Seung-Jung Park, MD
Asan Medical Center, Republic of Korea
Seung-Jung Park, MD (Asan Medical Center, Korea) sheds light on following consequences:
For all ischemic lesions with favorable anatomy for percutaneous coronary intervention (PCI), consider guideline-directed medical therapy with complete revascularization with drug-eluting stent (DES).
For unfavorable anatomy for PCI and low ejection fraction (EF), and/or diabetic patients, consider optimal medical treatment with coronary artery bypass grafting (CABG) first.
Further studies on physiology and image-supported contemporary PCI versus CABG in multi-vessel disease (MVD) patients with ischemic cardiomyopathy (EF <50%) or diabetes are needed.
Park presented his approach and future perspective on MVD revascularization at the 28th TCTAP 2023 on May 7.
In the 2021 ACC/AHA/SCAI guideline for coronary artery revascularization, CABG is still recommended as Class I (EF <35%), lla (EF 35-50%) in low EF with MVD. But in EF>50% with MVD, any revascularization is recommended as Class llb (CABG was downgraded to Class llb compared with the 2011 CABG guideline).
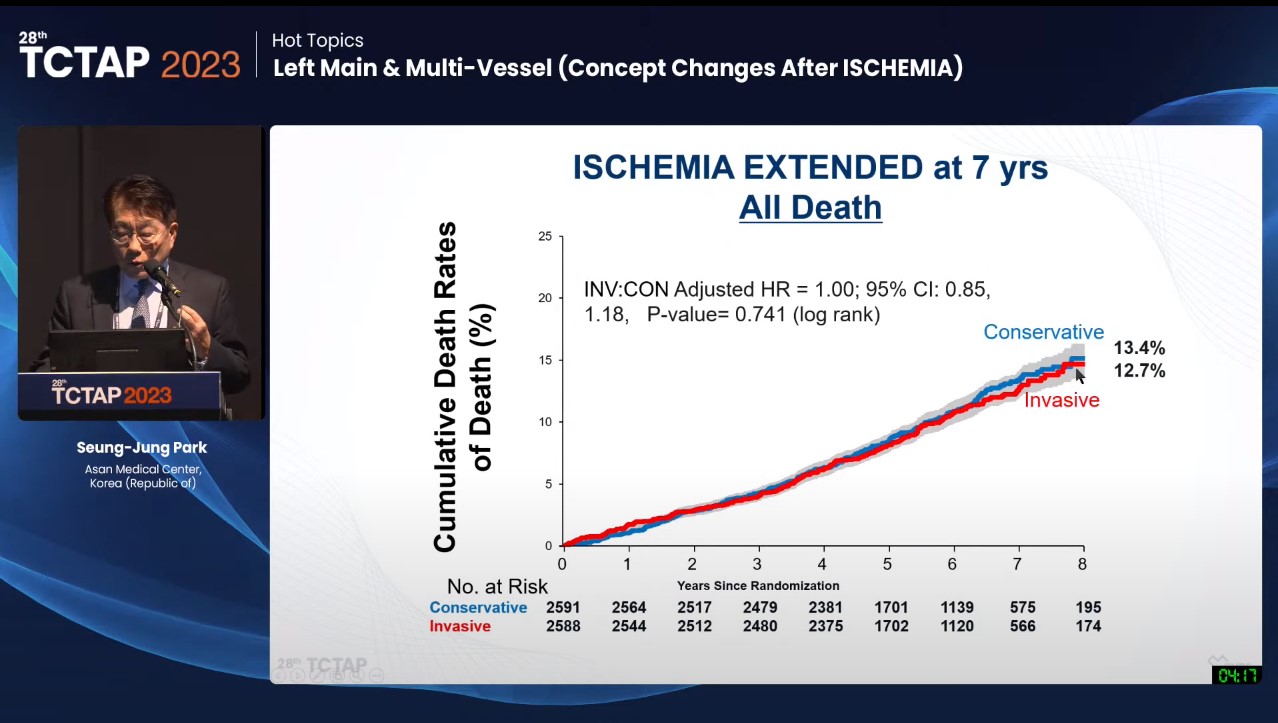
According to the ISCHEMIA trial, which became evidence of the downgrade, there were no survival and ischemic event benefits in the invasive strategy group (PCI or CABG) compared with the conservative strategy group in patients with moderate or severe ischemia (Figure 1).
Comparing CABG and PCI in MVD, CABG is recommended as Class Ia in diabetic 3 vessel disease (SYNTAX I, BARI 2D, and FREEDOM trials), and PCI may be considered as Class lla for poor CABG candidates based on the long-term outcomes of the BEST trial.
