Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-090
Navigating Complexity: Managing Left Main Trifurcation Lesion With Stent Protrusion into Aorta
By Kay Powpuree, Viroon Likitlertlum
Presenter
Kay Powpuree
Authors
Kay Powpuree1, Viroon Likitlertlum1
Affiliation
Rajavithi Hospital, Thailand1,
View Study Report
TCTAP C-090
Coronary - Complex PCI - Left main
Navigating Complexity: Managing Left Main Trifurcation Lesion With Stent Protrusion into Aorta
Kay Powpuree1, Viroon Likitlertlum1
Rajavithi Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
Thai male 62 years old presenting at emergency department with acute onset retro-sternal chest pain at rest 4 hours prior to hospital.


Relevant Test Results Prior to Catheterization
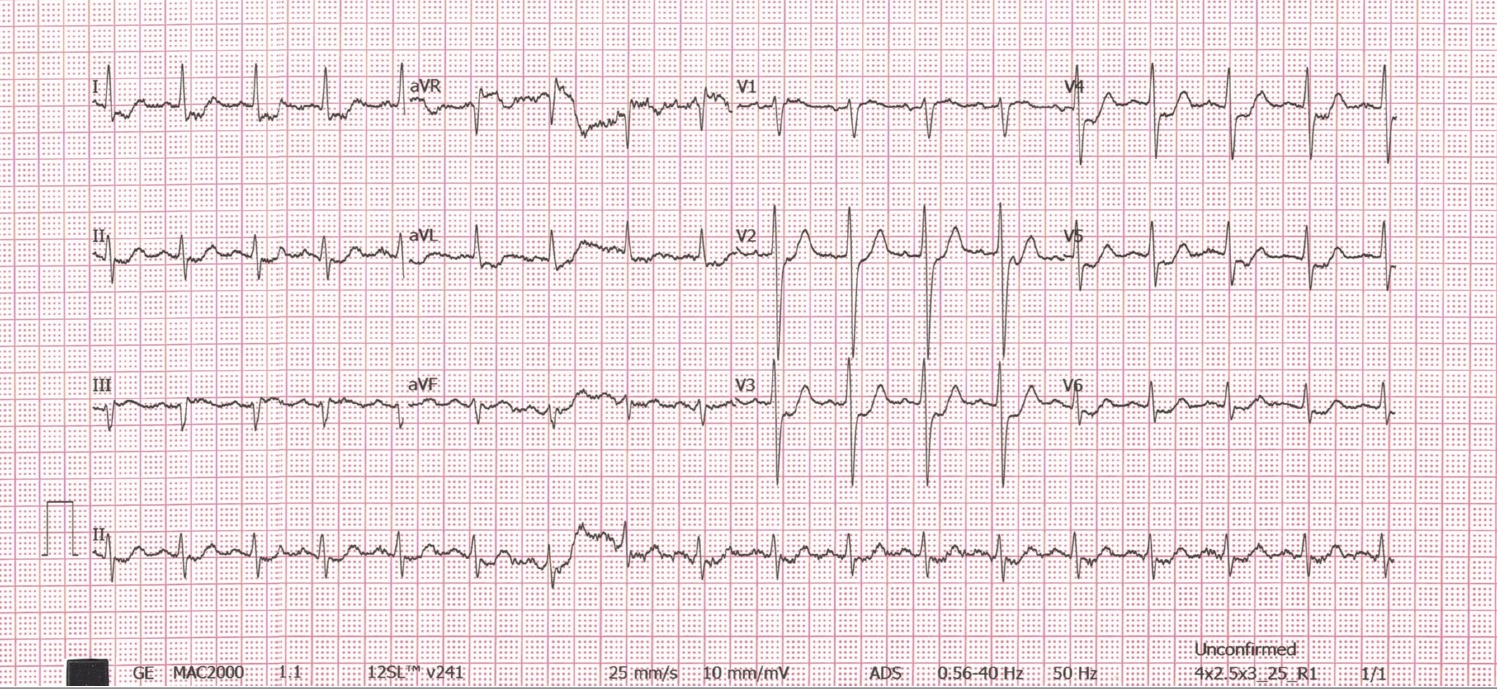
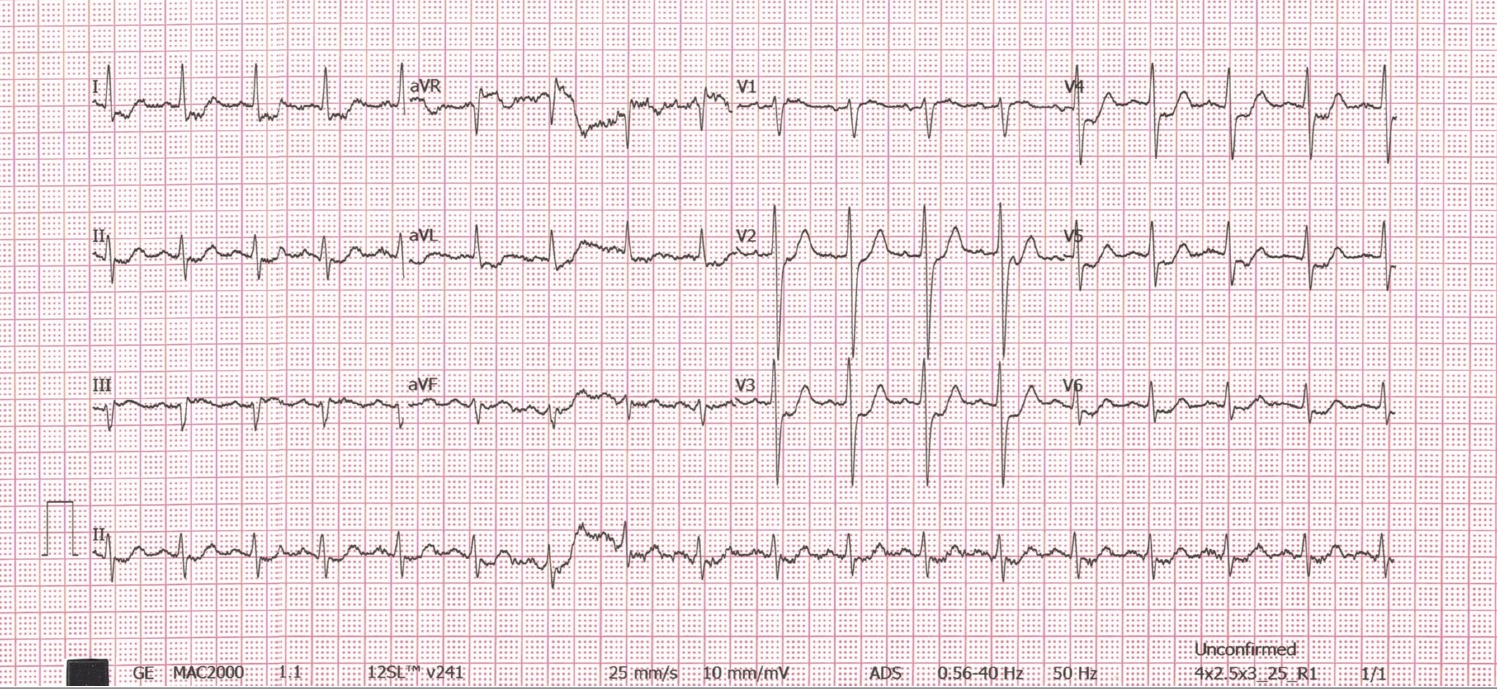
EKG was shown Sinus rhythm diffuse ST depression in lead I, II, avL, V2-V6, ST elevation in lead aVRCXR: Normal cardiac contour without lung infiltration or congestionLab: Troponin I 2568 ng/dl, Hb 13 g/dl, Platelet 210,000/ml, INR1.1 Creatinine 0.75 mg/dlEchocardiography: Good LV systolic function (LVEF 67%), Hypokinesia at basal to mid segment of inferior wall, no significant valvular abnormalities, no pericardial effusion, no Aortic root dissection was detected
