Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-020
Validation of New Modified ARC-HBR Criteria in Patients Undergoing Percutaneous Coronary Intervention in Thailand
By Donluck Poonkasem, Krissada Meemook
Presenter
Donluck Poonkasem
Authors
Donluck Poonkasem1, Krissada Meemook2
Affiliation
Vibharam Hospital, Thailand1, Ramathibodi Hospital Mahidol University, Thailand2
View Study Report
TCTAP A-020
Clinical Trials & Science
Validation of New Modified ARC-HBR Criteria in Patients Undergoing Percutaneous Coronary Intervention in Thailand
Donluck Poonkasem1, Krissada Meemook2
Vibharam Hospital, Thailand1, Ramathibodi Hospital Mahidol University, Thailand2
Background
In order to classify bleeding risk in patient undergoing PCI, the Academic Research Consortium for High Bleeding Risk (ARC-HBR), which was a collaboration among leading research organizations, regulatory authorities, and physician-scientists from the United States, Asia, and Europe focusing on percutaneous coronary intervention–related bleeding, published the new set of criteria called “ARC-HBR” criteria. The ARC-HBR criteria was categorized in major and minor factors which composed of demographic data, comorbidities, bleeding history, current medications, and laboratory investigations. The patient at high bleeding risk was defined if one major or two minor criteria were met. There have been numerous studies attempting to validate the ARC-HBR criteria using their respective populations, including from US, Spain, Japan and even Thailand. A previously published trial, validating the criteria in the Thai population, demonstrated a statistically significant increase in primary bleeding outcomes at one year for high bleeding risk patients. It also exhibited a sensitivity of 70% and a specificity of 53.3% for BARC 3 or 5 bleeding at one year. Although it demonstrated a high negative predictive value, the positive predictive value was low. Consequently, we utilized the previous data to develop new modified criteria and validate them in a different Thai population. This study aimed to establish the accuracy of the new modified ARC-HBR criteria in Thai patients undergoing PCI.


Methods
The new criteria were modified from the original ARC-HBR criteria and data from Cox regression multivariate analysis of previous trial in Thai population. Age ≥ 75 years, which was the minor factor in the original criteria, was indicated being the strong predictor of primary endpoint; thus, it was transformed from minor to major factor in the criteria. On the contrary, because CKD was not the strong predictor and tended to be the protective factor, only severe CKD (eGFR <30 mL/min/ 1.73 m2) was used as one of the factors in these new criteria and transformed to minor criterion. This retrospective cohort study applied the new modified ARC-HBR definition to consecutive patients undergoing PCI in Ramathibodi hospital between September 1st, 2021 and March 31st, 2022. Patients were identified as HBR if at least one major criterion or two minor criteria were met. They were then followed up for one year. The primary outcome of this study was the risk of Bleeding Academic Research Consortium ( BARC) 3 or 5 bleeding at 1-year. Additionally, secondary outcomes were also evaluated, including the risk of gastrointestinal (GI) bleeding and ischemic outcomes—cardiovascular death, recurrent myocardial infarction (MI) and stent thrombosis.


