Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-003
Now You See It, Now You Don't
By Siew Hoon Ong, Aslannif Roslan
Presenter
Siew Hoon Ong
Authors
Siew Hoon Ong1, Aslannif Roslan1
Affiliation
National Heart Institute, Malaysia1,
View Study Report
TCTAP C-003
Coronary - ACS/AMI
Now You See It, Now You Don't
Siew Hoon Ong1, Aslannif Roslan1
National Heart Institute, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
70 year old man, active smoker and known hypertensive, hyperlipidemia presented to a primary care hospital 1 month ago with reduced effort tolerance for 1 week. ECG showed late presentation inferior myocardial infarction changes and he was treated with dual antiplatelet and low molecular weight heparin. He was referred to our center for further management.
On review he was NYHA class II with no significant physical findings. ECG showed Q waves and T inversion in inferior leads.

On review he was NYHA class II with no significant physical findings. ECG showed Q waves and T inversion in inferior leads.

Relevant Test Results Prior to Catheterization
BP 144/68pulse 68 bpm regularlungs clearCVS dual rhythm no murmur
ECHO:LVEF 49%, dilated Left ventricle (LVIDd 5.77cm)Hypokinetic posterior, inferior and septal areaincreased septal thickness IVSd 1.15cmmild aortic and mitral regurgitation
Chest X ray: cardiomegaly

