Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-081
The Last Resort for Frequent In-Stent Restenosis
By Keisuke Nakabayashi, Takeshi Sasaki, Taro Takeyama, Nobuhito Kaneko, Hiroshi Ando
Presenter
Keisuke Nakabayashi
Authors
Keisuke Nakabayashi1, Takeshi Sasaki1, Taro Takeyama2, Nobuhito Kaneko1, Hiroshi Ando1
Affiliation
Kasukabe Chuo General Hospital, Japan1, Dokkyo Medical University Saitama Medical Center, Japan2,
View Study Report
TCTAP C-081
Coronary - Complex PCI - In-Stent Restenosis
The Last Resort for Frequent In-Stent Restenosis
Keisuke Nakabayashi1, Takeshi Sasaki1, Taro Takeyama2, Nobuhito Kaneko1, Hiroshi Ando1
Kasukabe Chuo General Hospital, Japan1, Dokkyo Medical University Saitama Medical Center, Japan2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
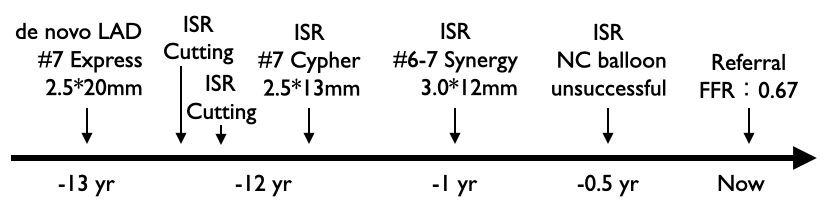
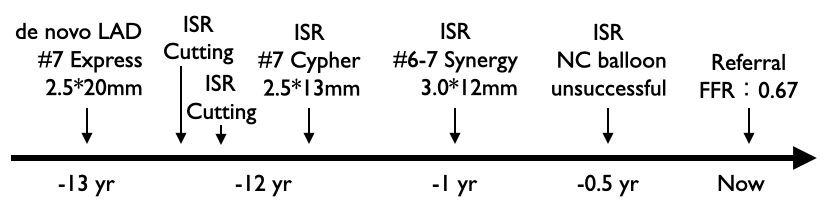
