Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-039
Efficacy and Safety of Angiotensin Receptor-Neprilysin Inhibitor Versus Angiotensin Converting Enzyme Inhibitor or Angiotensin Receptor Blocker in Acute Myocardial Infarction Patients: A Meta-Analysis of Randomized Controlled Trials
By Muammar Emir Ananta, Ignatius Ivan, Alya Darin Wijaya, Chabib Fachry Albab, Siska Danny
Presenter
Muammar Emir Ananta
Authors
Muammar Emir Ananta1, Ignatius Ivan2, Alya Darin Wijaya3, Chabib Fachry Albab4, Siska Danny5
Affiliation
Jakarta Islamic Hospital Cempaka Putih, Indonesia1, Atma Jaya Catholic University of Indonesia, Indonesia2, University College London, United Kingdom3, Alumnus of Universitas Airlangga, Surabaya, Indonesia4, Indonesian Society of Interventional Cardiology, Indonesia5
View Study Report
TCTAP A-039
Pharmacotherapy (Coronary)
Efficacy and Safety of Angiotensin Receptor-Neprilysin Inhibitor Versus Angiotensin Converting Enzyme Inhibitor or Angiotensin Receptor Blocker in Acute Myocardial Infarction Patients: A Meta-Analysis of Randomized Controlled Trials