ECHO:LVEF 49%, dilated Left ventricle (LVIDd 5.77cm)Hypokinetic posterior, inferior and septal areaincreased septal thickness IVSd 1.15cmmild aortic and mitral regurgitation
Chest X ray: cardiomegaly

Relevant Catheterization Findings
Left main: normalLeft anterior descending artery: normal
Left circumflex artery: normal, giving faint retrogrades to right coronary territoryRight coronary artery: totally occluded mid RCA
Left circumflex artery: normal, giving faint retrogrades to right coronary territoryRight coronary artery: totally occluded mid RCA
Interventional Management
Procedural Step
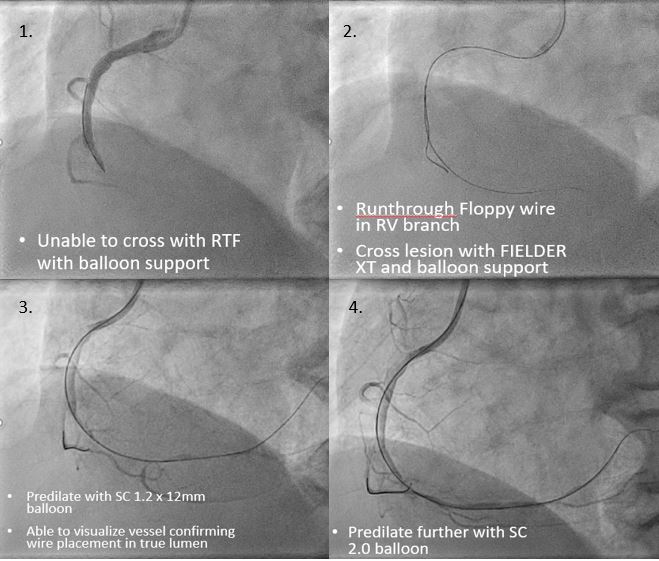
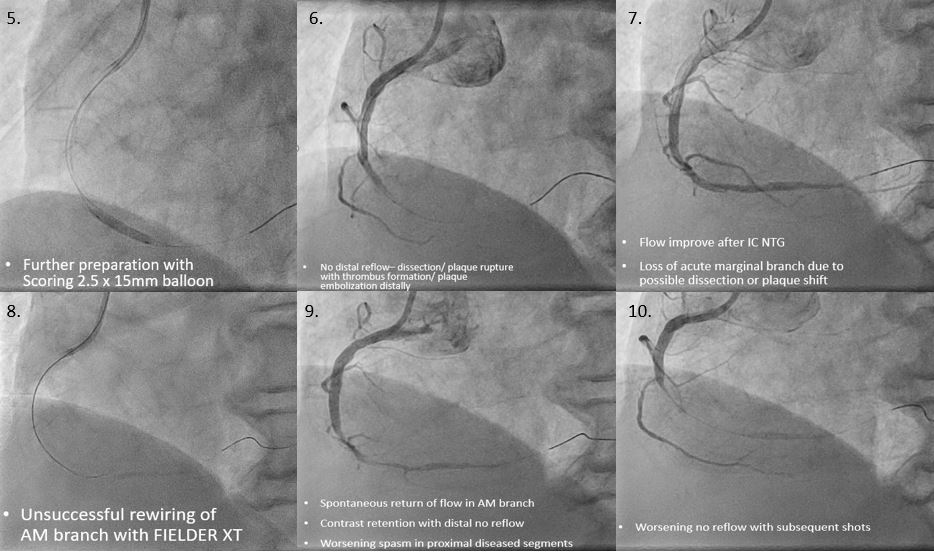
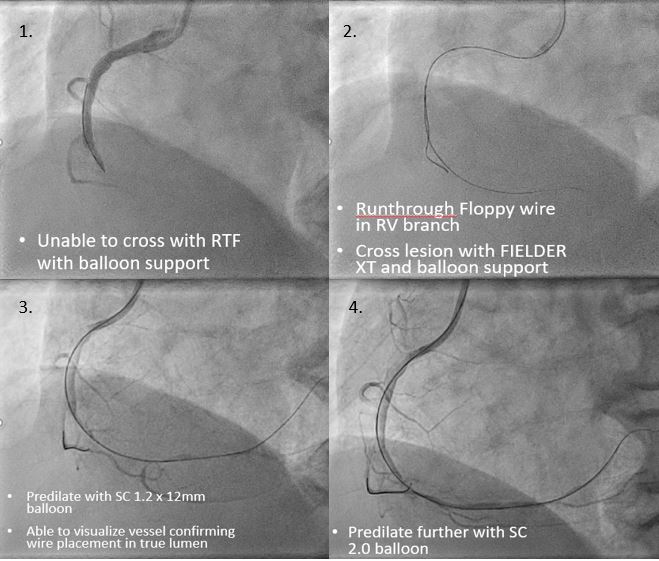
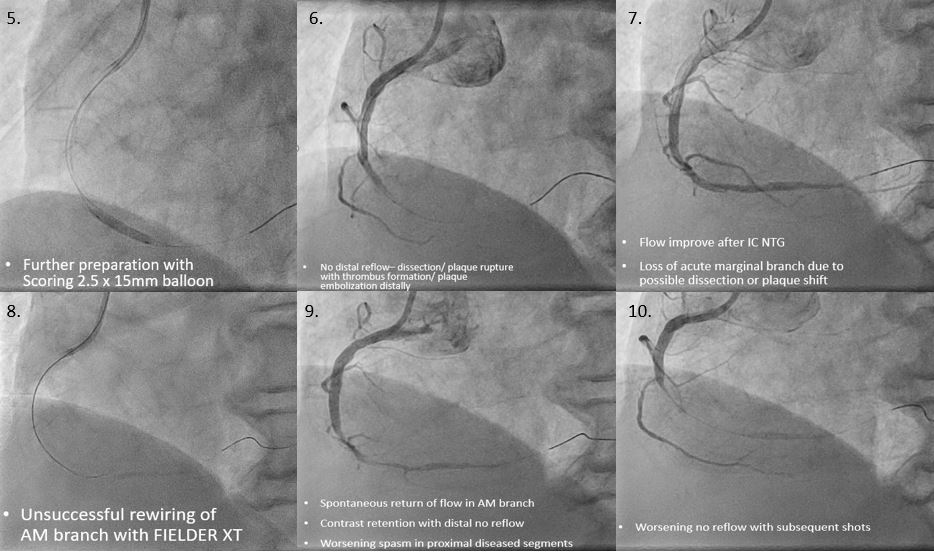
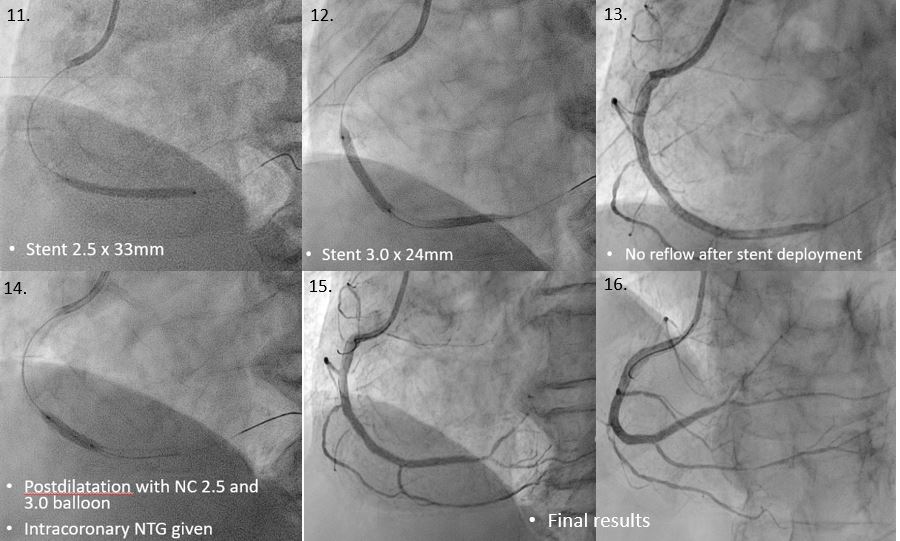
PCI to RCA was attempted with JR 3.5 guide and Runthrough Floppy wire but unable to cross lesion. Lesion was successfully crossed using a FIELDER-XT wire with 2.0 SC balloon support, with RTF wire giving extra support in RV branch.2.0 SC balloon was unable to cross tightest lesion hence predilation was done with SC 1.2 x 12mm balloon. Contrast injection confirmed position of wire in true lumen.Further predilatation with SC 2.0 balloon showed improved vessel expansion. Scoring NC 2.5 balloon predilatation was then done. After scoring balloon predilatation, no-reflow occurred from mid to distal RCA; flow improved after IC NTG but Acute