Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-021
Re-Evaluating the Role for Revascularisation in Stable Coronary Disease: A Systematic Review and Meta-Analysis
By Nushrat Sultana, Nitesh Nerlekar, Anthony White
Presenter
Nushrat Sultana
Authors
Nushrat Sultana1, Nitesh Nerlekar1, Anthony White1
Affiliation
Monash Heart, Victorian Heart Hospital, Australia1
View Study Report
TCTAP A-021
Clinical Trials & Science
Re-Evaluating the Role for Revascularisation in Stable Coronary Disease: A Systematic Review and Meta-Analysis
Nushrat Sultana1, Nitesh Nerlekar1, Anthony White1
Monash Heart, Victorian Heart Hospital, Australia1
Background
Conventional strategies for the management of stable coronary artery disease (CAD) often favour an initial revascularisation approach. Whether there is improved mortality and reduction in adverse cardiovascular outcomes when compared to optimal medical therapy (OMT) alone remains controversial, given the latter can be underutilised and sub-optimally administered in clinical settings. This meta-analysis aims to provide a nuanced perspective on the comparative impacts of routine revascularisation and OMT on long-term mortality in stable CAD.
Methods
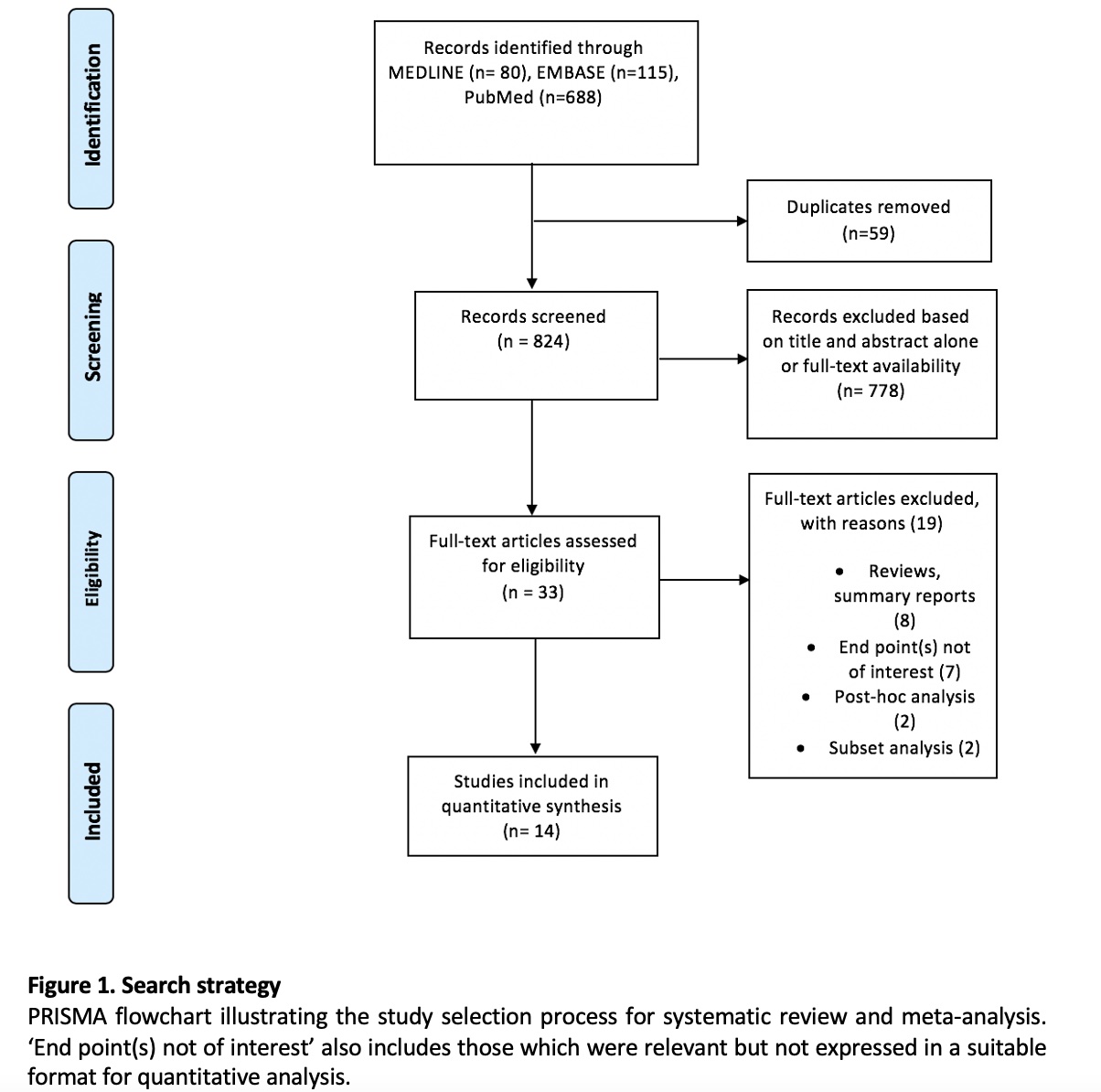
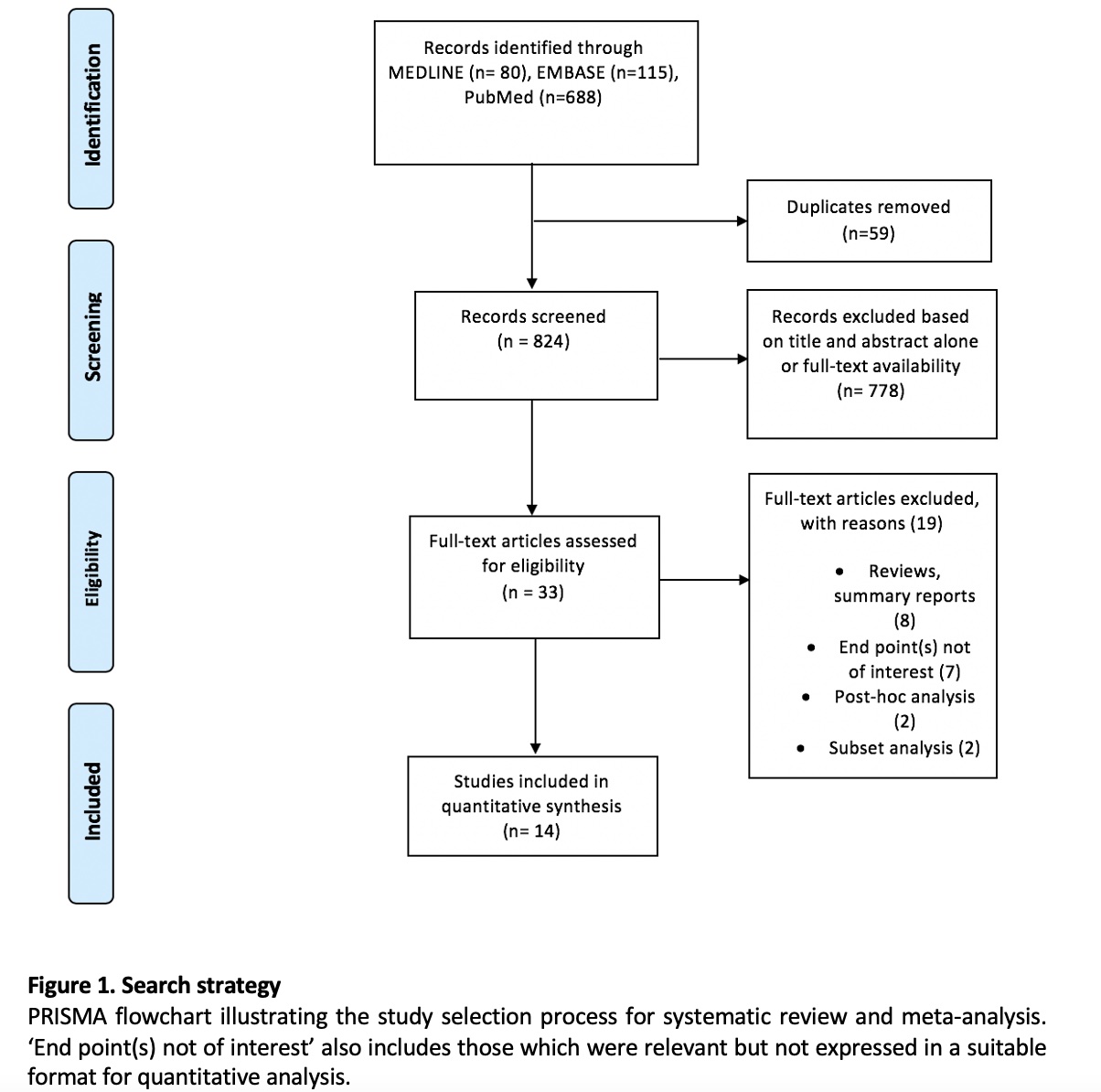
A systematic search was conducted using the PUBMED, MEDLINE and EMBASE databases. Results were limited to randomised controlled trials (RCT) comparing an initial revascularisation approach (percutaneous coronary intervention (PCI), coronary artery bypass grafting (CABG)) to OMT