Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-014
Ultra Low Contrast IFR-IVUS Guided PCI
By Dewi Ayu Paramita, Billal Patel
Presenter
Dewi Ayu Paramita
Authors
Dewi Ayu Paramita1, Billal Patel2
Affiliation
Siloam Hospitals Balikpapan, Indonesia1, Gleneagles Jpmc, Brunei Darussalam2,
View Study Report
TCTAP C-014
CORONARY - Acute Coronary Syndromes (STEMI, NSTE-ACS)
Ultra Low Contrast IFR-IVUS Guided PCI
Dewi Ayu Paramita1, Billal Patel2
Siloam Hospitals Balikpapan, Indonesia1, Gleneagles Jpmc, Brunei Darussalam2,
Clinical Information
Patient initials or Identifier Number
BZ
Relevant Clinical History and Physical Exam
A 46 years old man was referred to our hospital as NSTEMI. Patient has typical chest pain and the risk factor were DM, hypertension noncompliant with medication, and CKD. Patient has history of recurrent PCI and stents including ISR which his last angiography procedure was done in June 2022. From physical examination, patient's blood pressure was 150/90 mmHg. Chest examination revealed that patient had normal heart sound and crackles in bottom of lung field.
Relevant Test Results Prior to Catheterization
ECG of this patient showed ST depression in anterolateral leads. From laboratory result, the troponin was 900, creatinine was 524, and blood glucose was 14.