Marginal branch was lost. Attempts to rewire the branch with FIELDER-XT was unsuccessful. There was transient improvement of perfusion in the branch, however subsequent shots showed worsening distal no reflow and we decided to proceed with stenting. Unfortunately due to technical issues IVUS was not available for this case.Distal RCA was stented with 2.5 x 33mm to cover possible distal dissections, followed by another 3.0 x 24mm stent covering the proximal disease segment. Following stenting, distal no reflow persisted; flow improved after postdilatation and IC NTG.Final results showed TIMI III flow with no dissections or complications.
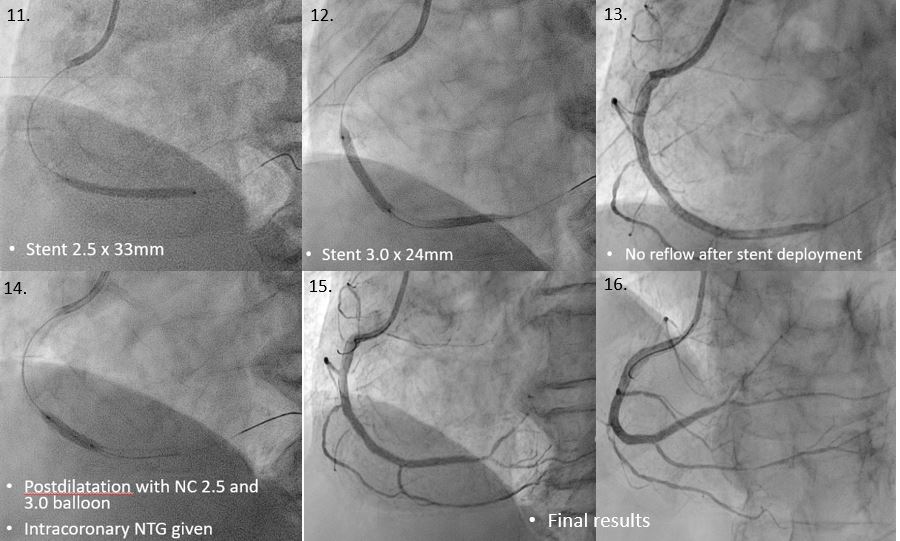
Case Summary
This patient had delayed presentation inferior MI one month ago and likely has organized thrombus and preexisting unstable heavy plaque burden. Repeated plaque modification causes disturbance to the unstable plaque, resulting in no reflow due to vessel dissection, plaque rupture with thrombus formation or distal embolization of atheromatous material into the distal vascular bed. Prompt stenting and intracoronary vasodilatation with NTG improved coronary flow and gave a favorable outcome. As in primary PCI, aggressive plaque modification should be avoided in such lesions. Intracoronary imaging with IVUS or OCT will be invaluable to assess plaque morphology and guide further management.