Results
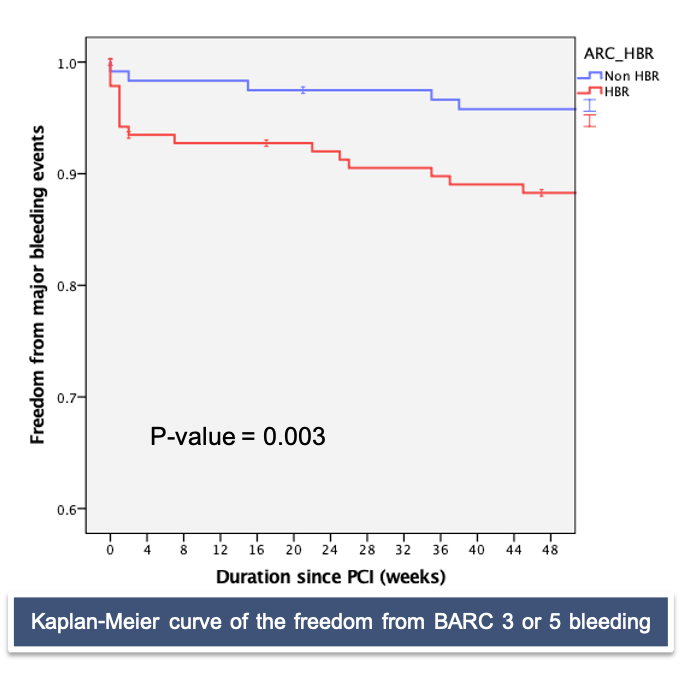
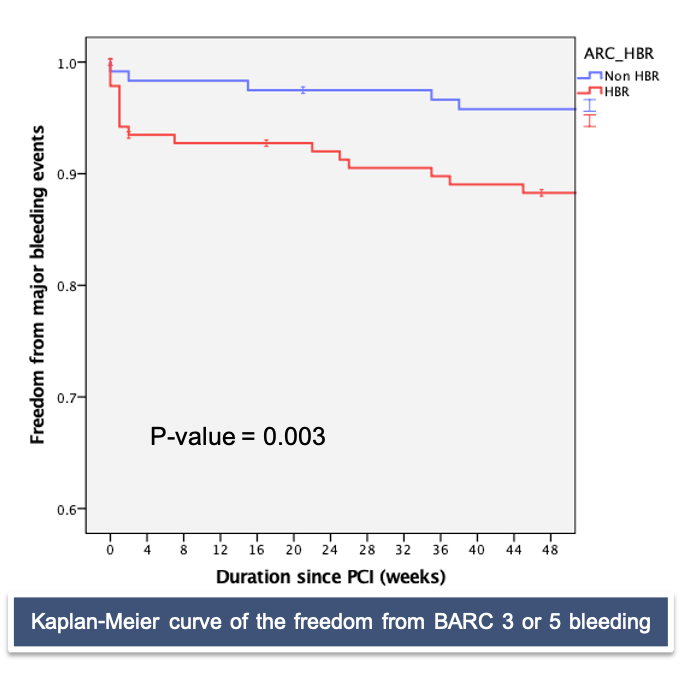
A total of 260 patients undergoing PCI at the Ramathibodi cardiac catheterization laboratory were included in the study and had complete follow-up at one year. 140 patients were categorized as HBR group (58%). The majority of the population in this trial were male (68.4%) and the median age was 73 years (62, 79). CCS accounted for 39.2% of the indications for PCI in our population, while ACS, including non-ST-segment elevation myocardial infarction (NSTEMI) and ST-segment elevation myocardial infarction (STEMI) account for 35%. Additionally, the femoral artery access site (70%) was preferred over radial access for performing PCI in our center. Patients undergoing PCI received coronary drug-eluting stents (DES) in 97.7% of cases. The primary bleeding endpoint, BARC 3 or 5 bleeding at 1-year occurred in 15% of patients in the HBR group and in 4.2% of the non-HBR group (HR [95%CI]: 4.06 [1.48-11.13], p = 0.004). The difference was primarily driven by BARC 3 bleeding (13.6% vs 4.2%. p=0.009). Furthermore, the Kaplan-Meier curve was used to estimate the freedom from BARC 3 or 5 bleeding at 1-year, which was significantly different between patients with HBR and non-HBR (85% vs. 95.8%, p=0.003). On the contrary, there is no statistical difference among ischemic outcomes; all-cause death (5.7% vs. 1.7%, p=0.091), cardiac death (2.9% vs. 0.8%, p=0.236), recurrent MI (2.9% vs.1.7%, p=0.524), stent thrombosis (0.7% vs. 0.8%, p=0.913) and stroke (0% vs. 2.9%, p=0.062). The ROC curve analysis showed that the new modified ARC-HBR criteria had a sensitivity of 80.8% and a specificity of 50.9% in predicting BARC 3 or 5 bleeding at 1-year.




Conclusion
The new modified ARC-HBR definition, adjusted based on previous data from the Thai population undergoing PCI, successfully identified patients at an increased risk of the BARC 3 or 5 bleeding endpoint at 1-year. Additionally, it demonstrated high sensitivity with intermediate specificity.

