Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-141
Acute Noflow After Stenting of LAD Chronic Total Occlusion
By Chien Hsien Lo
Presenter
Chien Hsien Lo
Authors
Chien Hsien Lo1
Affiliation
Da-Chien General Hospital, Taiwan1,
View Study Report
TCTAP C-141
Coronary - Complication Management
Acute Noflow After Stenting of LAD Chronic Total Occlusion
Chien Hsien Lo1
Da-Chien General Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
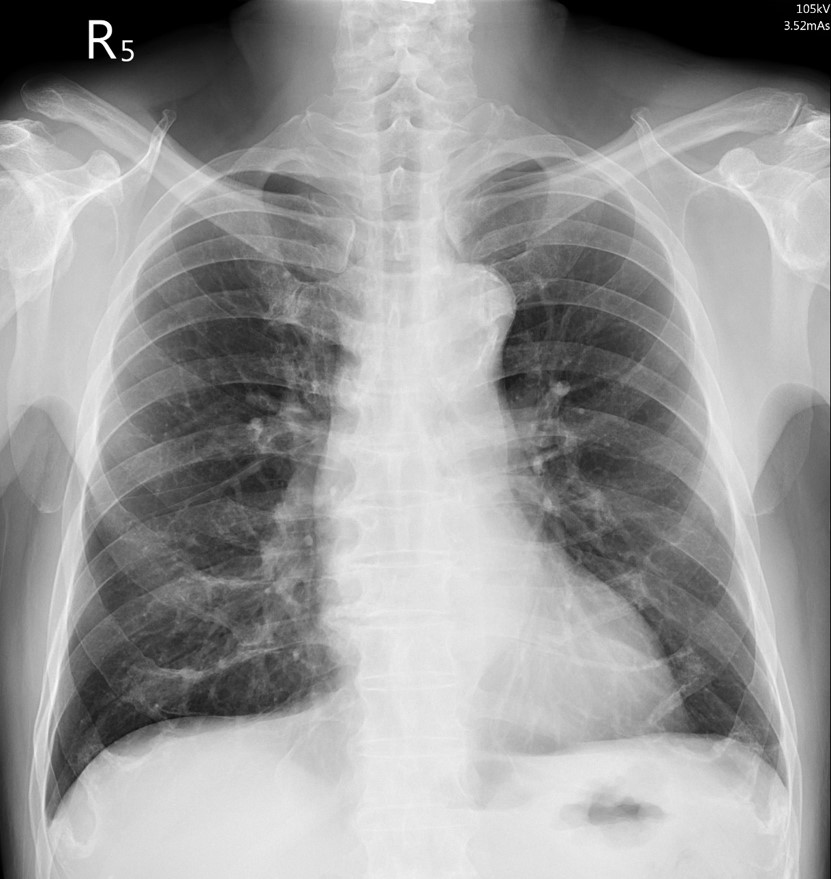
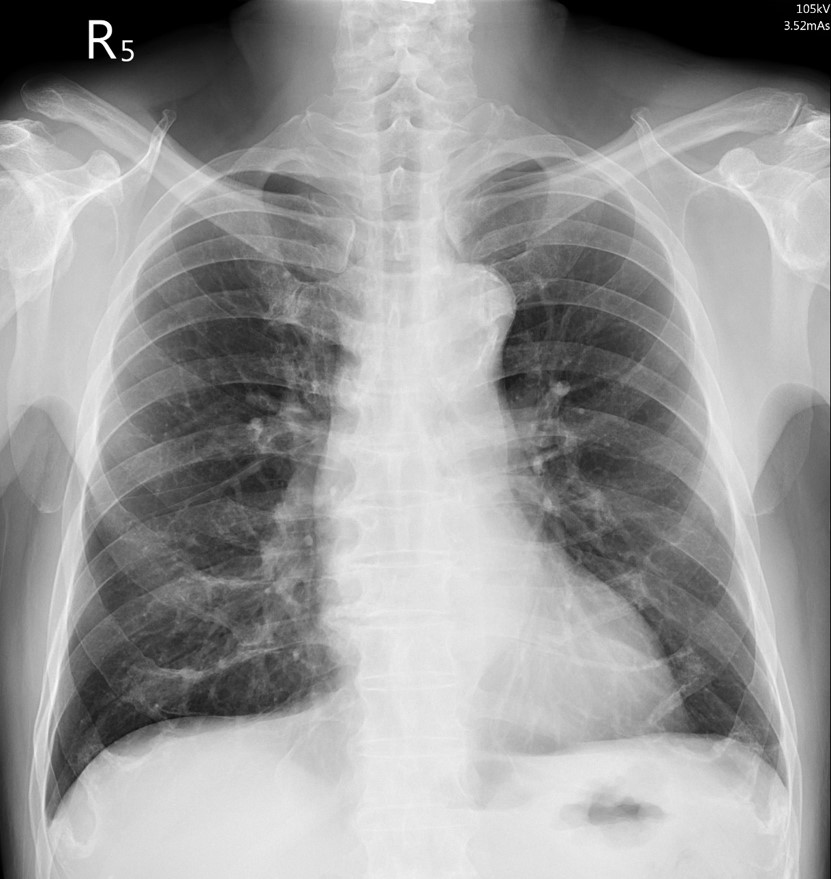
A 68-years-old man, has past history of Diabetes mellitus, dyslipidemia, hypertension and smoking. He presented with intermittent chest tightness for 2-3 months, symptom exacerbated for 2 weeks, complained with dyspnea on exertion.
