Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-150
Simplifying the Procedure for the Complex Patient: Stabilizing Hemodynamics for Safer PCI Using Percutaneous Left Ventricular Assist Device
By Toshikazu Kashiyama, Hitoshi Nakano
Presenter
Hitoshi Nakano
Authors
Toshikazu Kashiyama1, Hitoshi Nakano1
Affiliation
Sumitomo Hospital, Japan1,
View Study Report
TCTAP C-150
Coronary - Hemodynamic Support
Simplifying the Procedure for the Complex Patient: Stabilizing Hemodynamics for Safer PCI Using Percutaneous Left Ventricular Assist Device
Toshikazu Kashiyama1, Hitoshi Nakano1
Sumitomo Hospital, Japan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
An 82-year-old male with history of PCI in LAD was sent to our hospital for severe chest pain which was experienced 10 days before and subsequent breathing difficulty. His blood pressure was 125/75 mmHg, heart rate was 90 bpm, saturation was 92% on 10 L/min O2 by mask. Wheezes were heard on chest auscultation and the chest X-ray showed bilateral pulmonary edema (Figure 1).


Relevant Test Results Prior to Catheterization
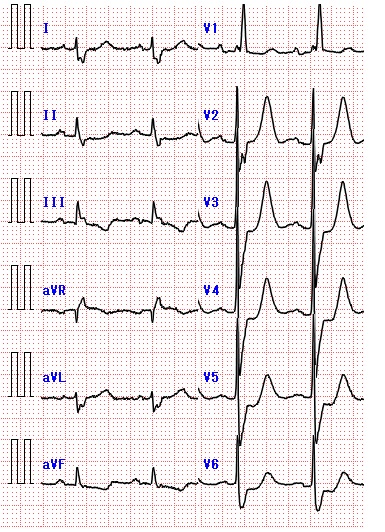
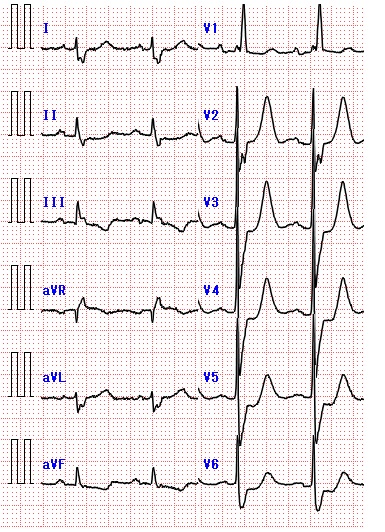
His ECG showed slight ST elevation over aVR lead and diffuse slight depression over precordial leads (Figure 2). Bedside echocardiography revealed globally decreased LV contraction with EF of 25% and moderate MR. . Because the blood test showed elevated troponin I of 6.36 ng/ml and NT-proBNP of 5300 pg/ml, he was transferred to catheterization laboratory suspected with acute hear failure due to recent myocardial infarction.
