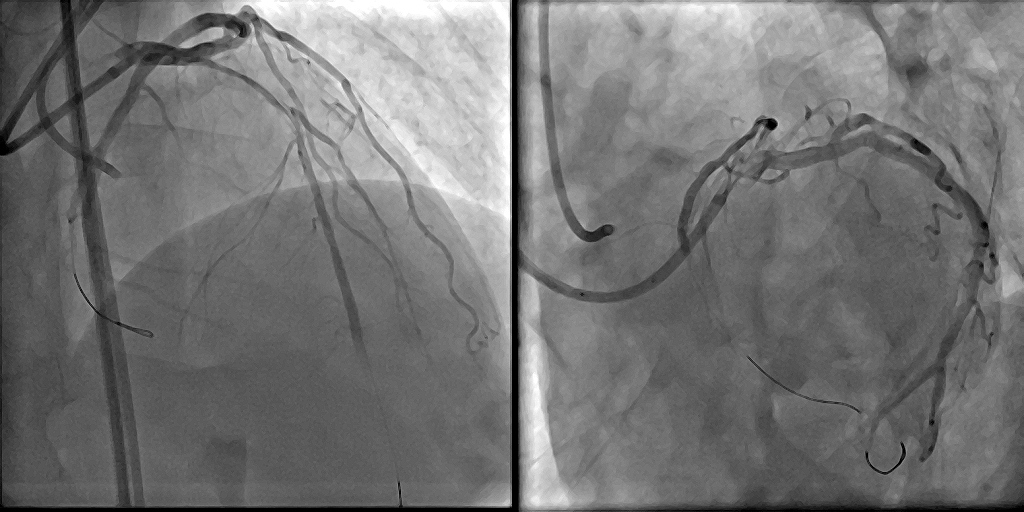
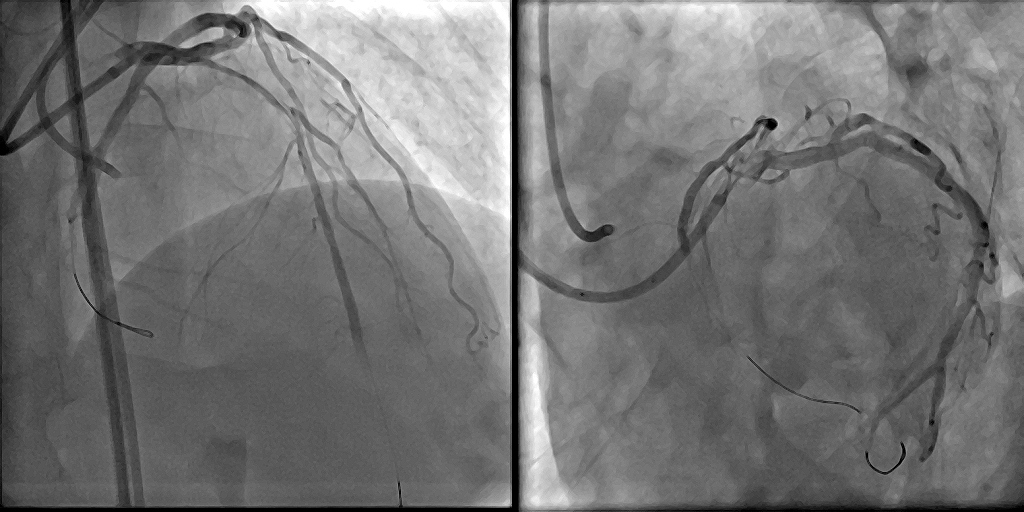
Relevant Catheterization Findings
Invasive coronary angiogram showed a left dominant system with only one CTO lesion over the proximal LAD and RCA has an anomalous origin. The segment distal to the LAD CTO is receiving collateral blood flow from RCA via Conus branch and LCx. J-CTO score for LAD lesion is 3: blunt cap, calcification and estimated length more than 20mm.




Interventional Management
Procedural Step
2 accesses were used: right femoral 7Fr with EBU 3.5 to engage left coronary system and left femoral 6Fr with AL1 to engage right coronary system for contralateral injection. At first Sion Blue wire was passed down to LCx followed by IVUS pullback to identify the stump of the CTO. Multiple attempts to puncture the proximal cap of CTO with the support of FineCross microcatheter, using wires with secondary curve including Fielder XTR, Gaia first and Conquest Pro but failed to. The initial IVUS was reviewed again and found the angle of LAD is more acute than the usual anatomy of LAD-LCx bifurcation. Subsequent attempt was done using slipstream method with Sasuke dual lumen catheter and under the guidance of IVUS, proximal CAP is punctured with Gaia 3rd wire without the secondary curve. With the same wire, the CTO lesion is crossed successfully. Wire in the true lumen was confirmed with IVUS from LCx wire for the proximal part, and contralateral injection for the distal part. The CTO lesion was predilated with a 2.0 x 15mm balloon at 6 atm and antegrade flow was restored. Fail attempts to wire the diagonal branch for protection with the help of Sasuke double lumen catheter with Sion Blue and Fielder XTR. 2nd IVUS run showed a calcified plaque in the lesion with myocardial bridging at the distal part. The lesion was further prepared with scoring balloon 3.0x20mm & cutting balloon 3.5x10mm, and treated with DCB 3.5x40mm (12atm, 3.67mm, 5 mins).