Relevant Test Results Prior to Catheterization
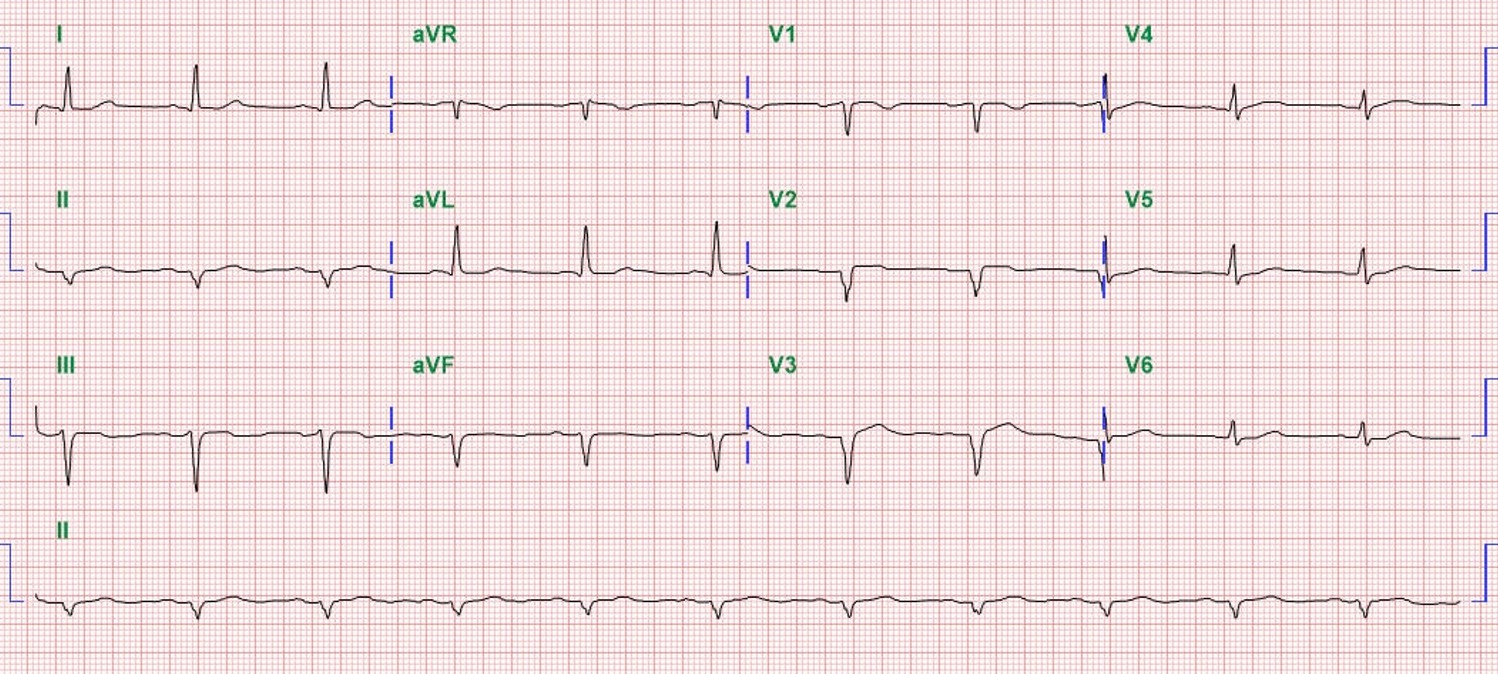
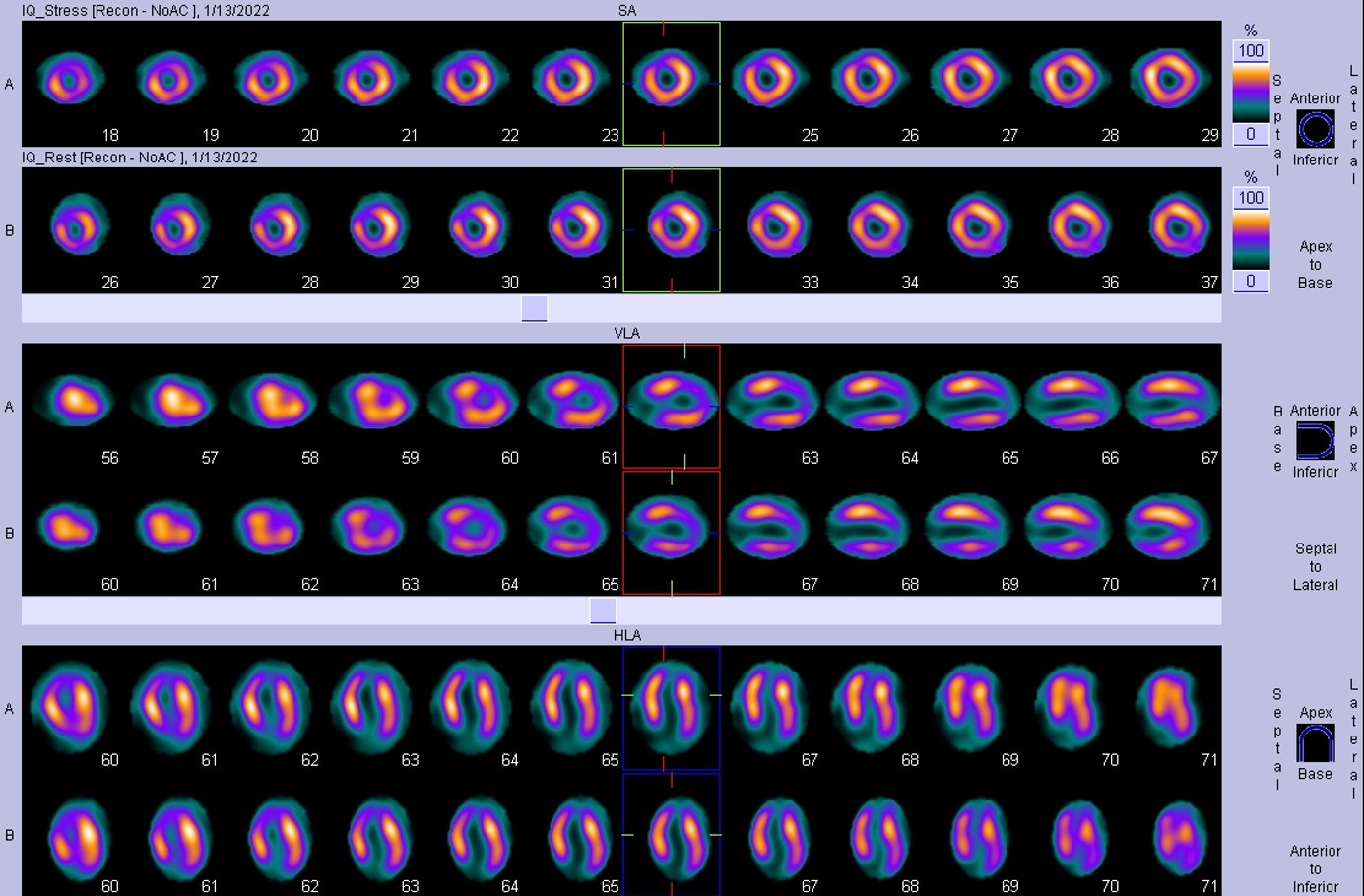