A 72-year-old man with exertional chest pain was transferred to our hospital. He had undergone the implantation of a bare metal stent and two drug-eluting stent in his left anterior descending artery (LAD) 13, 12 and 1 years before the current admission, respectively. He had experienced several episodes of in-stent restenosis (ISR). Finally, plain old balloon angioplasty (POBA) had failed with an apparent balloon indentation a month prior to this admission at the previous hospital.
Relevant Test Results Prior to Catheterization
Electrocardiogram: Sinus rhythm, heart rate of 62 beats, complete right bundle branch block.
Relevant Catheterization Findings
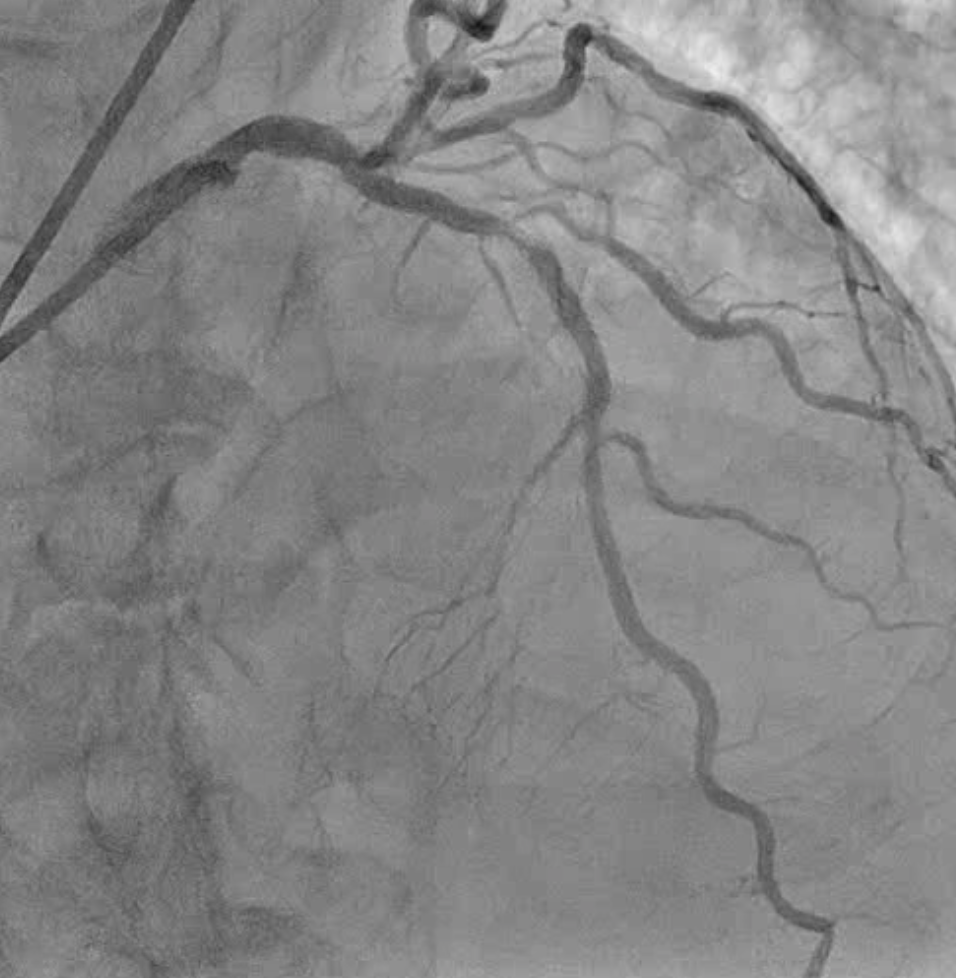
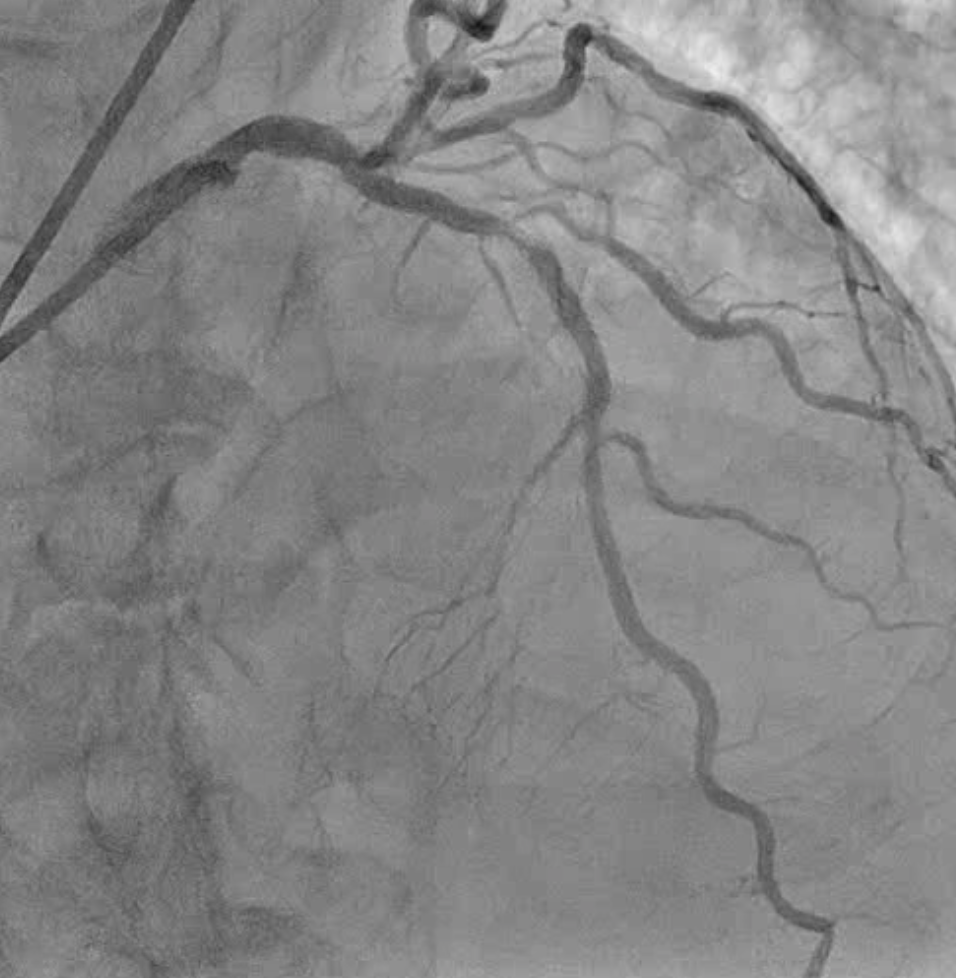
Initial angiography showed severe ISR in the LAD with a fractional flow reserve of 0.67 measured at the previous hospital. We also observed significant stenosis in the middle LAD, with obvious angiographic evidence of stent under-expansion.


