Lots of interesting abstracts and cases were submitted for TCTAP 2024. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-048
Impact of Minimal Invasive Extracorporeal Circulation in Coronary Artery Bypass Surgery: Meta-Analysis
By Ameer Fadhil Abbas Al Wssawi, Armand Gumera, Ali Saad Al-Shammari, Hasnaa Abdelsamad, Hashim Talib Hashim
Presenter
Armand Gumera
Authors
Ameer Fadhil Abbas Al Wssawi1, Armand Gumera2, Ali Saad Al-Shammari3, Hasnaa Abdelsamad4, Hashim Talib Hashim5
Affiliation
University of Al-Qadisiyah, Iraq1, University of Melbourne, Australia2, Al-Kindy general hospital, Iraq3, Ain Shams University, Egypt4, University of Warith Al-Anbiyaa, Iraq5
View Study Report
TCTAP A-048
Mechanical Circulatory Support
Impact of Minimal Invasive Extracorporeal Circulation in Coronary Artery Bypass Surgery: Meta-Analysis
Ameer Fadhil Abbas Al Wssawi1, Armand Gumera2, Ali Saad Al-Shammari3, Hasnaa Abdelsamad4, Hashim Talib Hashim5
University of Al-Qadisiyah, Iraq1, University of Melbourne, Australia2, Al-Kindy general hospital, Iraq3, Ain Shams University, Egypt4, University of Warith Al-Anbiyaa, Iraq5
Background
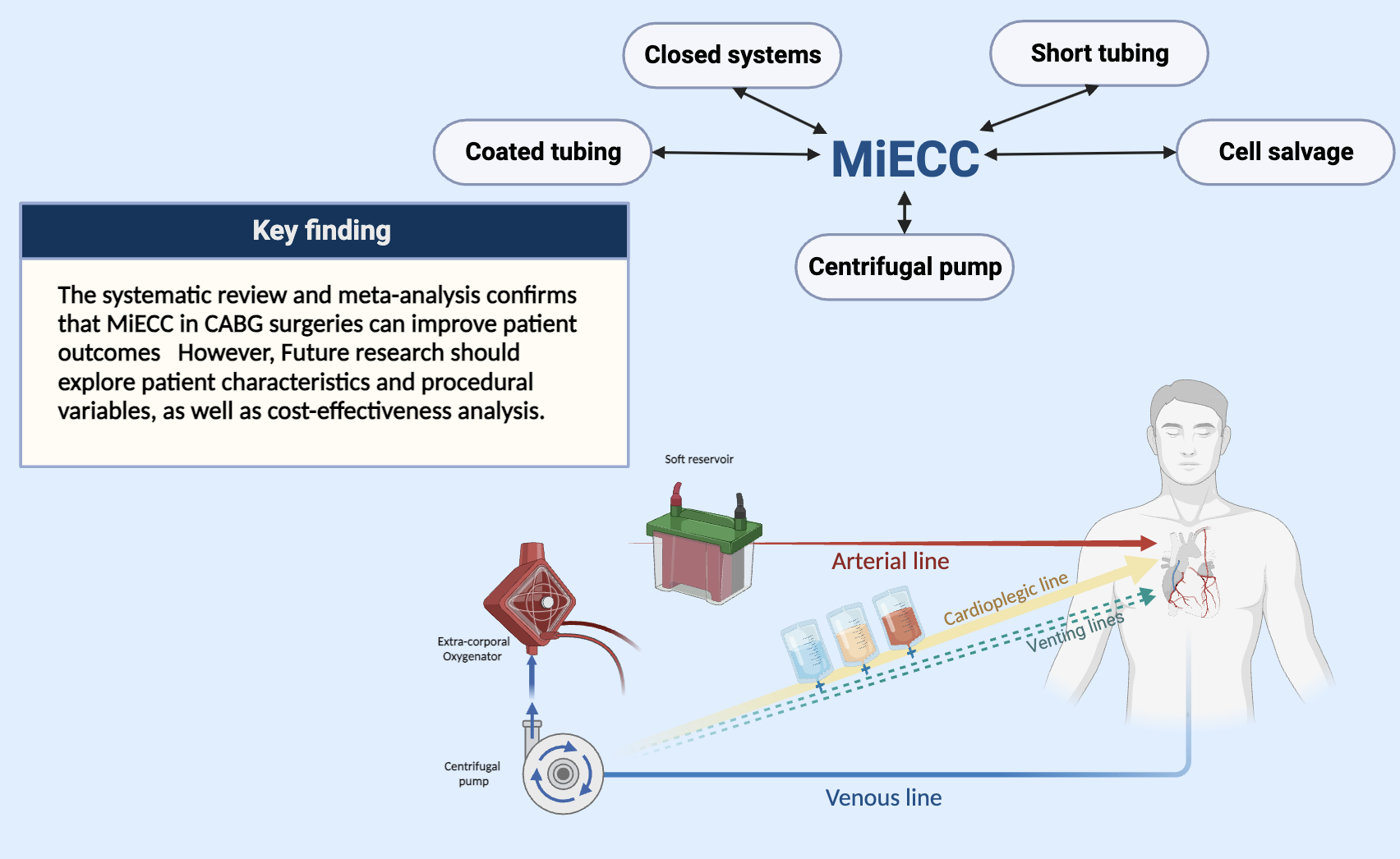
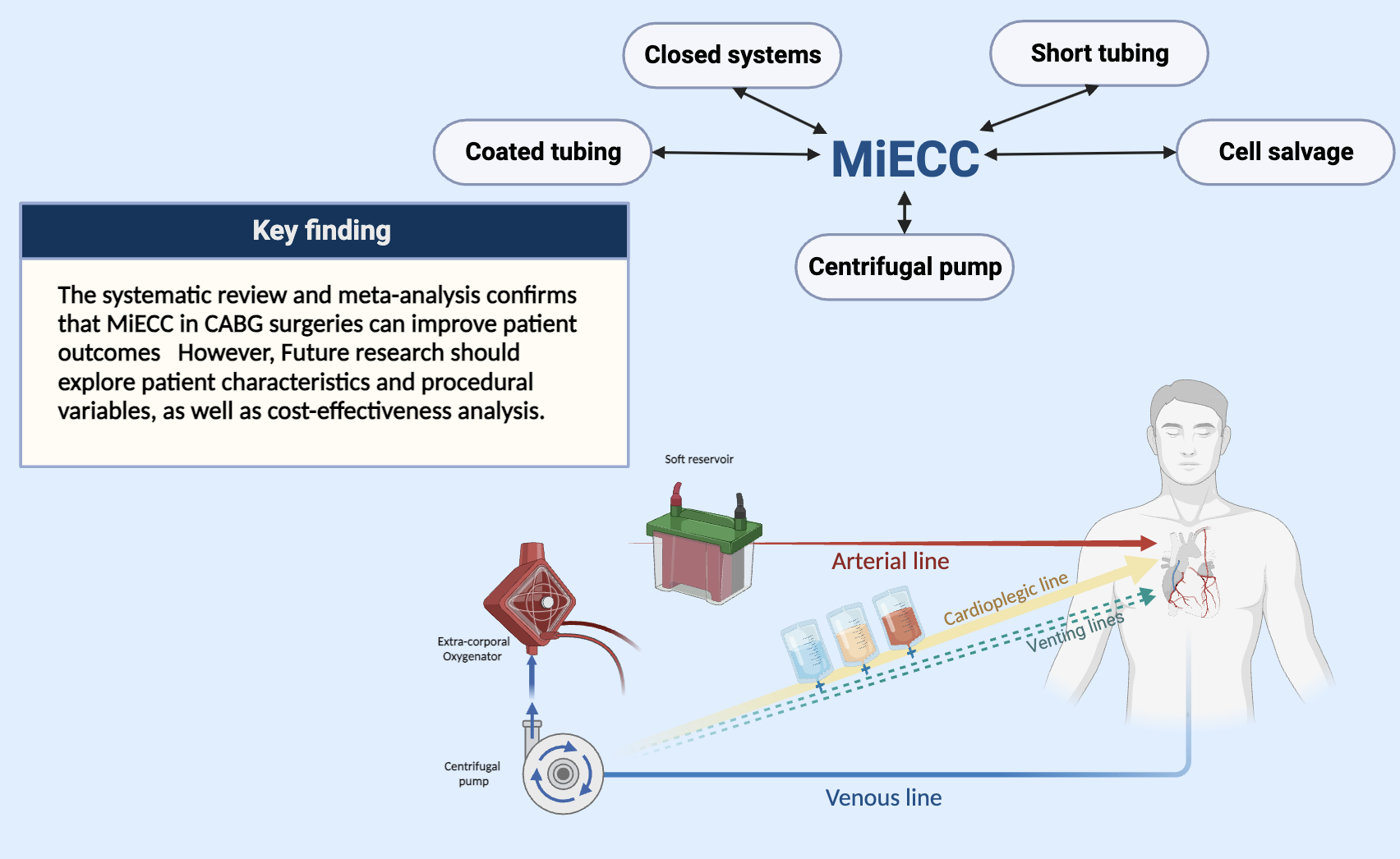
Coronary artery disease (CAD) continues to be a leading global health issue, often treated with coronary artery bypass grafting (CABG), which implements conventional approaches that have significant drawbacks. Minimal invasive extracorporeal circulation (MiECC) has emerged as a promising alternative. However, heterogeneous research has led to clinical uncertainty.ObjectivesTo evaluate and compare the efficacy and safety of MiECC with traditional approaches in coronary artery bypass grafting (CABG). The review aims to address the key question: "Do patients undergoing CABG with MiECC experience superior outcomes compared to those using traditional perfusion techniques?