alone. The outcomes of interest were mortality (both all-cause and cardiac), incidence of myocardial infarction (MI), unplanned revascularisation, hospitalisation for cardiac reasons and stroke. Inclusion criteria across all studies comprised of patients with symptomatic stable angina, or those who demonstrated evidence of ischaemia on stress testing or had documented disease with at least one stenosis (above 70%) in a major coronary artery on angiography. Patients with significantly reduced left ventricular ejection fraction (below 35%) were excluded from all trials. Random-effects meta-analysis was performed using the programming language R. Results are reported as odds ratio (OR) with 95% confidence intervals (95% CI). Study heterogeneity is determined by the I2 statistic.
Results
824 articles were screened for eligibility, with 33 full-text papers retrieved for potential inclusion and detailed evaluation. Of this group, 14 RCTs met criteria for quantitative analysis. Quantitative analysis included 15,081 participants, of whom 7,734 had undergone revascularisation with PCI (80.2%) or CABG (19.8%). The remaining patients were treated with OMT (48.8%). Median follow-up ranged between twelve months and five years. Thirteen of the fourteen trials selected for meta-analysis reported the incidence of all-cause mortality and MI. The incidence of mortality did not vary significantly between an approach involving revascularisation with medical therapy versus medical therapy alone (13 studies, OR, 0.99; 95% CI, 0.87 – 1.12; p = 0.77; I2 = 