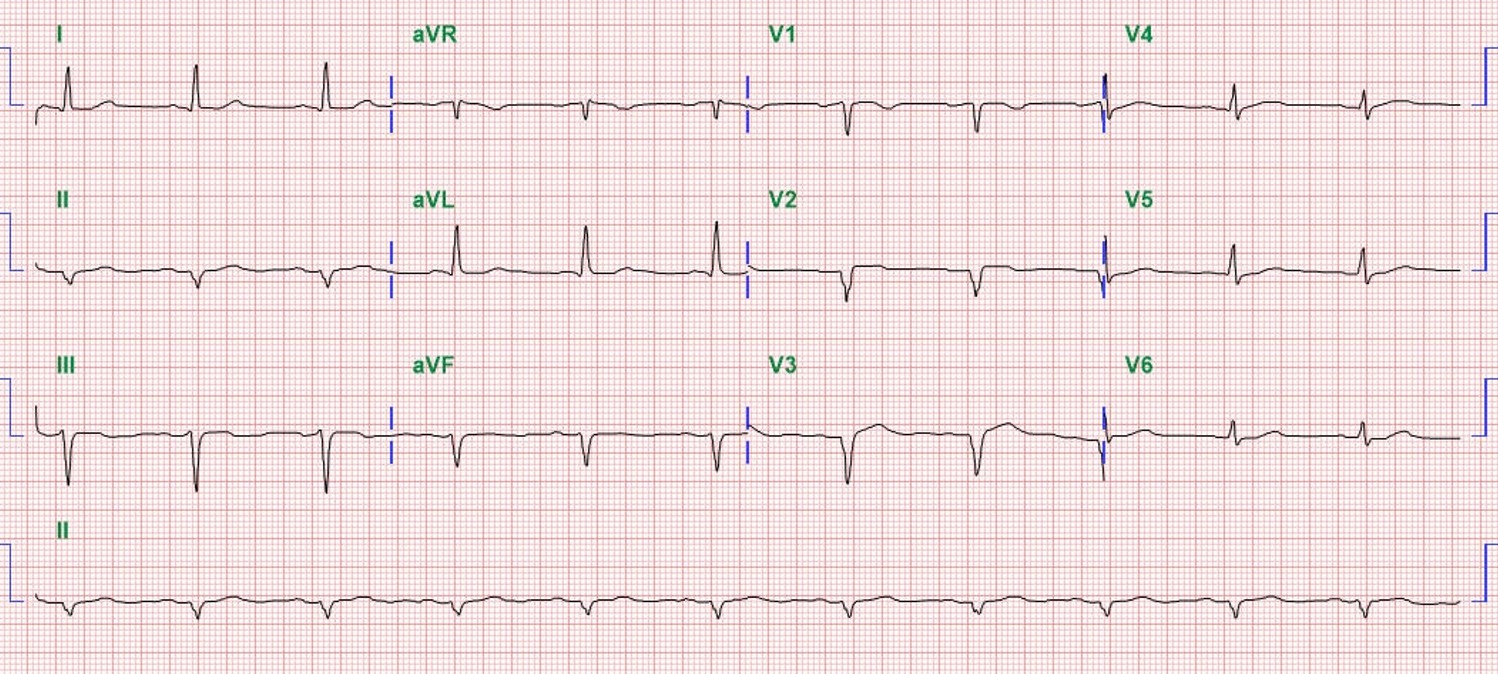
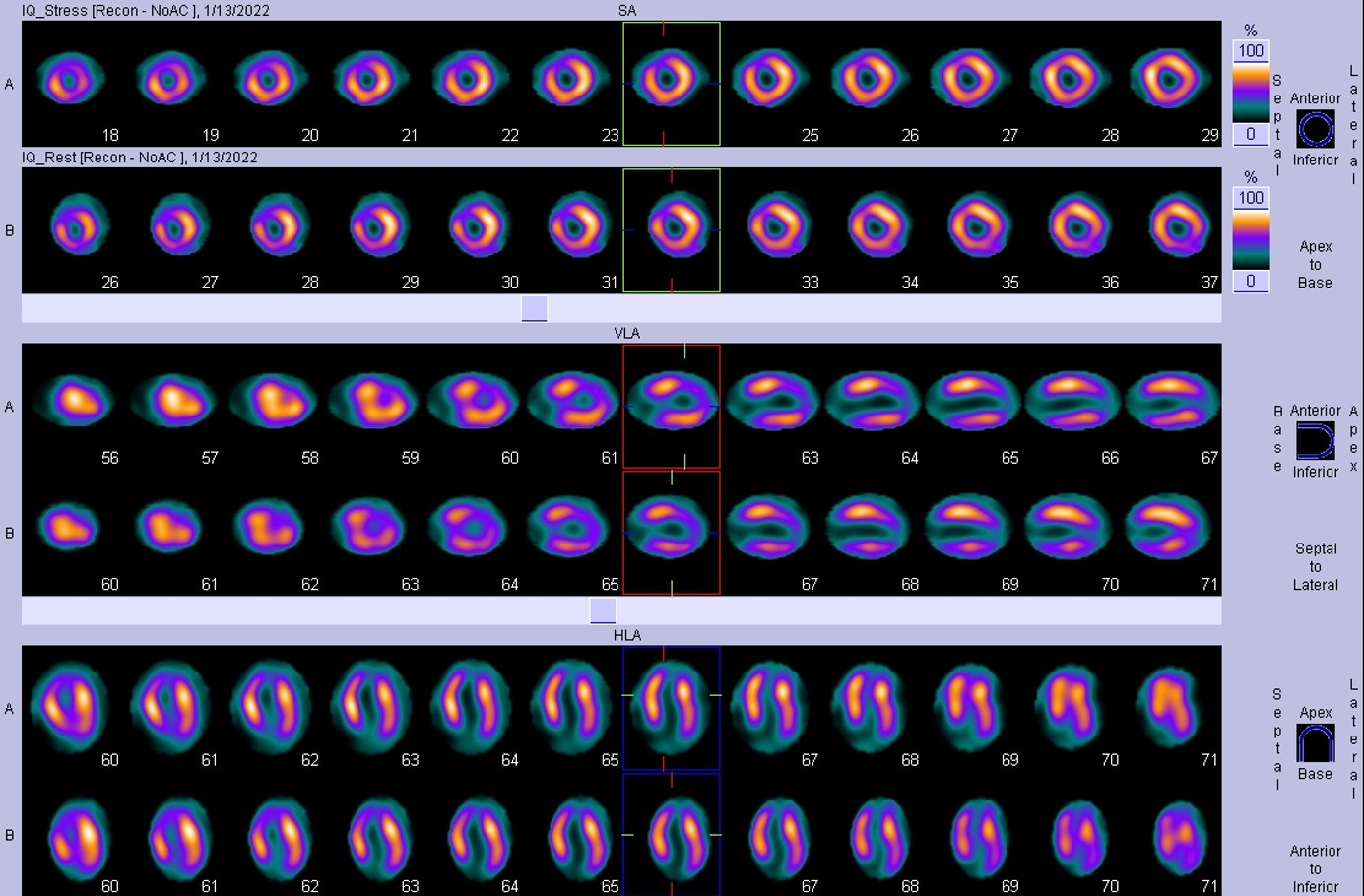
ECG showed sinus rhythm, old anterior infarct. Myocardial perfusion scan