Muammar Emir Ananta1, Ignatius Ivan2, Alya Darin Wijaya3, Chabib Fachry Albab4, Siska Danny5
Jakarta Islamic Hospital Cempaka Putih, Indonesia1, Atma Jaya Catholic University of Indonesia, Indonesia2, University College London, United Kingdom3, Alumnus of Universitas Airlangga, Surabaya, Indonesia4, Indonesian Society of Interventional Cardiology, Indonesia5
Background
Blockade of renin-angiotensin system (RAS) with angiotensin receptor-neprilysin inhibitor (ARNI) has been shown to be superior to angiotensin converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) in improving survival and reducing hospitalization for heart failure (HHF) of heart failure patients. However, its benefit remains controversial in acute myocardial infarction (AMI) patients.
Methods
We performed systematic search of databases through Pubmed, Embase, and Cochrane Library for all eligible articles. The inclusion criteria were (1) Randomized Controlled Trials (RCTs); (2) AMI patients; (3) Comparison of efficacy and/or safety between ARNI with ACEI or ARB; (4) Hospital initiation of treatments; (5) Full-text article available in English. The primary endpoint was major adverse cardiovascular events (MACE). Secondary endpoints were all-cause mortality, cardiovascular mortality, all-cause rehospitalization, HHF, malignant arrhythmia, myocardial infarction, parameters of left ventricular function, and adverse effects. Pairwise meta-analyses were conducted to pool risk ratio (RR) for categorical outcomes and weighted mean difference (WMD) for numerical outcomes with corresponding 95% confidence intervals (CIs).
Results
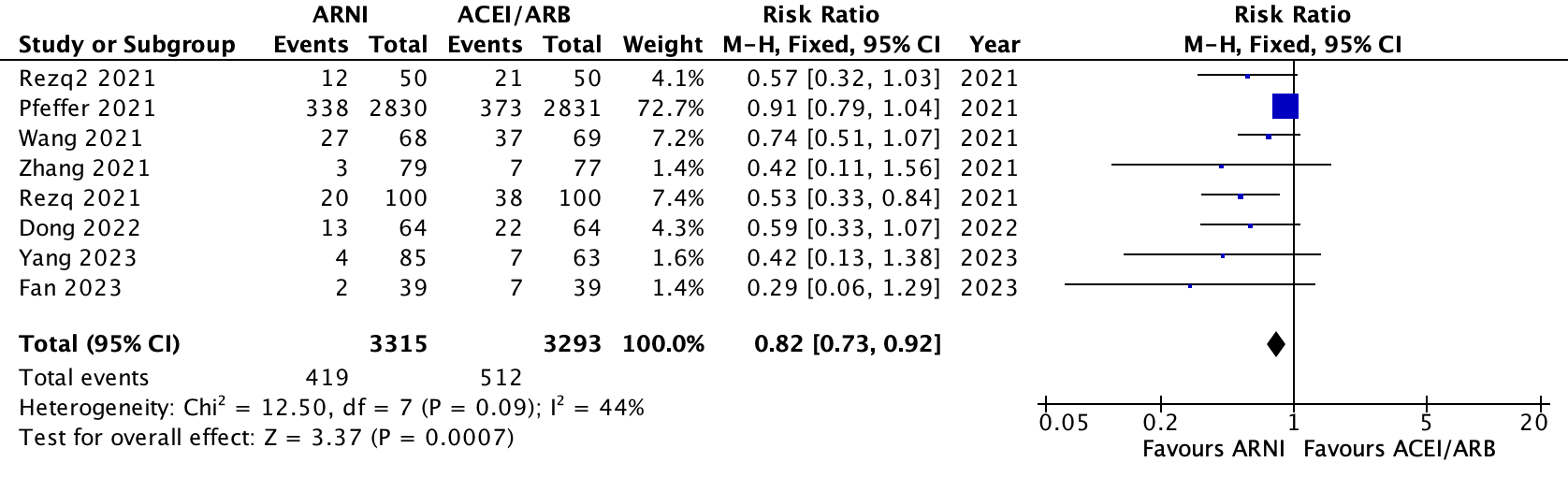
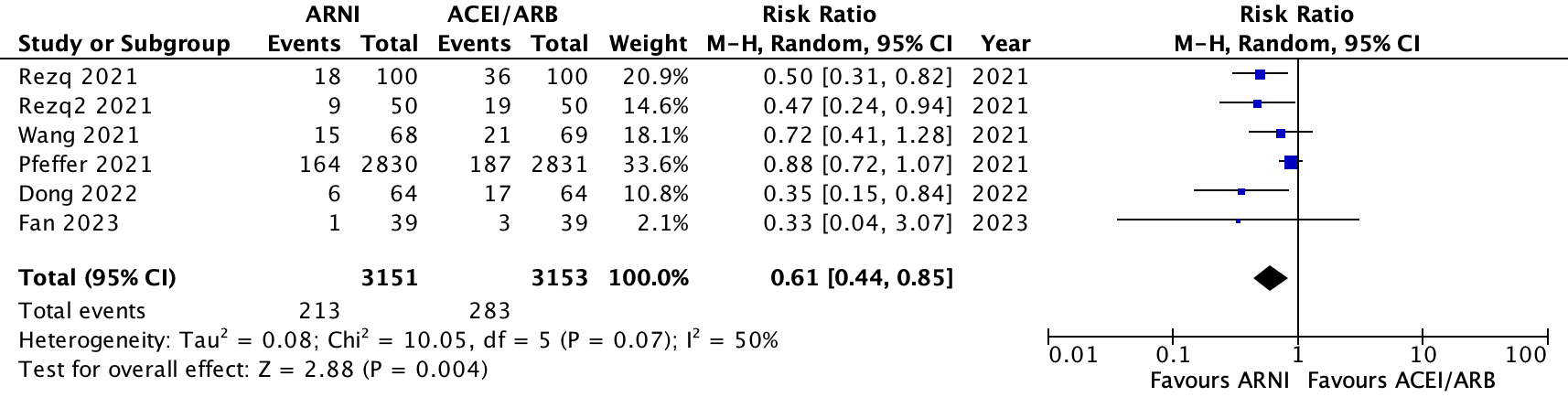
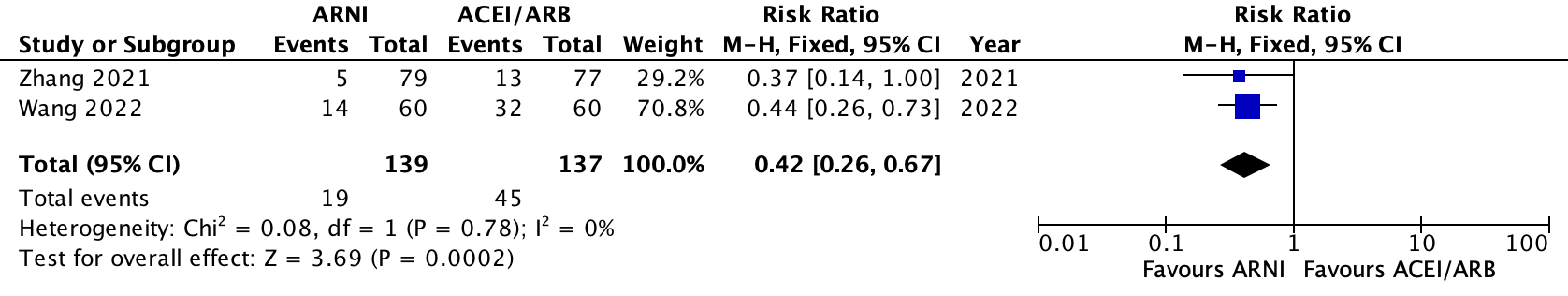
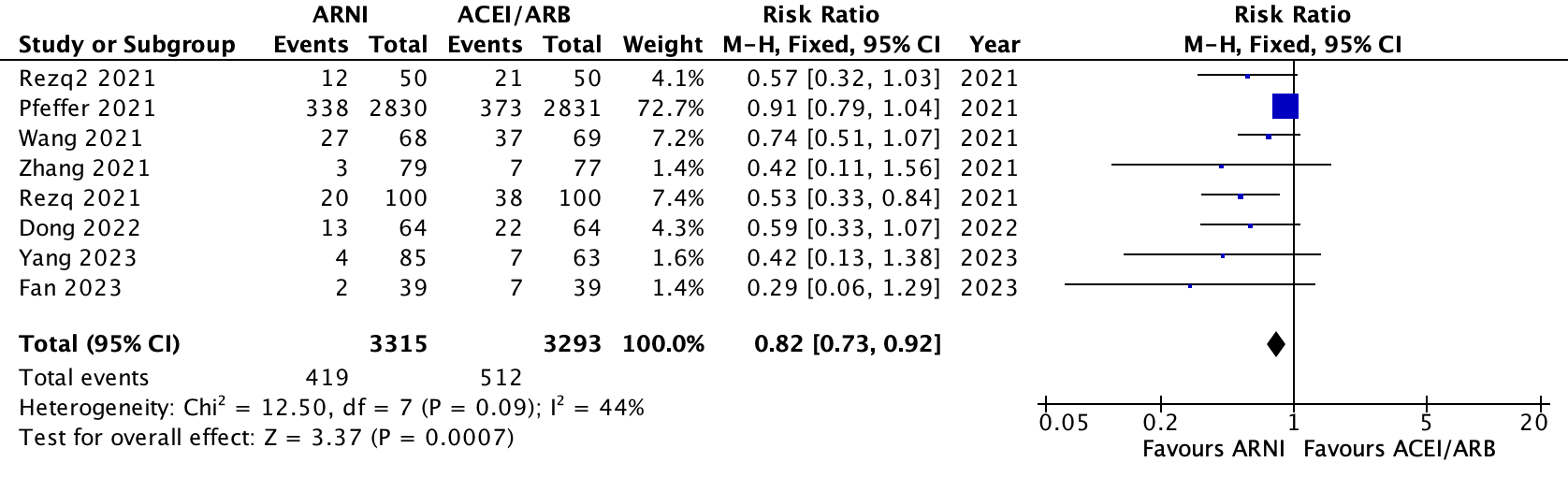
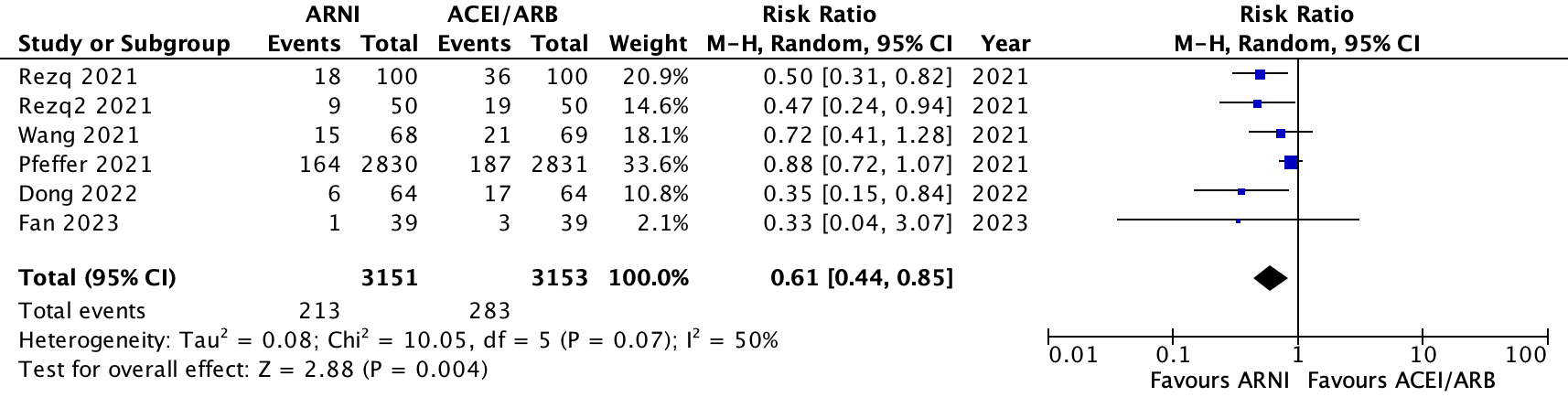
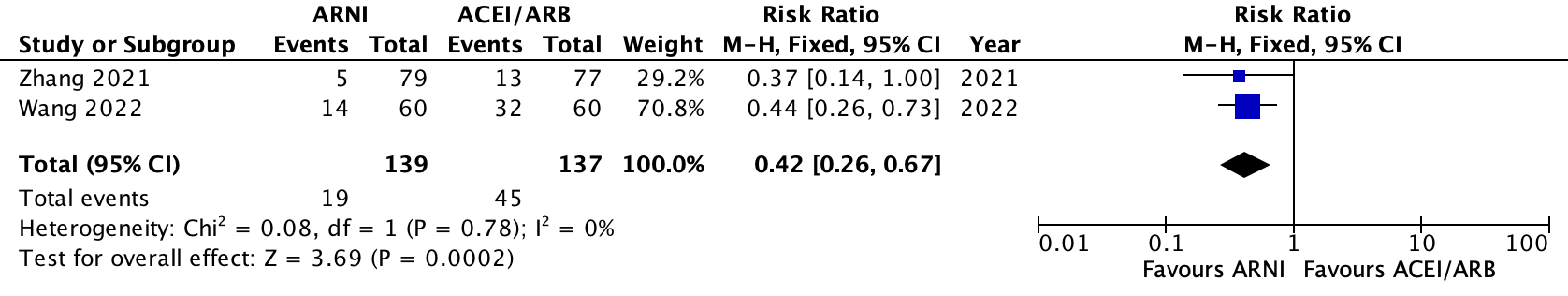
9 RCTs were included involving a total of 6700 AMI patients. 3375 patients in ARNI group and 3325 patients in ACEI or ARB group. 8 of the studies were conducted in ≤ 200 patients. Follow-up period ranges from 1 month to 36 months. Meta-analyses found that compared to treatment with ACEI or ARB, ARNI use was significantly associated with 18% lower incidence of MACE [RR 0.82 (95% CI 0.73–0.92; p=0.00007; I2=44%)], 23% lower incidence of HHF [RR 0.77 (95% CI 0.65–0.91; p = 0.002; I2=37%)], and 58% lower readmission rates [RR 0.42 (95% CI 0.26–0.67; p = 0.00002; I2=0%)]. However, there was a 30% increase in hypotension [RR 1.30 (95% CI 1.30; 1.19–1.42; p < 0.00001; I2=0%)]. Patients treated with ARNI significantly had higher left ventricular ejection fraction [WMD 3.42% (95% CI 2.11–4.73%; p < 0.00001; I2=30%)], lower left ventricular end systolic diameter [WMD -4.39 mm (95% CI -5.90– -2.88 mm; p < 0.00001; I2=33%)], and lower left ventricular end diastolic diameter [WMD -3.09 mm (95% CI -4.59– -1.59; p < 0.00001; I2=42%)] at the end of follow up. Egger’s regression test found significant publication bias for MACE (p = 0.0009) and HHF (p = 0.0051).
Conclusion
Compared to treatment with ACEI or ARB, AMI patients treated with ARNI have lower incidence of MACE, HHF, and all-cause rehospitalization and better left ventricular function, but with higher risk of hypotension. Further research is needed to confirm these findings as most studies have small sample size.