Relevant Catheterization Findings
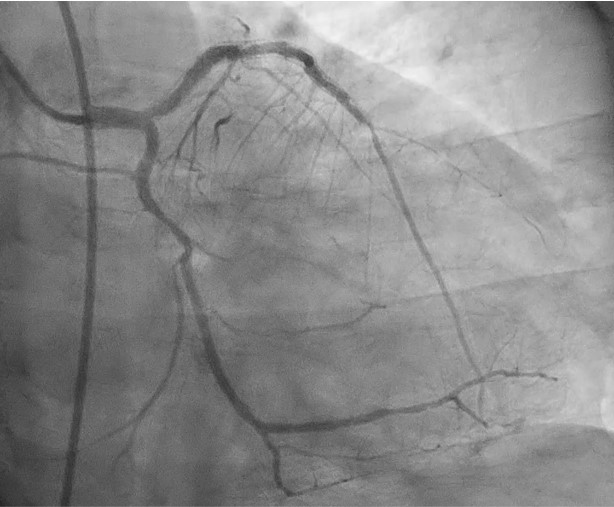
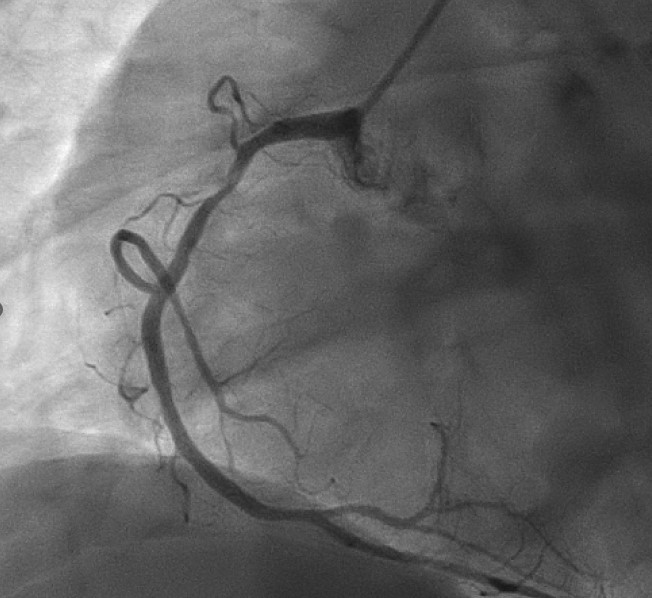
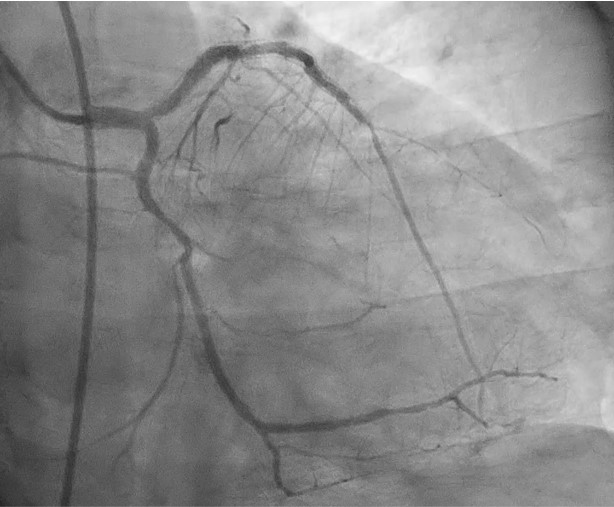
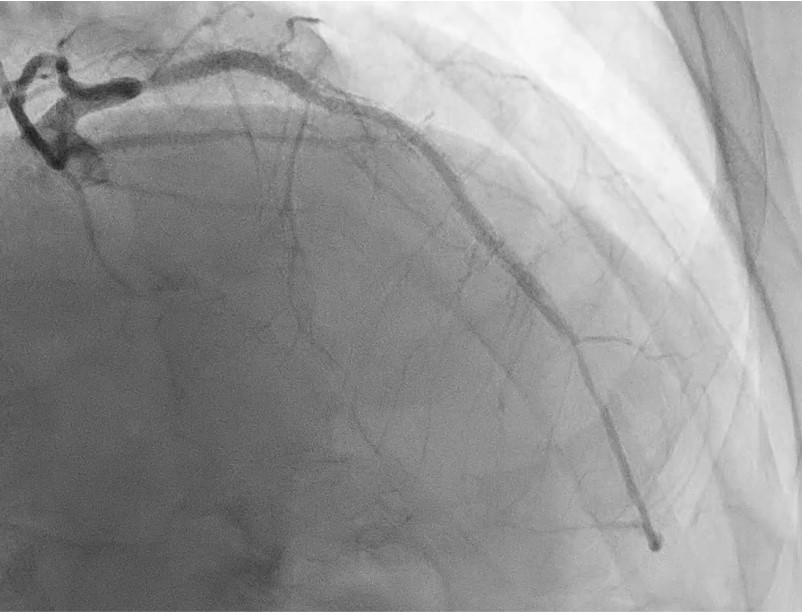
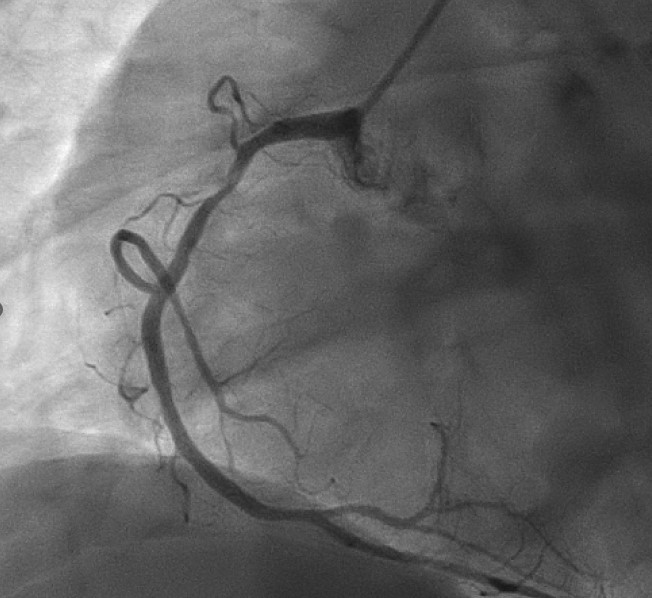
Angiography procedure was done via right femoral artery with ultrasound guided access as patient's right radial artery was impalpable. Angiogram showed that this patient has severe ostial LAD, severe ISR, severe stenosis beyond distal stent edge; severe stenosis in mid LCx (worse than before); and severe stenosis in proximal RCA
Interventional Management
Procedural Step
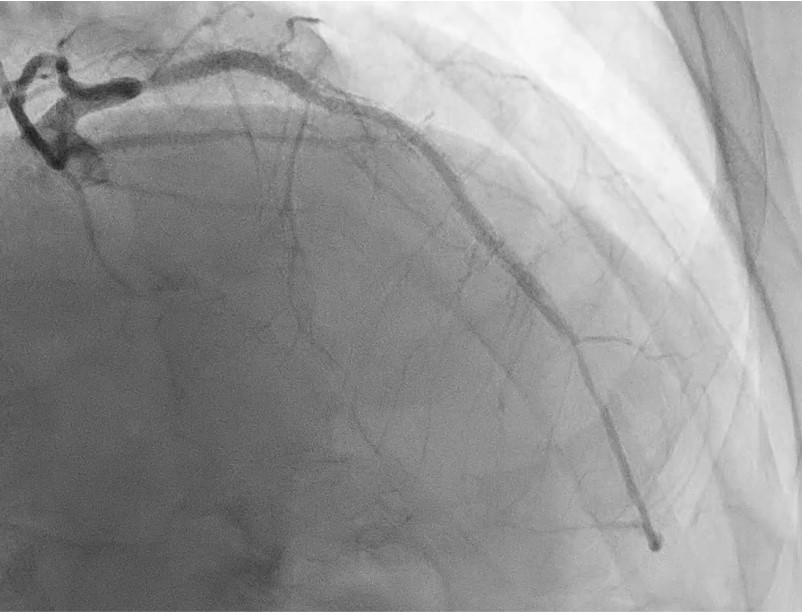
