Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-120
Loss of Flow in LCx and I Was Unable to Move the Guidewire Freely.
By Chatree Wongsinkongman, Viroj Muangsillapasart
Presenter
Chatree Wongsinkongman
Authors
Chatree Wongsinkongman1, Viroj Muangsillapasart1
Affiliation
Chulabhorn Hospital, Thailand1,
View Study Report
TCTAP C-120
Coronary - Complication Management
Loss of Flow in LCx and I Was Unable to Move the Guidewire Freely.
Chatree Wongsinkongman1, Viroj Muangsillapasart1
Chulabhorn Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 73-year-old Asian female with preexisting diseases of psoriatic arthritis, hypertension and hyperlipidemia presented with typical ischemic chest discomfort 2 hours prior to admission. Physical examination revealed BP 140/80 mmHg without other prominent abnormal physical examination. She was initially diagnosed as high risk NSTE-ACS at ER and we were consulted to perform coronary angiogram urgently.


Relevant Test Results Prior to Catheterization
Echocardiogram showed mildly impaired LV systolic function, LVEF 46% with hypokinesia in anterior-anteroseptal wall with akinesia in inferior wall. Chest X-ray showed no evidence of pulmonary edema. High-sensitivty troponinT was pathologically elevated at 331 pg/ml. LDL-C showed 196 mg/dL. CBC, BUN, creatinine and electrolyte were all within normal range.


Relevant Catheterization Findings
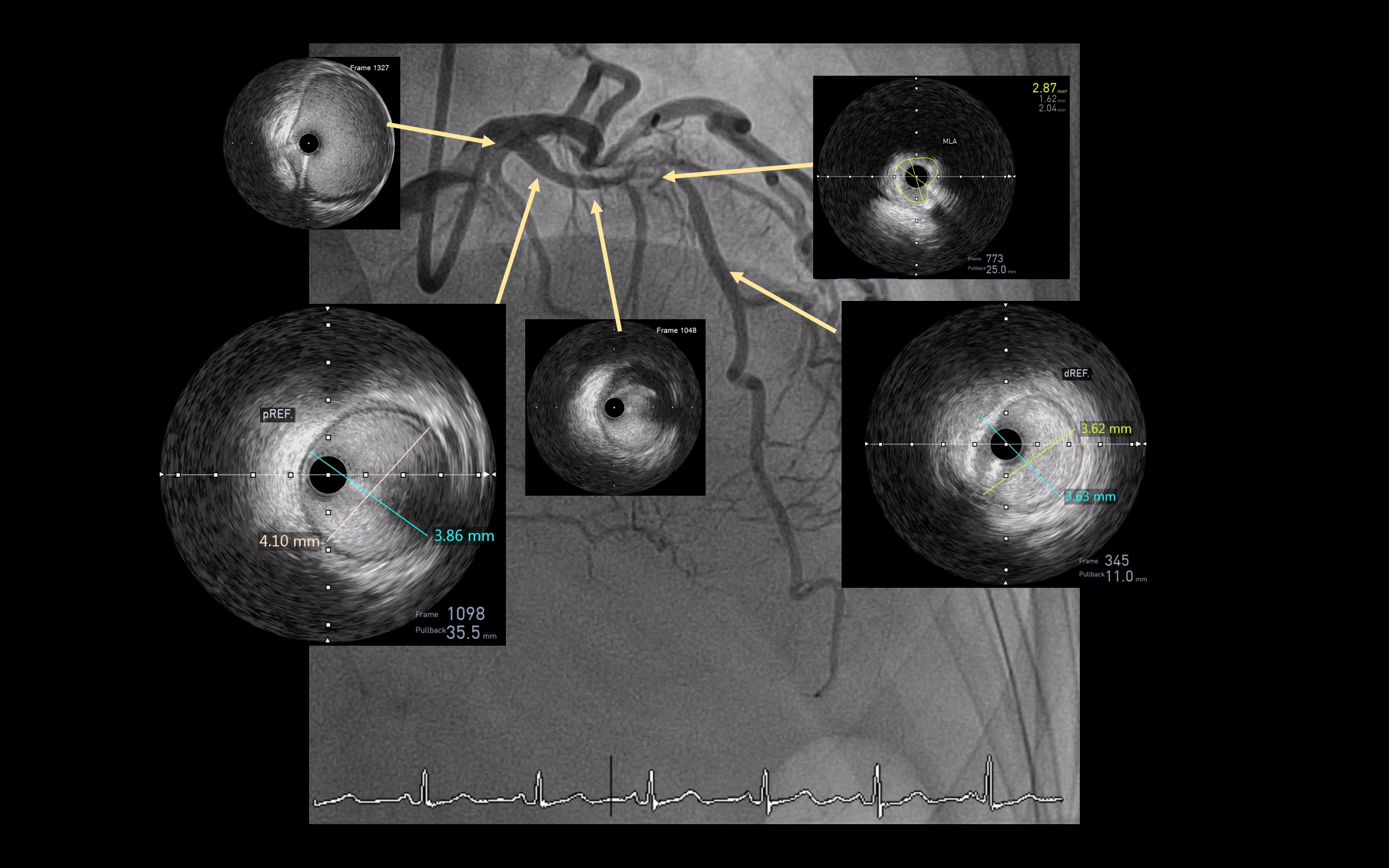
Coronary angiogram showed right dominant system. Left main appeared non-significant stenosis, LAD showed 95% diffuse stenosis at proximal to mid segment, DG showed 75% diffuse stenosis at proximal segment, Lcx showed 90% diffuse stenosis at proximal segment, OM2 showed 50% discrete stenosis at ostial segment, RCA showed 100% total occlusion at proximal segment which received collateral circulation from S1 to distal PDA. All of coronary showed TIMI grade 3 flow.
Interventional Management
Procedural Step
PCI was planned using right radial approach with 6F vascular sheath. Guiding Cordis XB 3.0 6F was engaged to LCA. Asahi Sion Blue 0.014" guidewire to Lcx and Asahi Sion 0.014" guidewire to LAD. PCI to LAD was identified as culprit lesion and was planned to performed under IVUS guidance, which IVUS showed mixed fibrous and attenuated plaque 270 degrees with length 8 mm, lesion length was 32 mm, proximal reference EEM diameter 4.1x3.86 mm, distal reference EEM diameter 3.62x3.63 mm with plaque burden < 50%, then SC balloon 2.5x15 mm was dilated at proximal to mid LAD at 10-14 atm. Everolimus-eluted DES 3.0x33 mm was implanted at proximal to mid segment. After stent implantation, the Lcx flow was reduced to TIMI flow grade 2. ACT was checked which was 234, so heparin 2000 unit was administered intracoronary Asahi Fielder XT-R guidewire was advanced to OM1 as jailed wire protection. Zotarolimus-eluting stent 2.75x22 mm was implanted at proximal LCx. Sion Blue was unable to remove and showed evidence of wire unraveling. Fielder XT-R was attempted to advance to distal Lcx but failed. Finecross microcatheter was advanced along with Sion Blue and was able to remove Fielder XT-R guidewire. Finecross microcatheter was unable to advance to distal segment of wire, so another Sion guidewire was advanced to distal LCx. Microcatheter was able to advance to distal segment of Sion Blue and was able to remove Sion Blue guidewire completely.


Case Summary
1. Guidewire fracture and unraveling is not a common complication during PCI but could cause catastrophe if left unmanaged.2. Microcatheter is your best friend to correct this complication, mastering the microcatheter usage is a must skill.3. Complication management according to algorithm is good thinking process that can be easily followed.