Interventional Management
Procedural Step
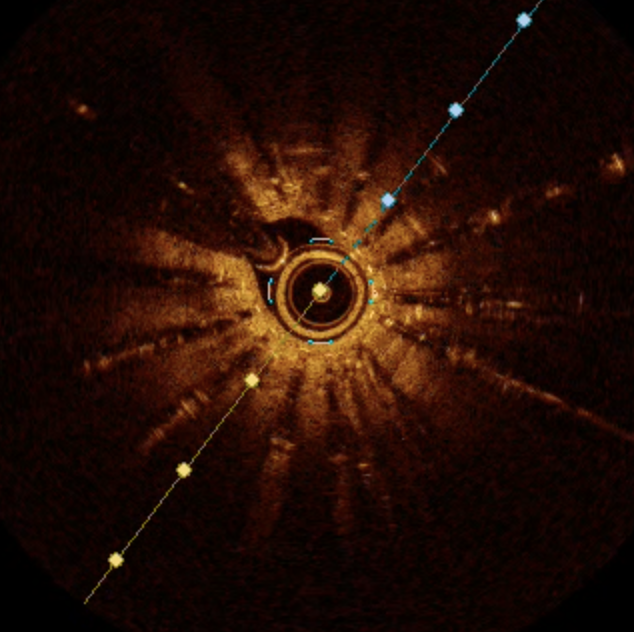
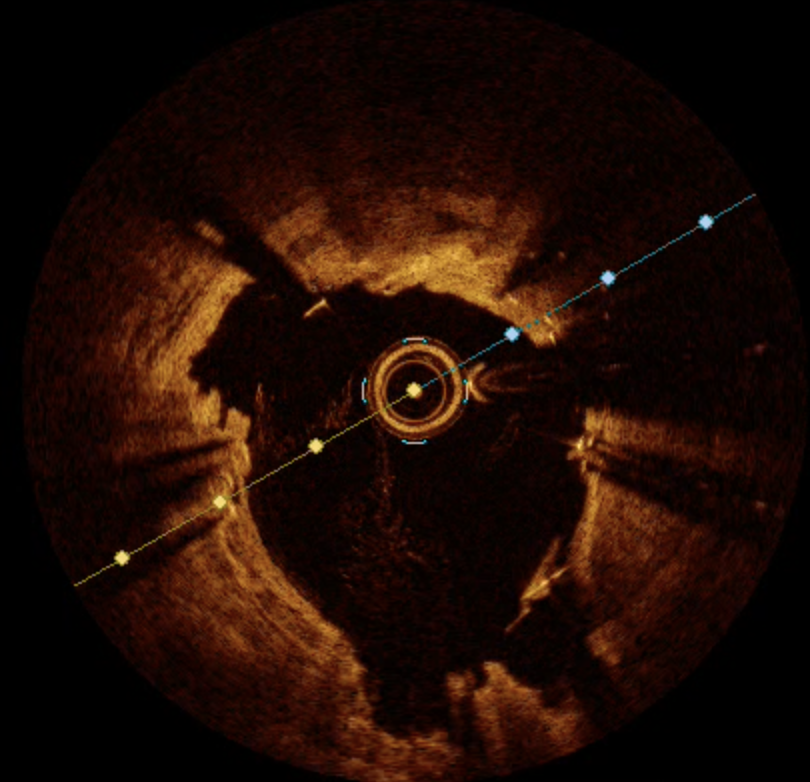
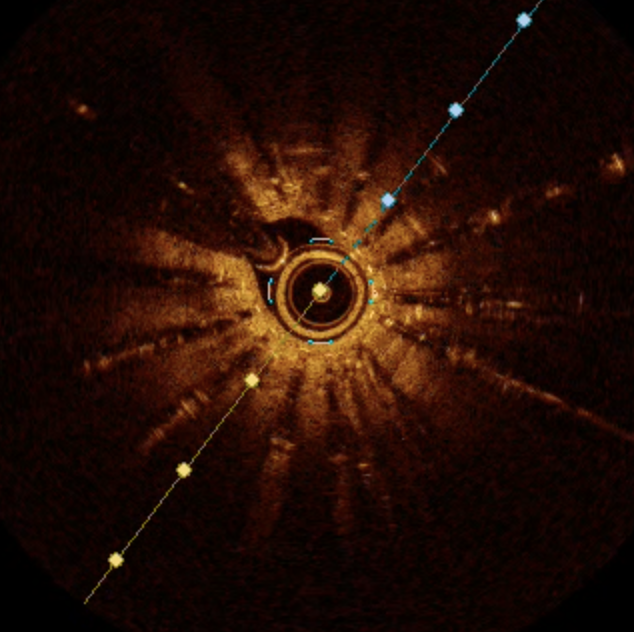
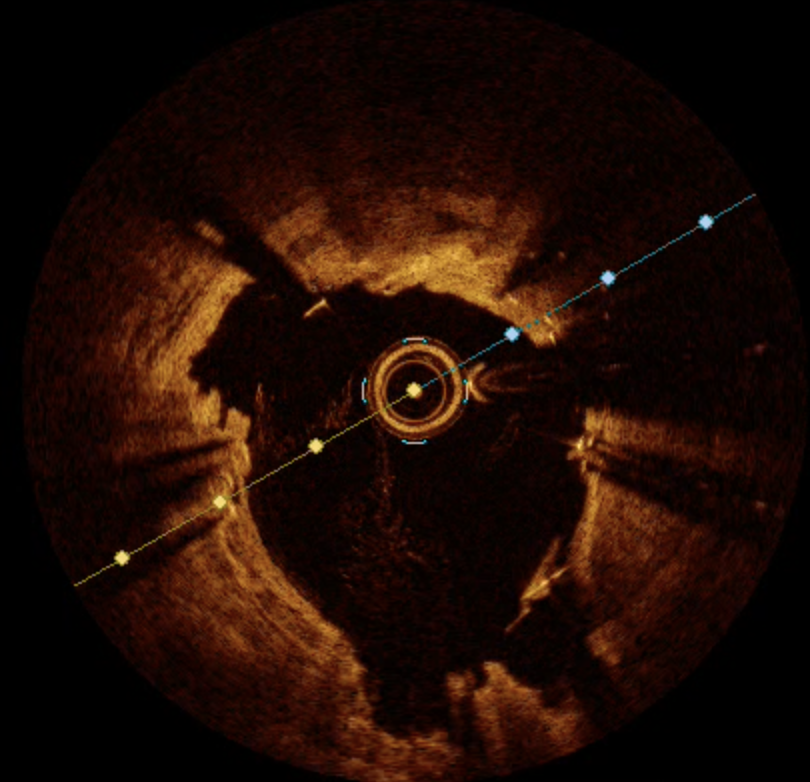
Following the unsuccessful POBA, it was decided that additional interventions were necessary. Optical coherence tomography (OCT) revealed that the target lesion was not due to new intimal calcification but was primarily a result of poor stent expansion and calcification beneath the stents. Consequently, we opted for excimer laser coronary angioplasty (ELCA, X-80, USA, Spectranetics) without saline flushing technique at 80 J and 80 Hz, to modify the calcium-plaque located beneath the stents and to increase the output power. Subsequently, we dilated the lesion with 3.0 mm non-compliant balloon at nominal pressure and up to 30 atm, eliminating the balloon indentation. Finally, a drug-coated balloon was applied. OCT confirmed sufficient stent expansion and the successful cracking of calcification beneath the previously implanted stents. The final angiography showed no residual stenosis. Two years after this procedure, the patient remained asymptomatic.


Case Summary
Stent under-expansion is a significant factor contributing to ISR. However, stent under-expansion can sometimes occur due to the presence of underestimated hard plaque. ELCA is a unique modality for modifying hard plaque beneath stents through photochemical, photothermal, and photomechanical effects. A study demonstrated that ELCA for ISR was associated with a larger final minimum lumen area and a greater stent area compared to previously implanted stents, potentially breaking the vicious circle. Although saline flushing with ELCA led to a lower incidence of coronary dissection, the non-flushing technique could enhance the effect when appropriately indicated, as in the case of ISR.