showed severe-degree partial reversible and damaged perfusion defect in apical anterior segments.
Relevant Catheterization Findings
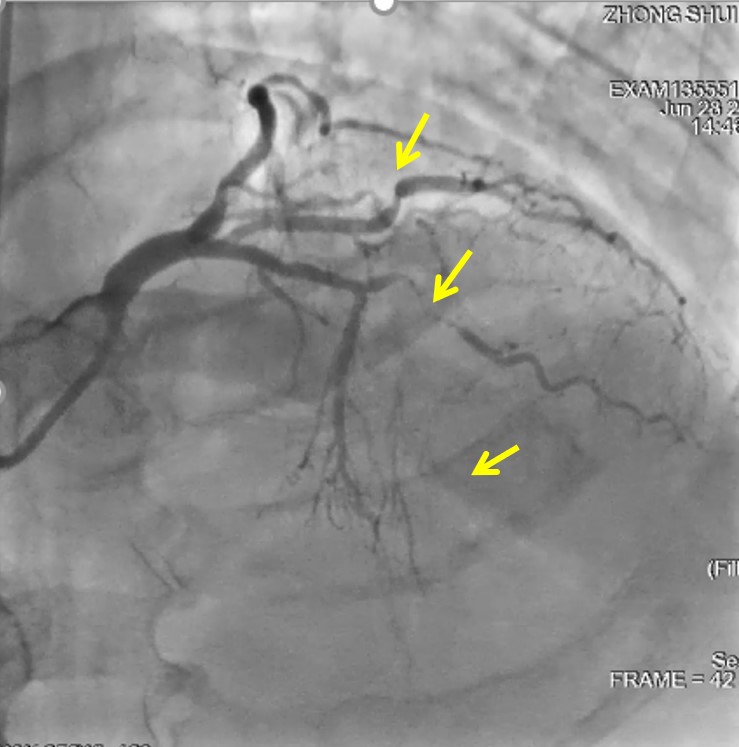
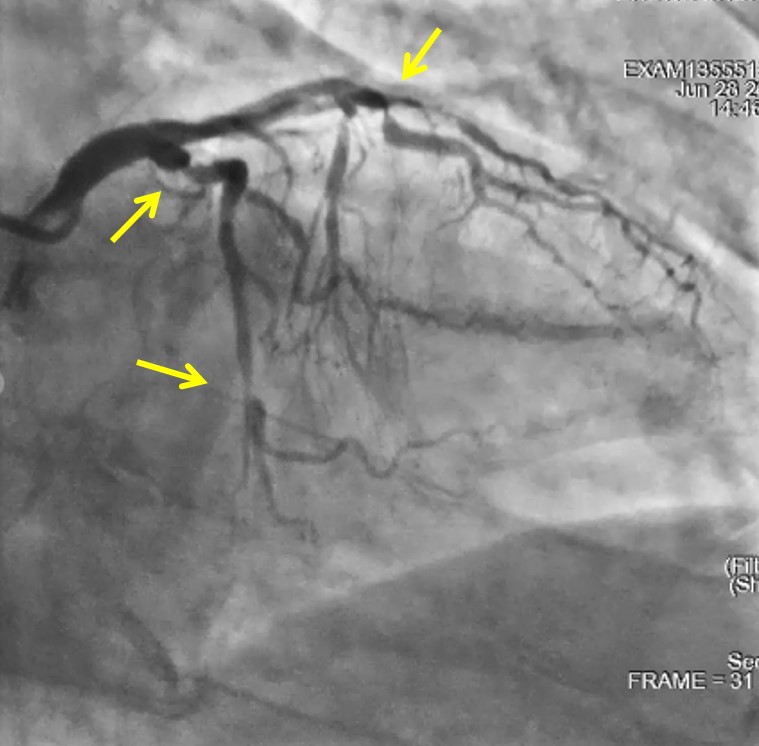
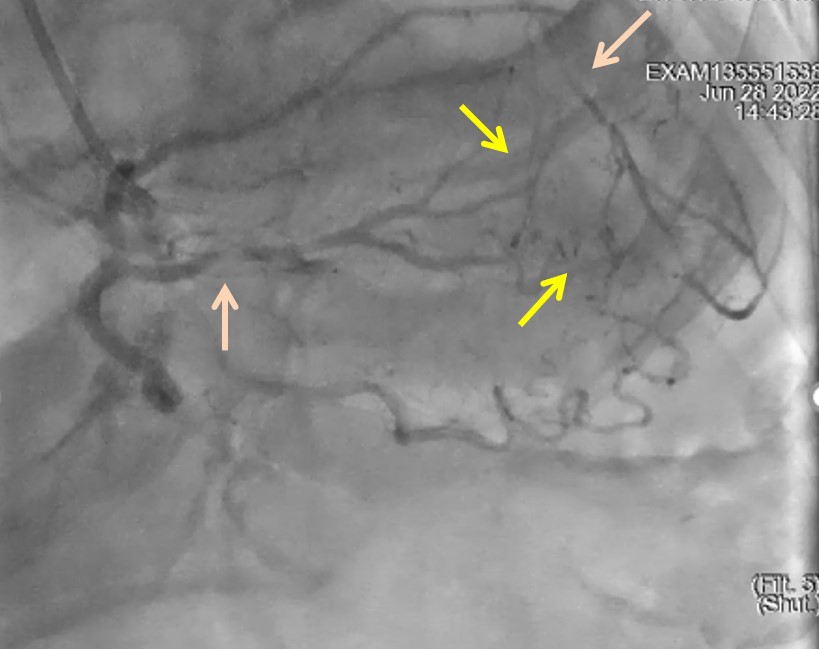
CAG showed m-LAD CTO with grade I~II collaterals from PDA and RV branches, Ramus and LCX stenosis. Syntax score: 24.5, J-CTO score 2 (blunted end, occlusion length >20mm).