Methods
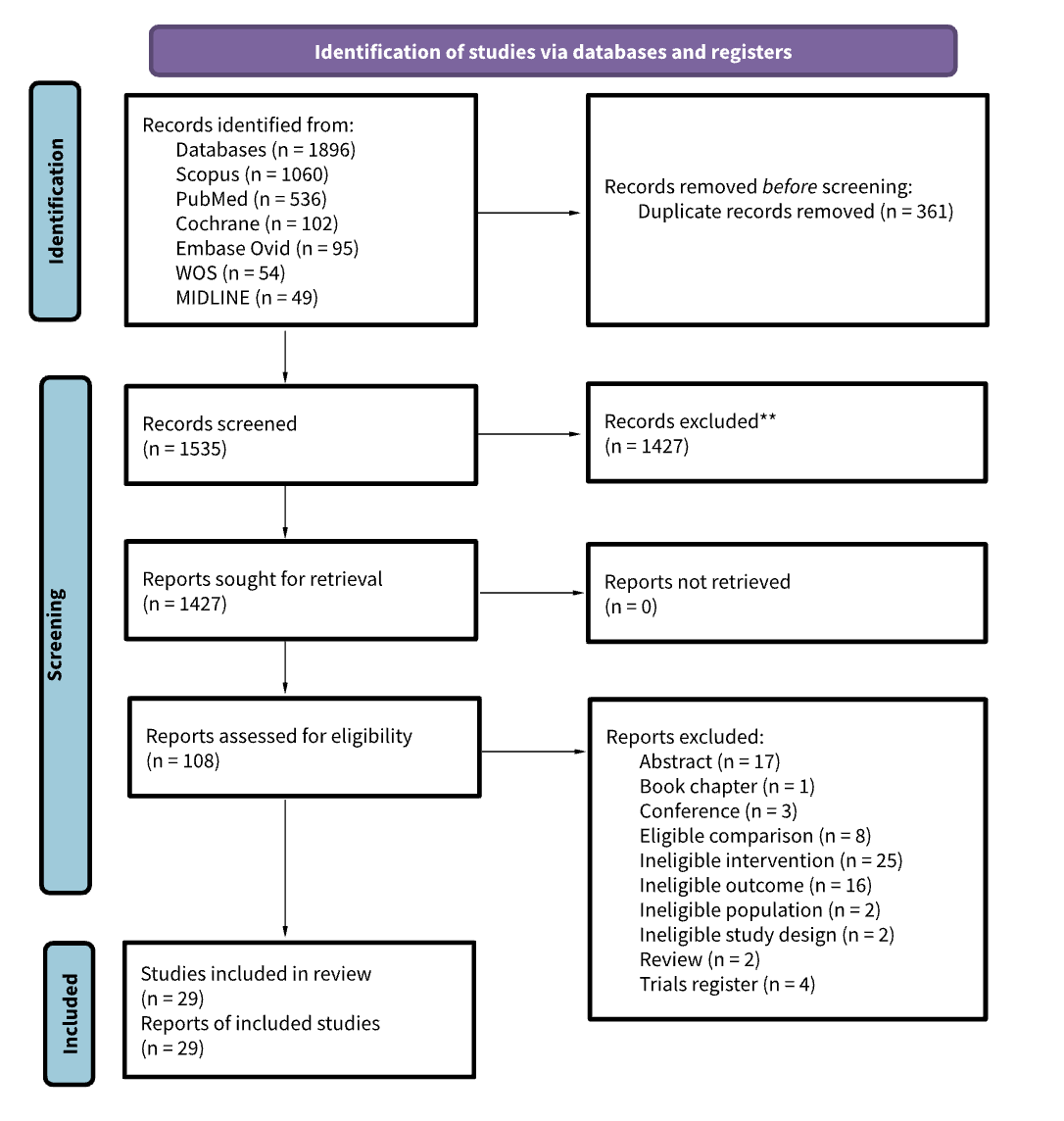
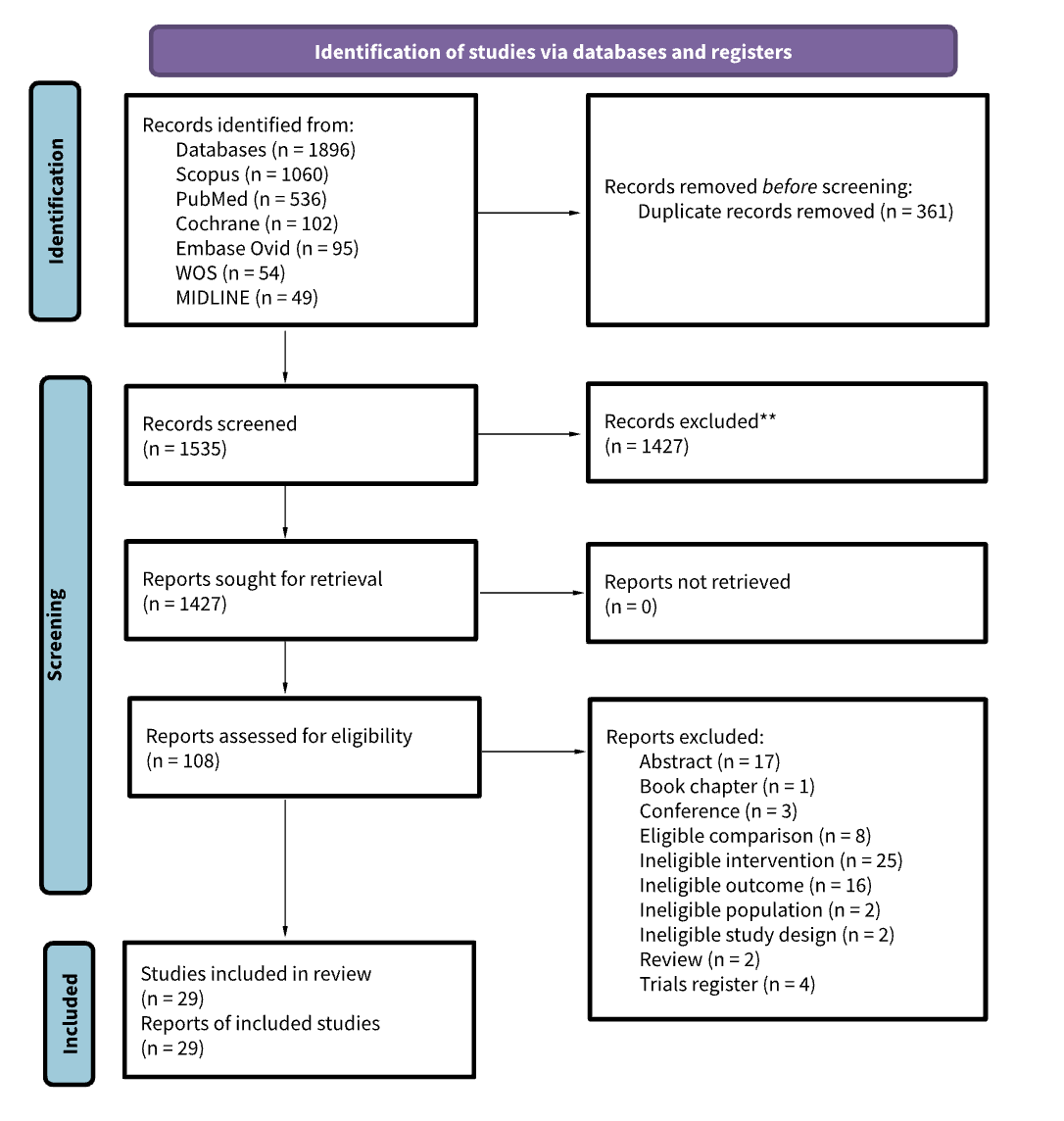
Search methods: Articles were searched using medical databases including PubMed, Medline, Scopus, Embase, Web of Science, and The Cochrane Central Register Of Controlled Trials (CENTRAL) from the database's inception until the 18th of August 2023.Selection criteria: We included English-language randomized controlled trials and cohort studies that looked for adults doing Coronary Artery Bypass Grafting(CABG) surgery and receiving the Minimally Invasive Extracorporeal Circulation technique.Data collection and analysis: A total of 1896 abstracts were screened, followed by full-text for 108 articles checked after duplicates and not related subjects removal, using PRISMA guidelines. Finally, a total of 29 studies were included for data extraction in our systematic review.Data analysis