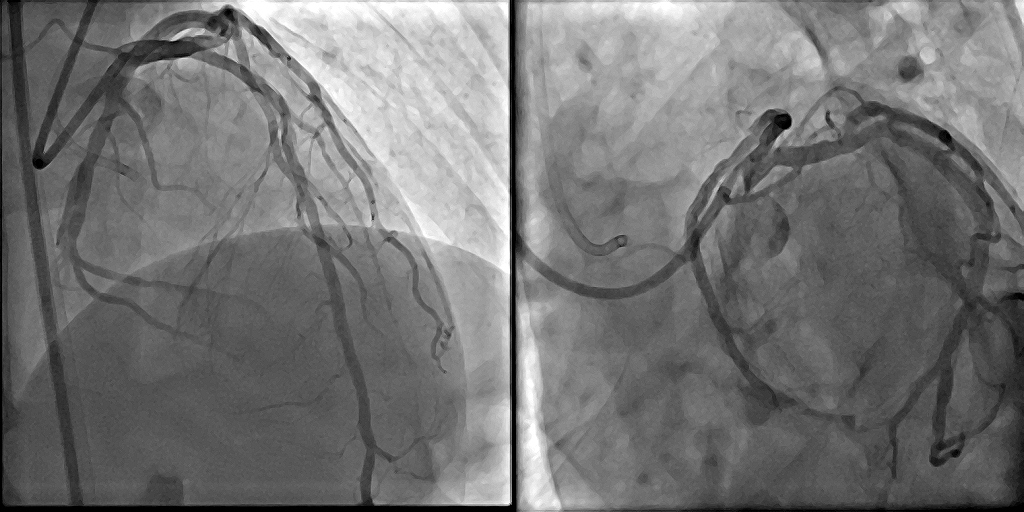

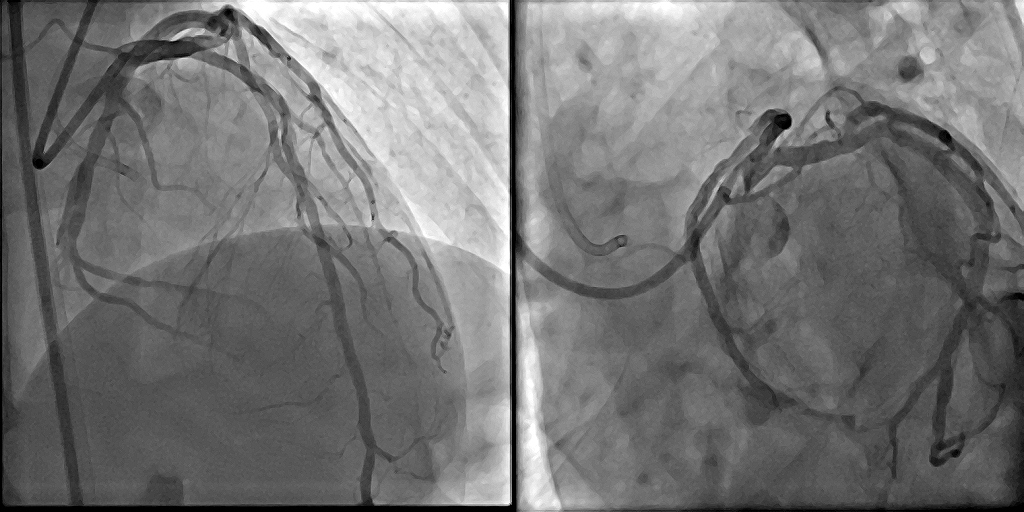
Case Summary
Antegrade approach was chosen because of the tortuous and small epicardial collateral from RCA and LCx. IVUS played a pivotal role in identifying the proximal cap of ostial CTO & assessing the branch’s angle. With the slip stream technique, it allows direct intracoronary visualization of proximal cap puncture & increases the support for the wire. Due to the acute angle of the LAD branch, the puncture to the proximal cap was made possible without a secondary curve to increase the stiffness . The treatment with DCB is to avoid jailing of diagonal branch, impingement of LCx, incomplete coverage of ostial lesion and undersizing of LMS lumen in LMS-LAD stenting.