0%). It was a similar case for MI (OR, 0.94; 95% CI, 0.81 – 1.09; p= 0.35; I2 = 10%). Ten reported the incidence of cardiac death, which demonstrated no significant difference between either approach also (OR, 0.97; 95% CI, 0.81 – 1.15; p = 0.87, I2 = 0%). The outcomes of unplanned revascularisation and hospitalisations for cardiac reasons demonstrated benefit of initial revascularisation (10 studies, OR, 0.75; 95% CI, 0.50 – 1.14; p < 0.01, I2 = 83%), (6 studies, OR, 0.68; 95% CI, 0.39 – 1.20; p < 0.01; I2 = 85%) although with higher heterogeneity. Finally, for the outcome of stroke, the results were suggestive, but not significant for an initial conservative strategy of OMT alone (8 studies, OR, 1.48; 95% CI, 0.84 – 2.62, p = 0.17, I2 = 33%).


Conclusion
Compared to OMT alone, an initial revascularisation strategy demonstrated similar outcomes for all-cause and cardiac mortality, and MI. However, rates of unplanned revascularisation and hospitalisation for cardiac reasons were significantly lower among the initial revascularisation cohort. Incidence of stroke was lower within the OMT group, although this lacked statistical significance. Further evaluation of subjective symptoms such as angina and exercise tolerance would be useful in providing an individualised approach in clinical settings. Angina questionnaires and scoring systems were not expressed in a standardised manner across the trials, precluding accurate quantitative analysis. Extended follow up will be beneficial to observe the impact of nonfatal events on overall mortality.