was done using RevMan 5.4 software. The risk of bias, sensitivity analysis, and heterogeneity test were done using Cochrane tools for systematic reviews.
Results
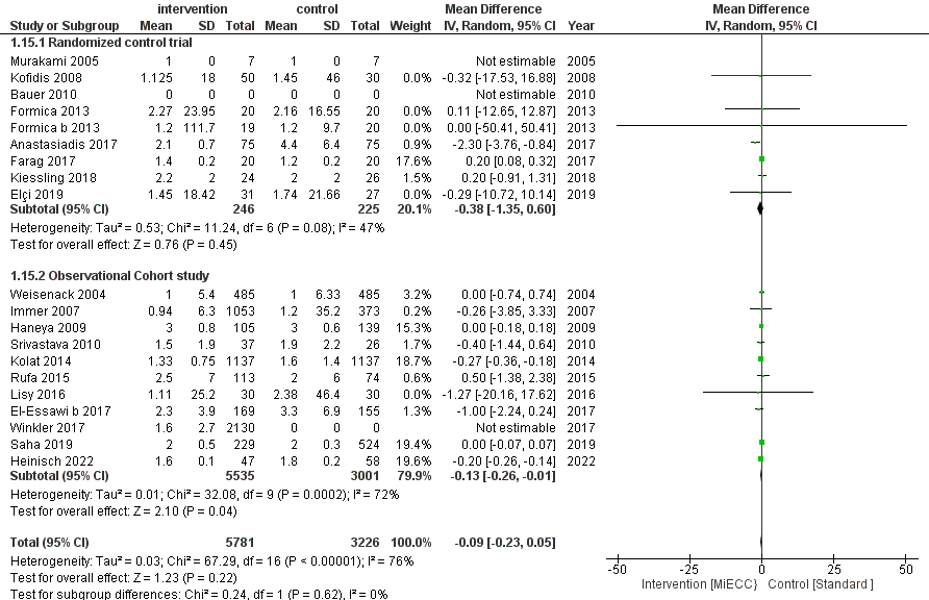
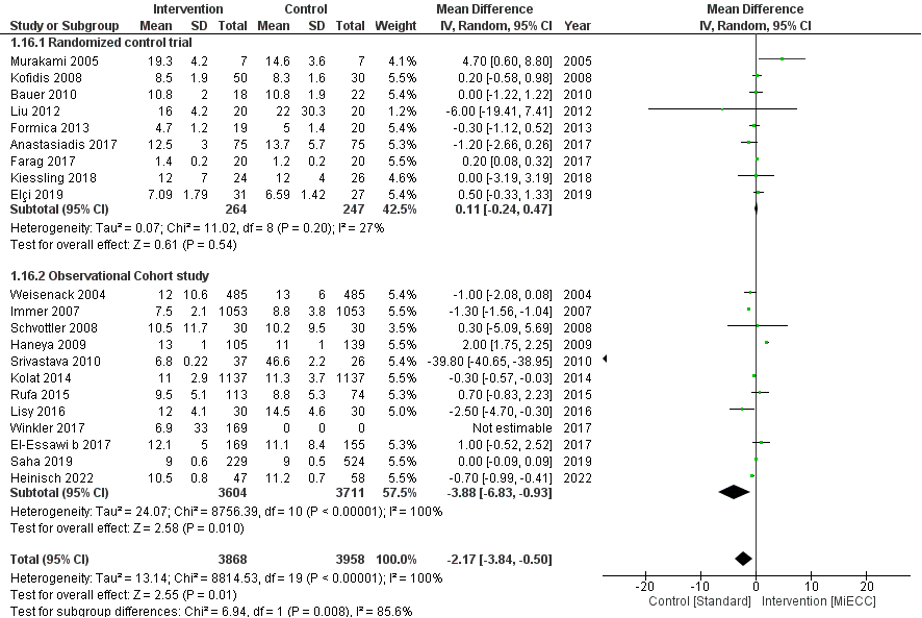
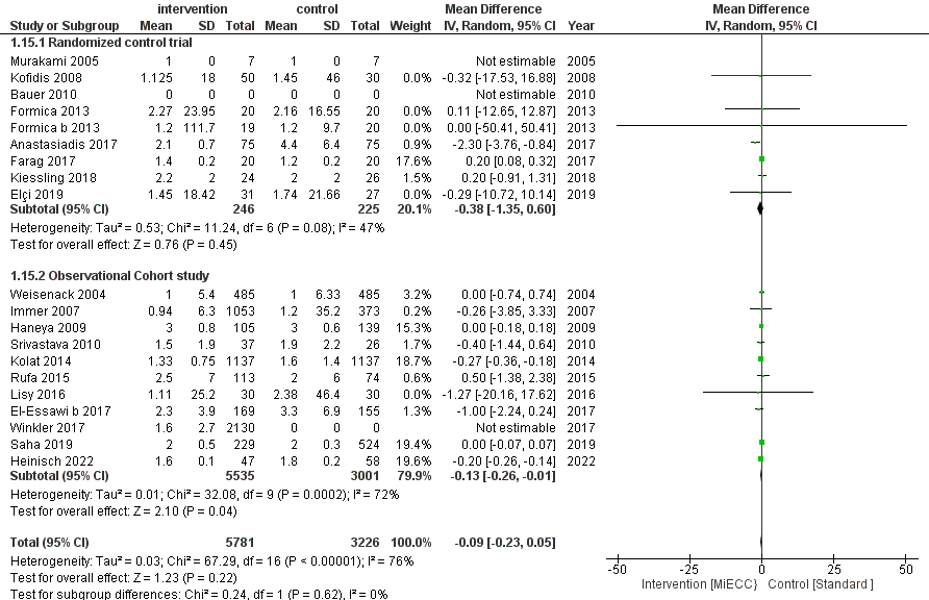
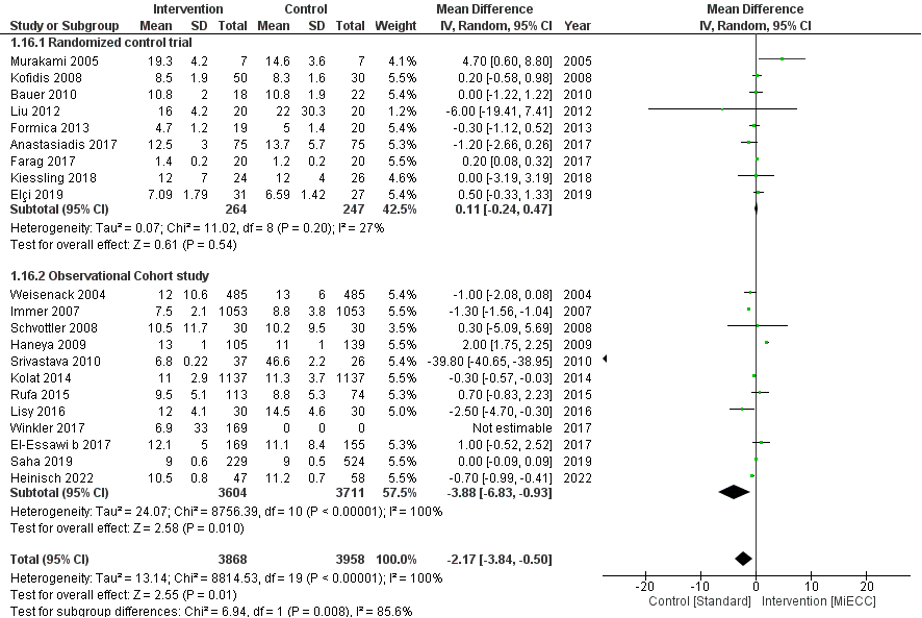
Main results: The primary outcomes for this study were: The duration of Intensive Care Unit (ICU), hospital stay, Cardiopulmonary Bypass (CPB), ventilation, and cross-clamp time of MiECC versus the standard method, the secondary outcomes were the Extracorporeal circuit(ECC), aortic clamp and operation time, intraoperative blood transfusion, postoperative blood, and drainage loss, atrial fibrillation incidence, myocardial ischemia, stroke, total and in-hospital mortality rates of MiECC versus the standard approach. Regarding the primary outcomes, the overall significant differences were shown