Relevant Catheterization Findings
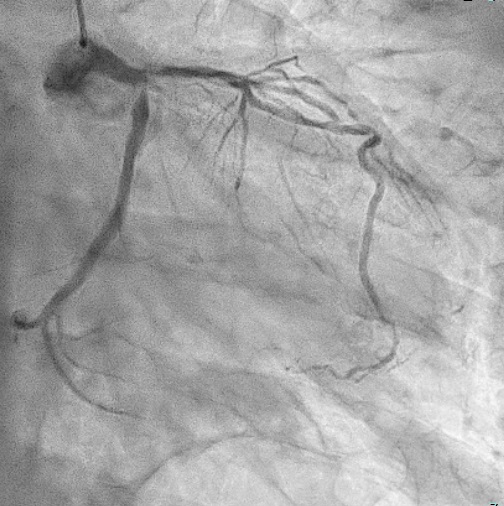
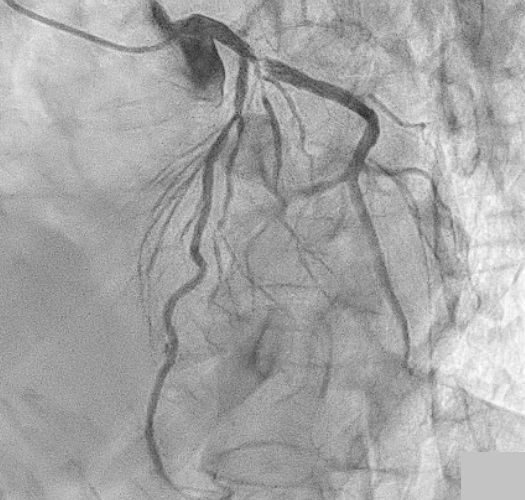
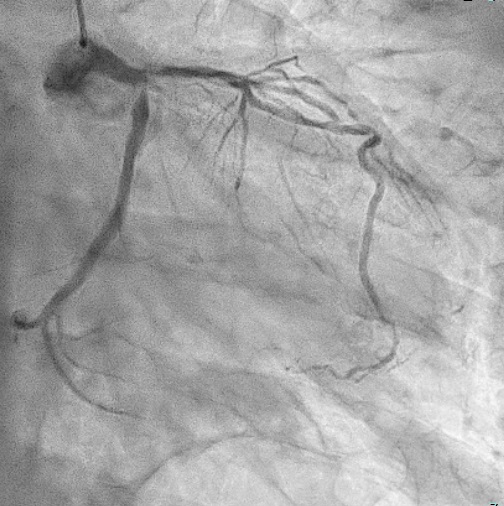
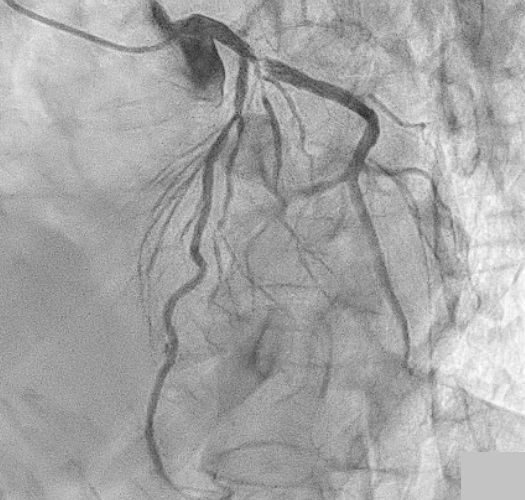
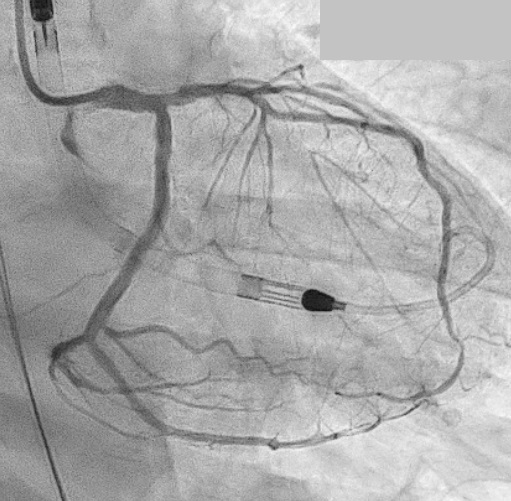
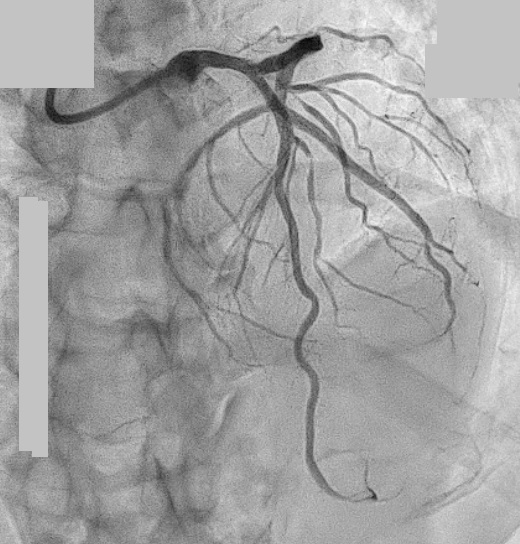
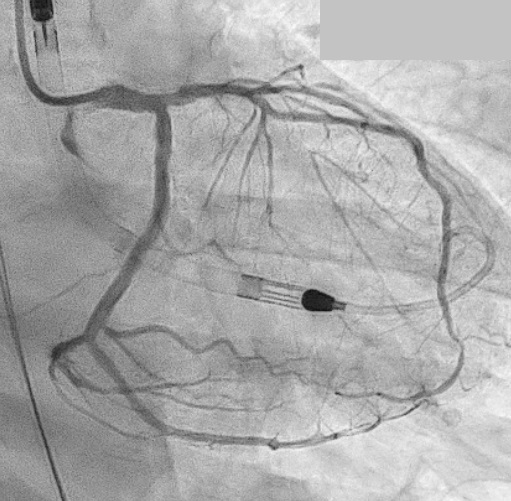
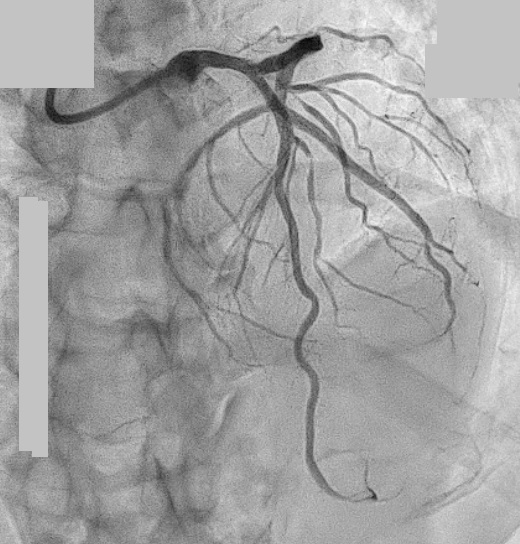
Coronary angiogram was demonstrated with 4 Fr diagnostic catheter via the right radial artery, which showed 90% stenosis in ostial LAD,99% stenosis in ostial LCX, and significant disease in the mid segment of LAD with hypoplastic RCA (Figure 3,4).
Interventional Management
Procedural Step
Because his saturation gradually went down under 85% and blood pressure also fell under 80/60 mmHg during coronary angiogram, he was put on Noninvasive Positive Pressure Ventilation (NPPV) and Percutaneous Left Ventricular Assist Device (Impella) was inserted via right femoral artery.


Case Summary
By the rapid introduction of Impella, unnecessary intubation and aggressive complex procedure for the elderly patient was avoided, even with the challenging clinical situation. This powerful device may leave physicians a good margin to discuss about the better treatment options.