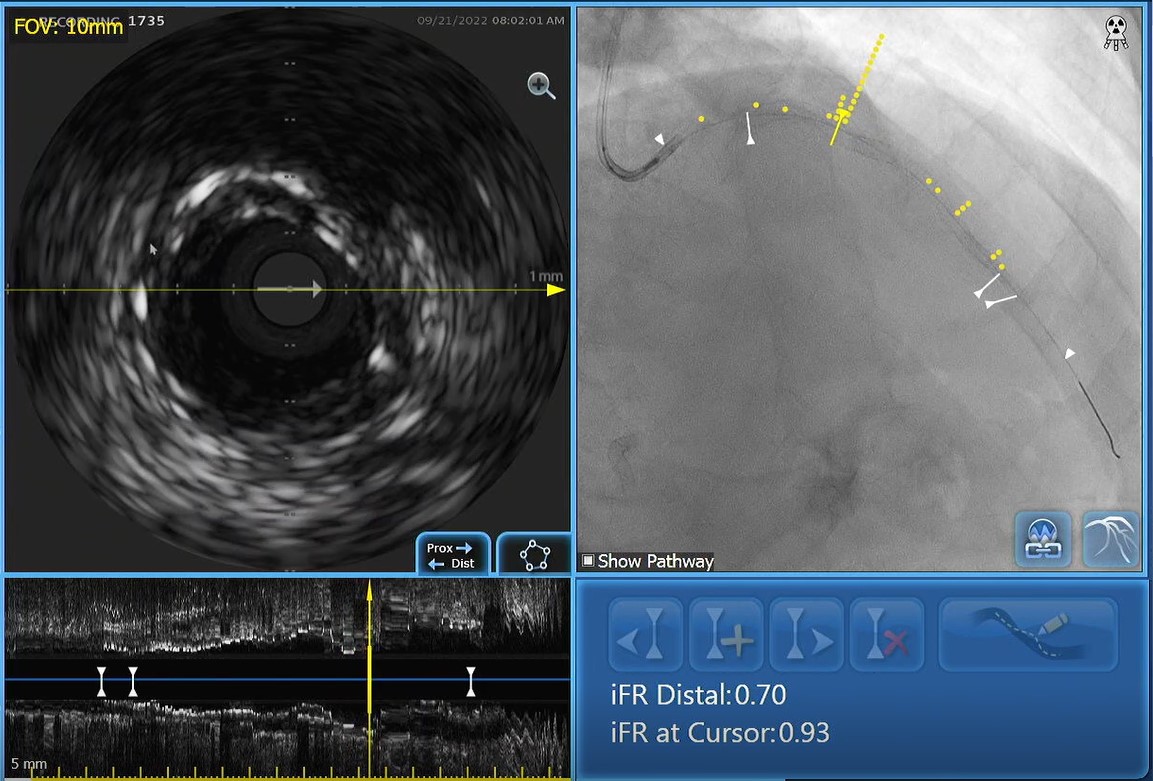
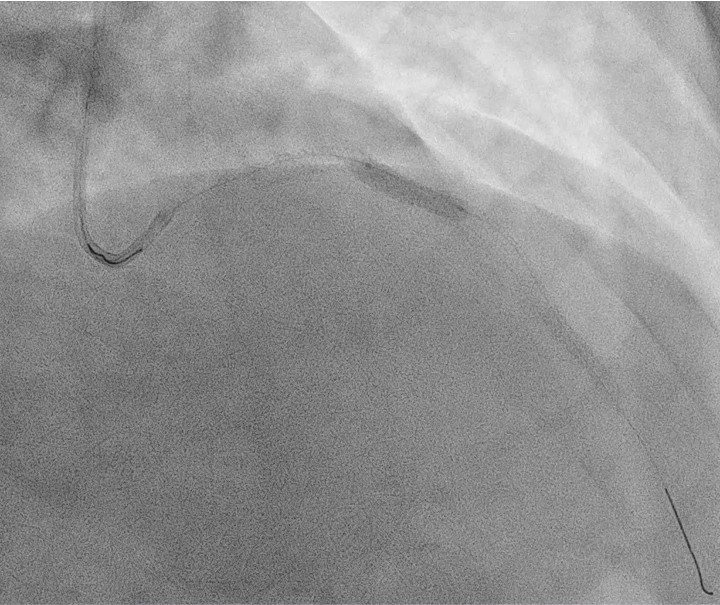
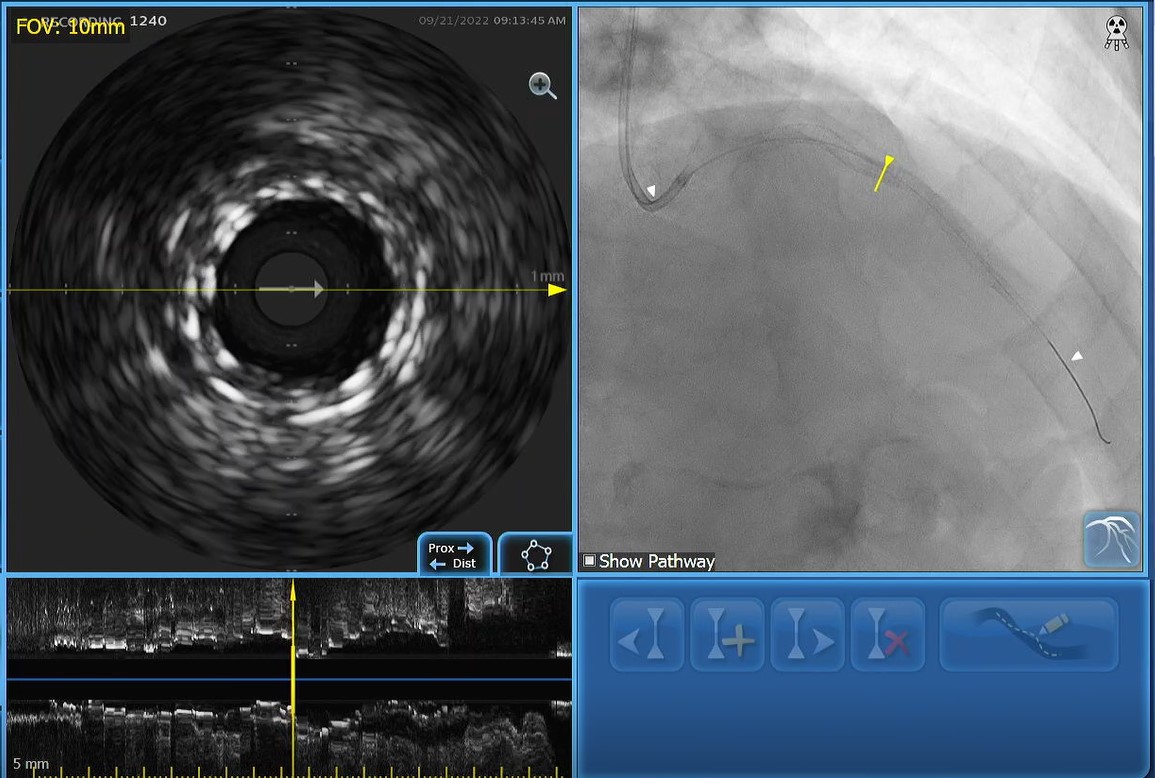
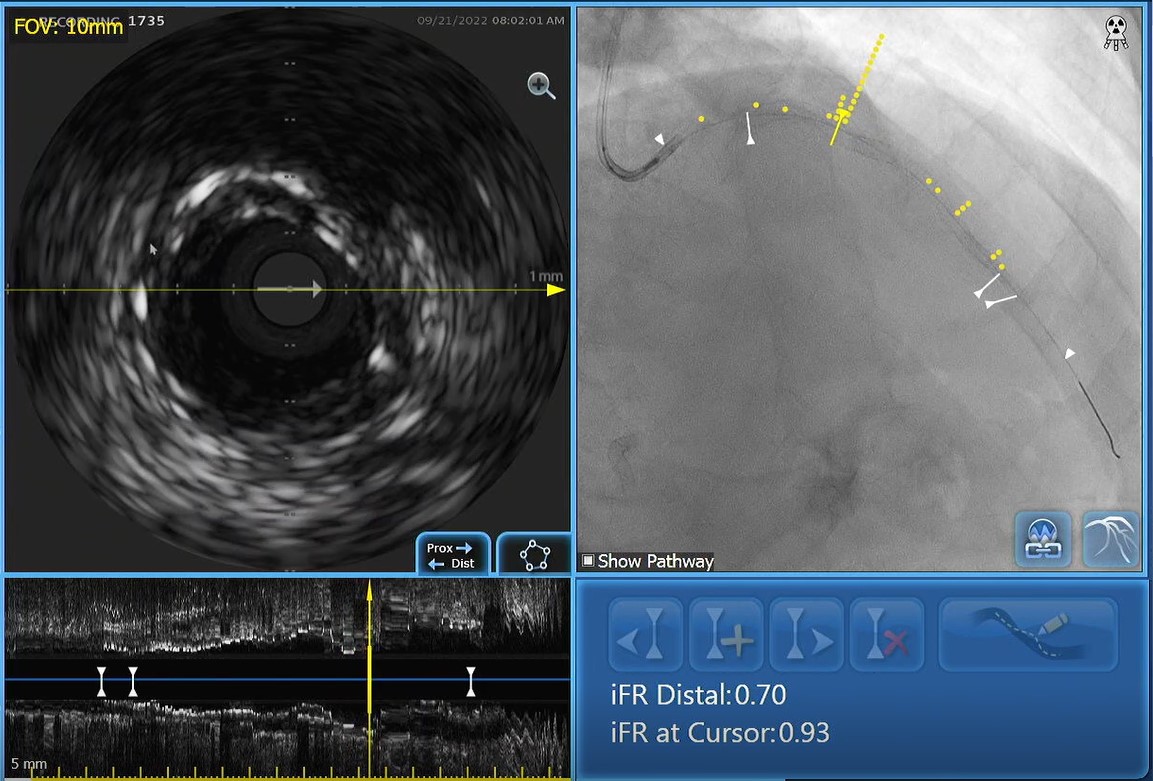
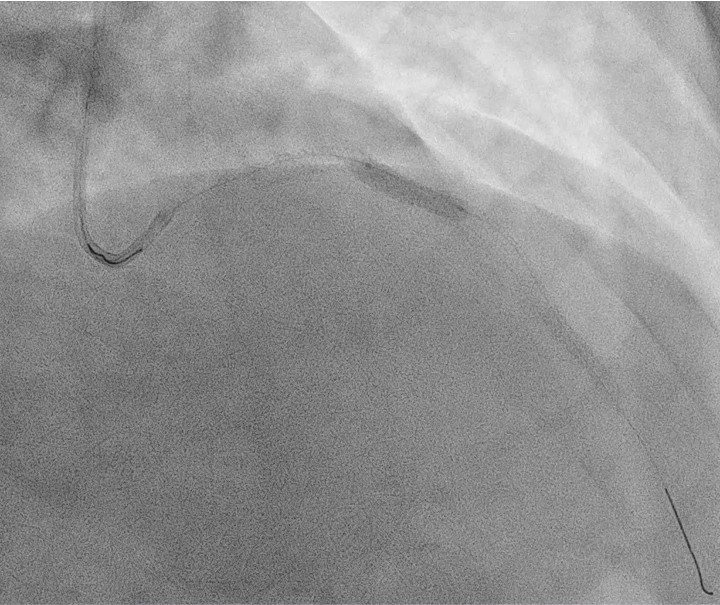
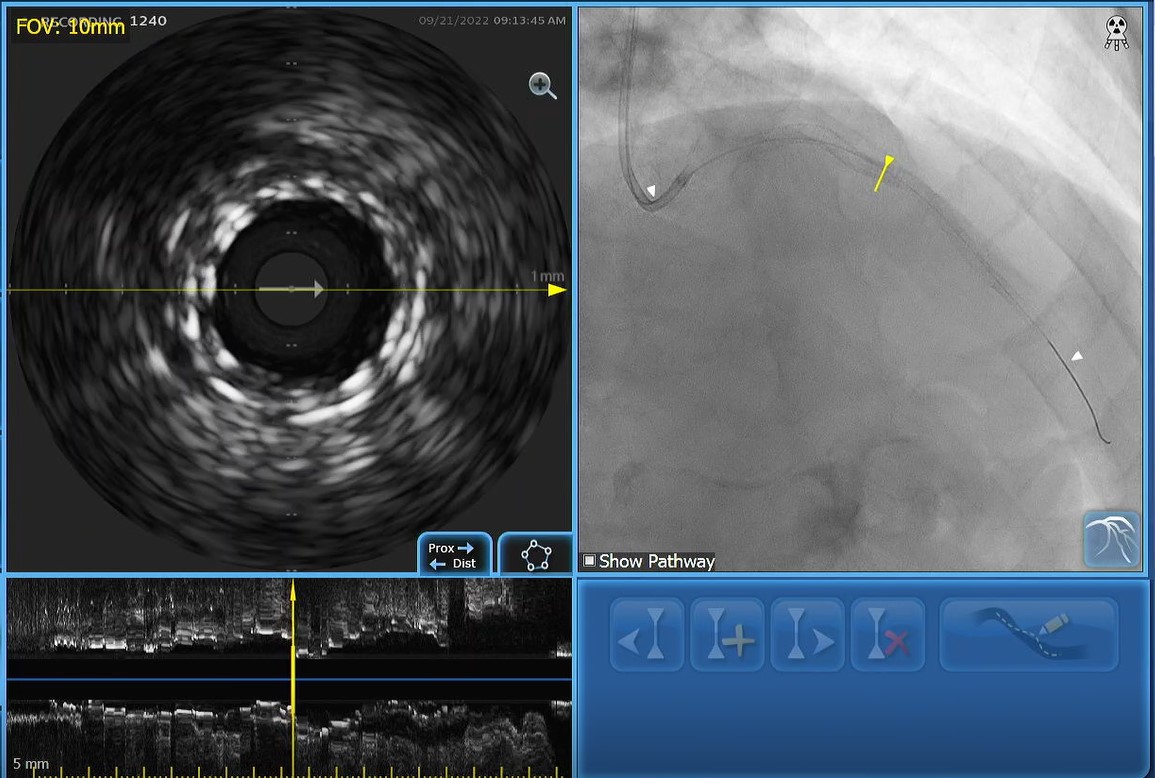
We only use 11 ml of contrast in angiography procedure. Then we proceed to PCI LAD. Firstly we did IFR to LAD which result was 0.77. IVUS showed mostly atheroma in beyond distal stent edge, stent under expanded, distal reference 3.0 mm, proximal reference 4.5 mm. After that, distal LAD was predilated with 2.5 mm NC balloon, 3.0 mm NC balloon was used in proximal-mid stent, 3.0 mm scoring balloon and 3.5 mm NC balloon were used in proximal edge stent. Then we treated distal LAD with 2.5X20mm DEB. IVUS evaluation showed no dissection beyond distal edge stent, proximal-mid stent well expanded, distal stent under expanded but IFR revealed significant step up in overlap site of proximal-mid stent. Hence, this site was decided to deploy 3.50/15mm DES at 18 atm. Another IVUS evaluation showed distal stent was under expanded, so further pre-dilatation was done with 3.0 mm NC balloon in distal stent; 3.5 mm NC balloon in mid stent. IFR evaluation revealed gradual step-up until proximal LAD. After IVUS and IFR evaluation showed acceptable result, we finished the procedure by deploying 3.0X30 mm DEB in distal stent and 3.5X20 mm DEB in proximal old stent. We only use 4 ml additional of contrast for final picture. So total 15 ml of contrast was delivered for this procedure.
Case Summary
Contrast-induced nephropathy has to be prevented due to adverse outcome complication. One of procedure to prevent contrast-induced nephropathy is low contrast PCI. Another way is to give renal protocol before or during the procedure but concern will be higher if the patient in heart failure condition to prevent acute pulmonary edema during PCI. IVUS-IFR guided PCI can guide operator to achieve a good outcome in low contrast PCI.