in the ventilation time, MiECC technique was associated with a reduction in the total hours, Mean difference (MD): -3.28; 95% confidence interval, -5.7, -0.87; p=0.008; Z=2.67; I2= 92%. In-hospital stay days were decreased in the MiECC group, MD:-2.17, 95%CI, (-3.84, -0.5), p=0.01. CPB time was increased in the standard group compared to the MiECC group, MD: 5.81, 95% CI: 5.81(0.95, 10.66). Overall cross-clamping time was also decreased but not significantly compared to the standard group, MD: -0.39; 95% CI, (-2.84, 2.07), P=0.76. The mean difference reduction in ICU days stays was -0.09 [95% CI, -023, 0.05]; P =0.22). Regarding the secondary outcomes, there was a significant overall difference in ECC hours between the two groups, MD: 5.71; 95%CI: (0.02, 11.39), p-value=0.05. Atrial fibrillation complication rate was higher in the standard group: 0.36; 95%CI: 0.36(0.2, 0.66), p-value=0.05. Myocardial ischemia complication rate was higher in the standard group, MD: 0.51; 95%CI, (0.27, 0.97), p-=0.04. The stroke complication rate was higher in the standard group compared to the MiECC group, MD: 0.35; 95%CI:0.16, 0.78), P=0.01. The in-hospital overall mortality rate was higher in the standard group but did not show significance: 0.61; 95%CI (0.33, 1.13), p=0.12. Postoperative drainage loss was not significantly different, MD: -136.71; 95%CI: (-337.17, 63.76), p =0.18. MiECC was linked to an increase in postoperative blood loss MD: -33.26, 95%CI: (102.1, 35.59), p=0.34.


Conclusion
The systematic review and meta-analysis confirm that MiECC in CABG surgeries can be beneficial over standard methods in multiple outcome measures. However, it is crucial to interpret these results carefully, as many studies displayed a low risk of bias across several domains. MiECC may be advantageous in clinical practice, potentially enhancing patient outcomes and reducing healthcare costs. However, implementing MiECC should be considered in the context of individual patient's medical condition and existing guidelines. The review identifies both potential advantages and gaps in the body of evidence concerning the use of MiECC in CABG surgeries. The utilization of MiECC was linked to shorter durations of ICU stay, hospital stay, and mechanical ventilation time, although the findings exhibited some variability in sensitivity analyses. The review highlights the need for more high-quality, effective RCTs with rigorous blinding and allocation protocols. Future research should investigate the reasons for observed heterogeneity in results, possibly exploring patient characteristics or procedural variables that may affect outcomes. A cost-effectiveness analysis of MiECC compared to standard methods can add another dimension to this line of research.