Relevant Catheterization Findings
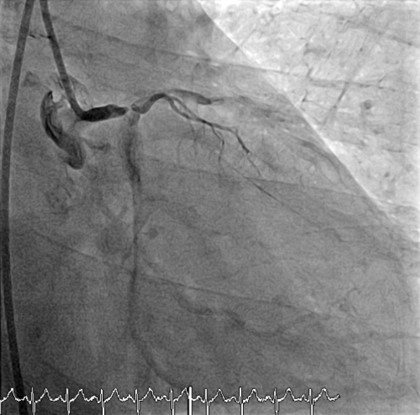
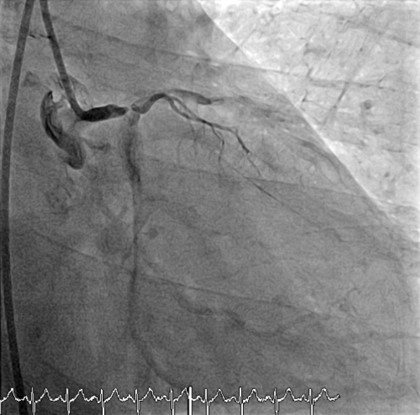
Right dominantLM : 95%stenosis distal LM (Medina 1:1:0:0)




Interventional Management
Procedural Step
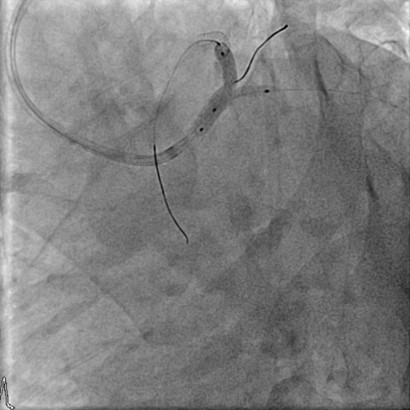
Right femoral approach: 7Fr. Femoral sheath, Heparin 5000 unit was
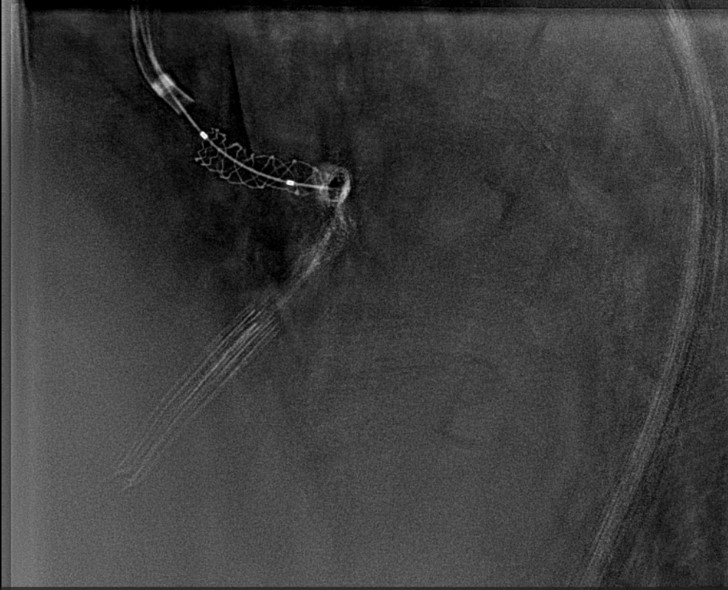
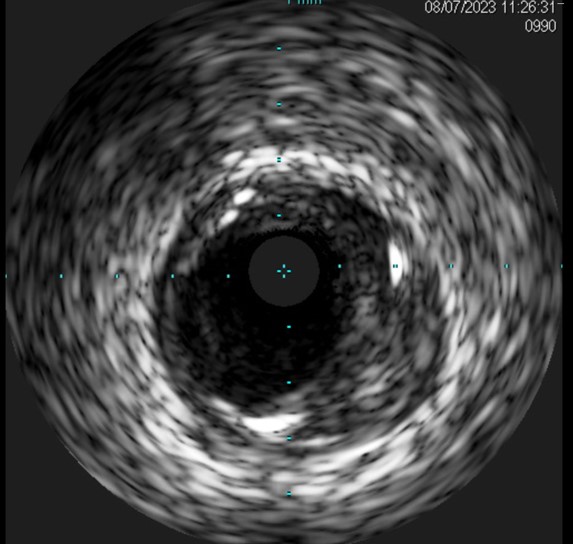
CAG at 3 months with IVUS guide shows ISR 60-65% mid to distal LM.PCI ISR of Left main by IVUS guidance to avoid wiring into side strut of elongate LM stent, and deployed Everolimus eluting stent 40 mm x 12 mm at LM.