“However, we have very limited data. For future perspectives, we have to consider physiology and image-supported contemporary PCI. It would be a totally different world!” Park said. This was because most of the previous studies were performed using the 1st generation DES and with limited concepts for physiology and imaging during PCI.
The SYNTAX ll trial showed the impact of physiology and imaging-guided PCI on revascularization outcomes for MVD. In the PCI group of the SYNTAX ll trial, physiology assessment (instantaneous wave-free ratio [iFR]/fractional flow reserve [FFR]) was performed in 75.5% and imaging (intravascular ultrasound [IVUS]) assessment in 84.1%. This study showed similar two-year outcomes for major adverse cardiovascular and cerebrovascular events (MACCE) between the SYNTAX ll PCI and SYNTAX I CABG trials (13.2% vs 15.1%, p=0.73) (Figure 2).
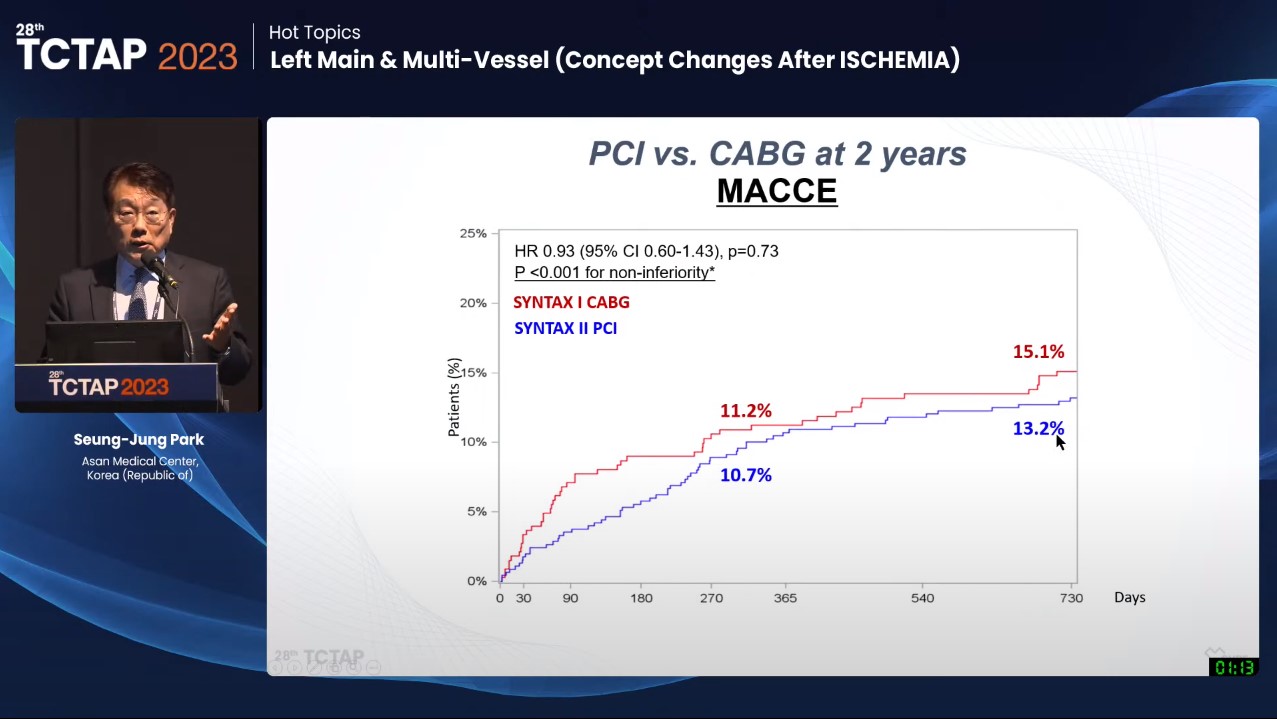
“Contemporary PCI (physiology and Image supported) is a totally different strategy and has totally different clinical outcomes compared to conventional angio-guided PCI. Still, we have no data about contemporary PCI vs CABG for MVD patients with ischemic cardiomyopathy (EF<50%) or diabetes. Further research is needed.” Park said.
Hot Topics
Left Main & Multi-Vessel (Concept Changes After ISCHEMIA)
Sunday, May 7, 3:30 PM - 4:20 PM
Presentation Theater 1, Vista 3, B2
Edited by

Gyung-Min Park, MD
Ulsan University Hospital, Korea (Republic of)

