Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-010
Three Months Follow-up Patients After Acute Coronary Syndrome
By Loc Vu, Dung Ho, Chinh Duc Nguyen, Thuan Huynh, Le Anh Do, Hieu Bui, Khang Phuc Nguyen, Tuong Diep, Quang Minh Mai, Thach Nguyen
Presenter
Loc Vu
Authors
Loc Vu1, Dung Ho2, Chinh Duc Nguyen3, Thuan Huynh4, Le Anh Do5, Hieu Bui2, Khang Phuc Nguyen6, Tuong Diep1, Quang Minh Mai1, Thach Nguyen7
Affiliation
Tan Tao University, Vietnam1, Thong Nhat Hospital, Vietnam2, Can Tho Stroke International Services General Hospital, Vietnam3, University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam4, E Hospital, Vietnam5, District 11 Hospital, Vietnam6, Methodist Hospital, Meriville, USA7
View Study Report
TCTAP A-010
ACS/AMI
Three Months Follow-up Patients After Acute Coronary Syndrome
Loc Vu1, Dung Ho2, Chinh Duc Nguyen3, Thuan Huynh4, Le Anh Do5, Hieu Bui2, Khang Phuc Nguyen6, Tuong Diep1, Quang Minh Mai1, Thach Nguyen7
Tan Tao University, Vietnam1, Thong Nhat Hospital, Vietnam2, Can Tho Stroke International Services General Hospital, Vietnam3, University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam4, E Hospital, Vietnam5, District 11 Hospital, Vietnam6, Methodist Hospital, Meriville, USA7
Background
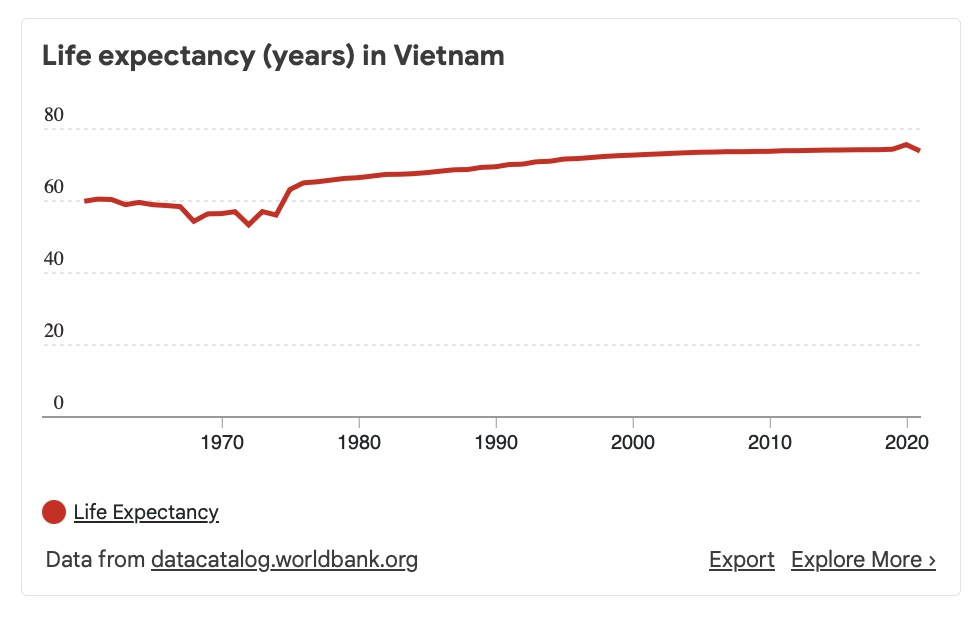
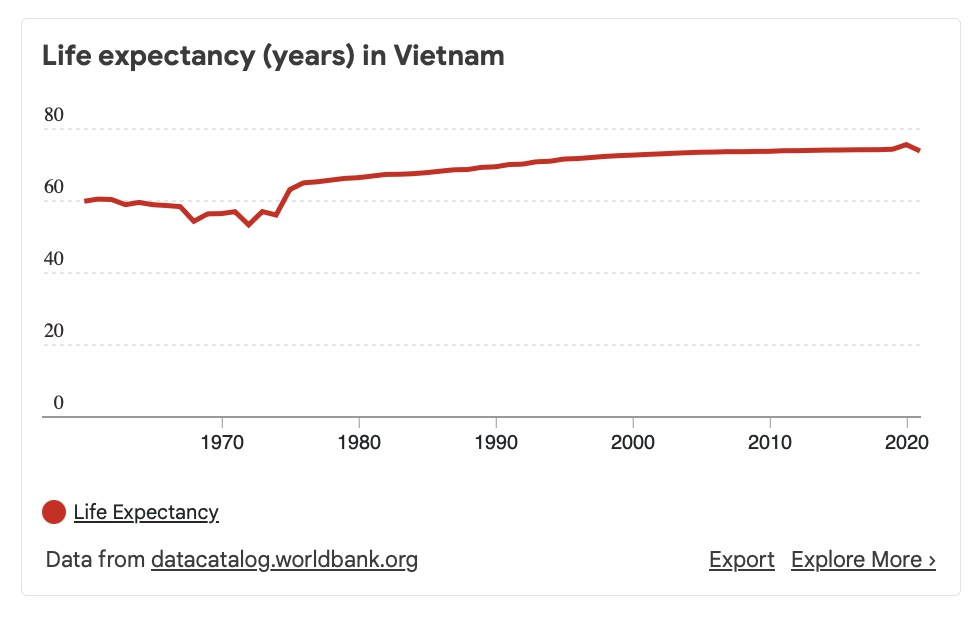
Recently, along with a better quality of life in Vietnam. Vietnam's life expectancy (years) has slightly increased to 75.38 years (World Bank 2020). The structure of the disease burden is changing from infectious to cardiovascular and metabolic disease. In particular, atherosclerotic cardiovascular disease is growing up. Hence, the diagnosis and management of acute coronary syndrome (ACS) in elderly patients are also facing a challenge. This study presents the data of ACS from a geriatric center in Vietnam.


Methods
A prospective cohort study from a single center was performed. Ninety patients diagnosed with ACS were enrolled. At the admission time, a comprehensive evaluation was performed (ECG, Killip classification, grace score, cardiac enzyme, lipid profile, echocardiogram), and the management strategy was based on multi-discipline consultations with patients and their families. The past medical history, management process, laboratory tests, and length of stay at the hospital were recorded. All patients are followed up for three months.
Results
90 (51 males) patients met the inclusion criteria with a mean age of 75.2 +/- 7.7 years old, which included 40 STEMI and 50 Non-STEMI patients. Initially, the ECG suggested 21/40 cases of the STEMI has infarction at inferior area, 17/40 cases at Anterior. Killip classification showed one patient was Killip IV, and Killip II and III were 18 and 7 patients, respectively. 55 cases underwent primary PCI. The ratio of patients who underwent PCI in STEMI was 90% compared to 34.5% of patients in the non-STEMI group (p<0.05). The difference in the length of hospital stays in patients with the left main disease (13.7 days) and no (10.6 days) was statically significant (p<0.001). Meanwhile, the difference in the length of stay in the hospital for STEMI (10.7 days) and non-STEMI (11.3 days) was not statically significant (p>0.05). Before discharge, the echocardiogram showed 7 patients had heart failure (HF) with a mildly reduced ejection fraction (EF) and 2 with HF-reduced EF. All were stable at discharge and three months later.
Conclusion
Early results in the treatment of ACS in Vietnamese elderly patients are promising. The personalized management for each patient based on multidisciplinary consultation and discussion with patients and family is the key to success in managing MI in very patients.