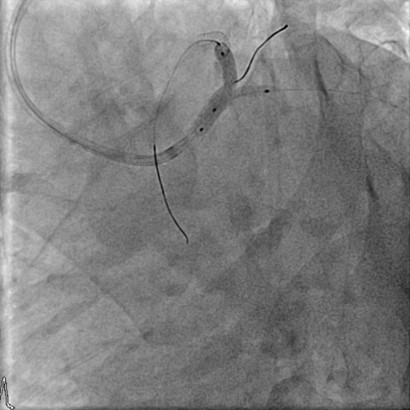
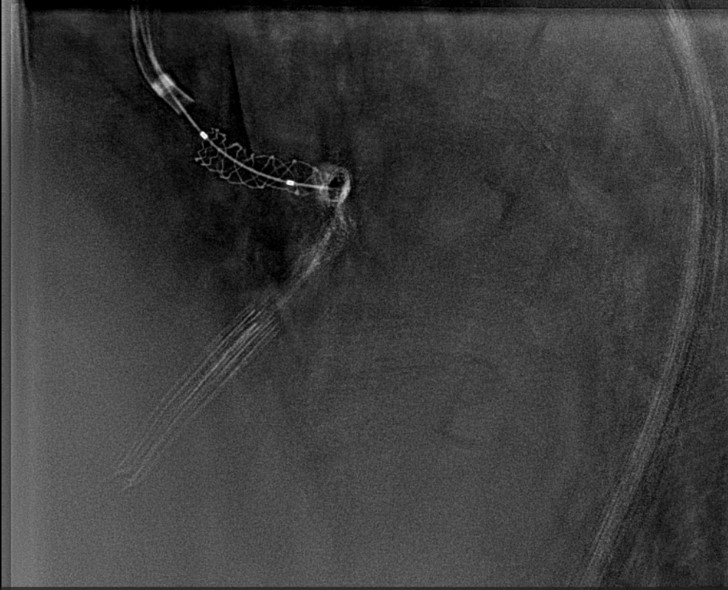
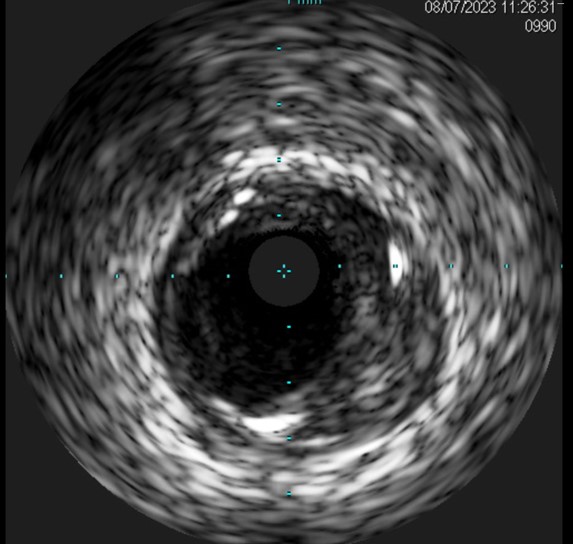
CAG at 3 months with IVUS guide shows ISR 60-65% mid to distal LM.PCI ISR of Left main by IVUS guidance to avoid wiring into side strut of elongate LM stent, and deployed Everolimus eluting stent 40 mm x 12 mm at LM.
Case Summary
IVUS-guided left main (LM) PCI is crucial for determining the actual size of the LM and evaluating the ostial side branches. This information helps in choosing the optimal balloon for post-dilatation. Attempting to compress a floating stent strut using a guiding catheter did not work and may result in longitudinal stent deformity. This could be harmful to the patient if left main (LM) blood flow is compromised and could potentially lead to LM dissection. Stent elongation may result in in-stent restenosis (ISR) because the stent does not cover the plaque lesion, preventing the delivery of drugs to prevent intimal proliferation and plaque protrusion.