Interventional Management
Procedural Step
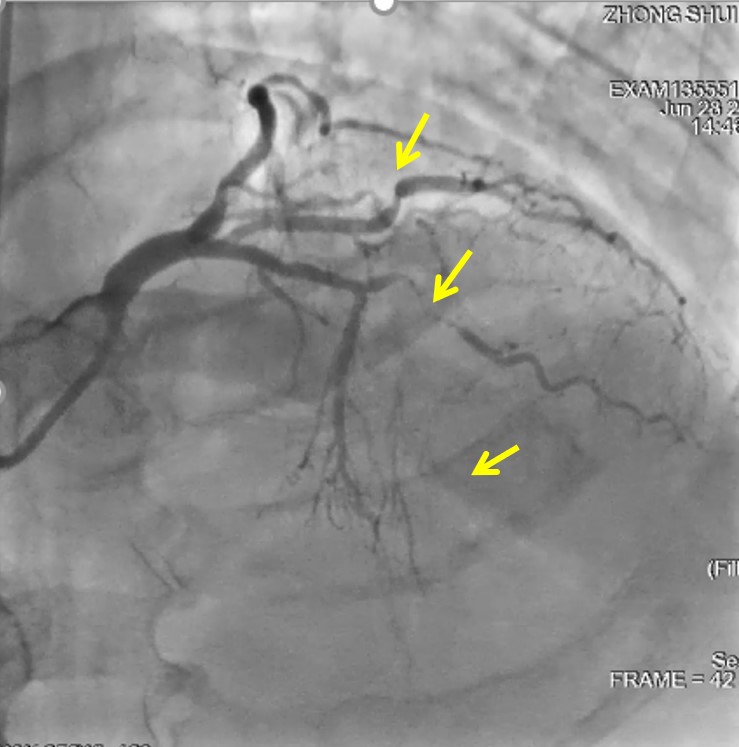
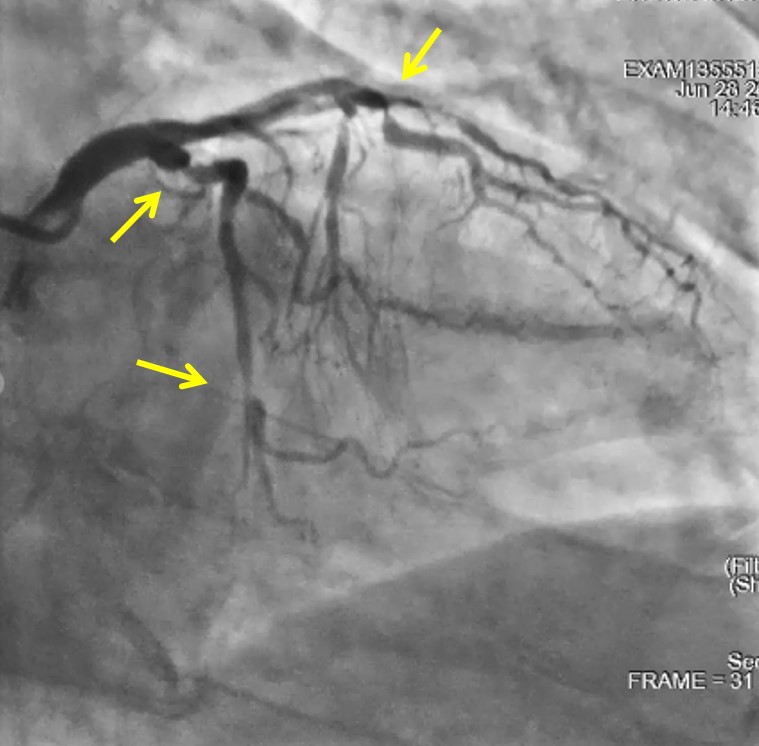
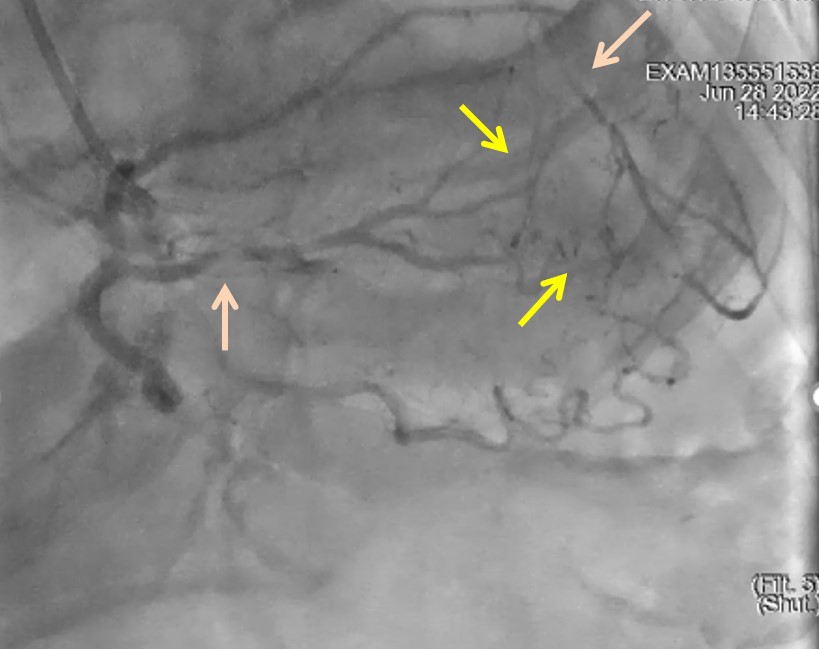
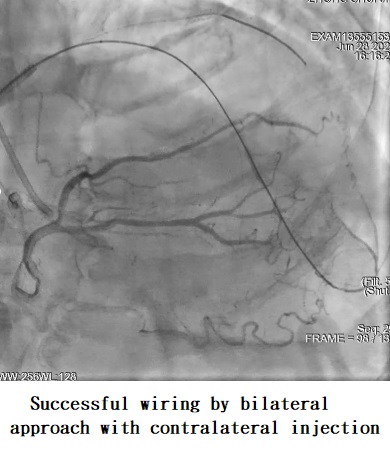
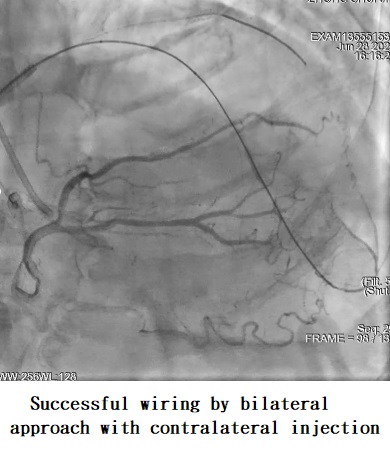
We started from left radial approach, PCI for LAD CTO (antegrade approach first, consider retrograde if require), initial Heparin used 6000IU. Wired used Fielder FC – failed, Fielder XT-R – failed, escalated to Gaia 2nd – unconfirm distal true lumen. Procedure time 60min at the time. Additional heparin gave 1500U (total 7500U). We tried bilateral radial approach with contralateral injection guided, Gaia 2nd wire successfully advance to d-LAD. Procedure time already 90mins, recheck ACT >400s. Sequential balloon pre-dilatation, DES 2.5*33mm to m-d LAD and well distal flow. When prepare distal POBA, acute distal no flow developed (Procedure time 100mins).Causes of no flow can be considered1.Poor distal flow (distal stenosis not cover yet)2.Acute plaque rupture -- not likely3.Intramural hematoma (no IVUS at present)4.Acute thrombosis, inadequate heparination (however ACT >400s 10 min ago). We deployed additional DES 2.5*15mm to d-LAD, still no distal flow. ***Recheck ACT: 178s. Thrombo-aspiration, IC aggrastat, urokinase were done. Repeated thrombo-aspiration and small balloon dilation however distal flow no regained. Patient denied angina
so we stopped the procedure, continue IV aggrastat drip + SC clexane. Patient got angina next morning and EKG progressed anterior wall ST elevation. 2nd look angio showed LAD acute stent thrombosis progression. After multiple small balloon dilatation, thrombus resolved and distal flow regained.




Case Summary
False ACT data will cause the whole procedure worsen and worsenAccurate blood sampling for ACT is important, avoid to mix with contrast.
Take home message;1.Early set up bilateral approach if CTO distal lumen is un-confirmed.2.Thrombus will not resolve under antithrombotic agent if no distal run off flow 3.Never forget to recheck ACT, need the right blood sampling, right heparin dose
Take home message;1.Early set up bilateral approach if CTO distal lumen is un-confirmed.2.Thrombus will not resolve under antithrombotic agent if no distal run off flow 3.Never forget to recheck ACT, need the right blood sampling, right heparin dose

