Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-044
Guts and Glory
By Kogulakrishnan Kaniappan, Datuk Kumara Gurupparan
Presenter
Kogulakrishnan Kaniappan
Authors
Kogulakrishnan Kaniappan1, Datuk Kumara Gurupparan1
Affiliation
National Heart Institute, Malaysia1,
View Study Report
TCTAP C-044
CORONARY - Adjunctive Procedures (Thrombectomy, Atherectomy, Special Balloons)
Guts and Glory
Kogulakrishnan Kaniappan1, Datuk Kumara Gurupparan1
National Heart Institute, Malaysia1,
Clinical Information
Patient initials or Identifier Number
TA
Relevant Clinical History and Physical Exam
73 years old lady with history of Atrial Fibrillation, Chronic Kidney Disease Stage, Hypertension, Diabetes Mellitus, HFrEF ~38%, history of pangastritis, presented with chest pain for 2 weeks. She was previously ADL independent.
Clinically, shewas alert, mildly tachypneic with warm peripheries.
Clinically, shewas alert, mildly tachypneic with warm peripheries.
Relevant Test Results Prior to Catheterization
2DTransthoracic Echocardiography :
CXR
ECG:
BloodInvestigations :
Diagnosis :

CXR
ECG:
BloodInvestigations :
Diagnosis :

Relevant Catheterization Findings
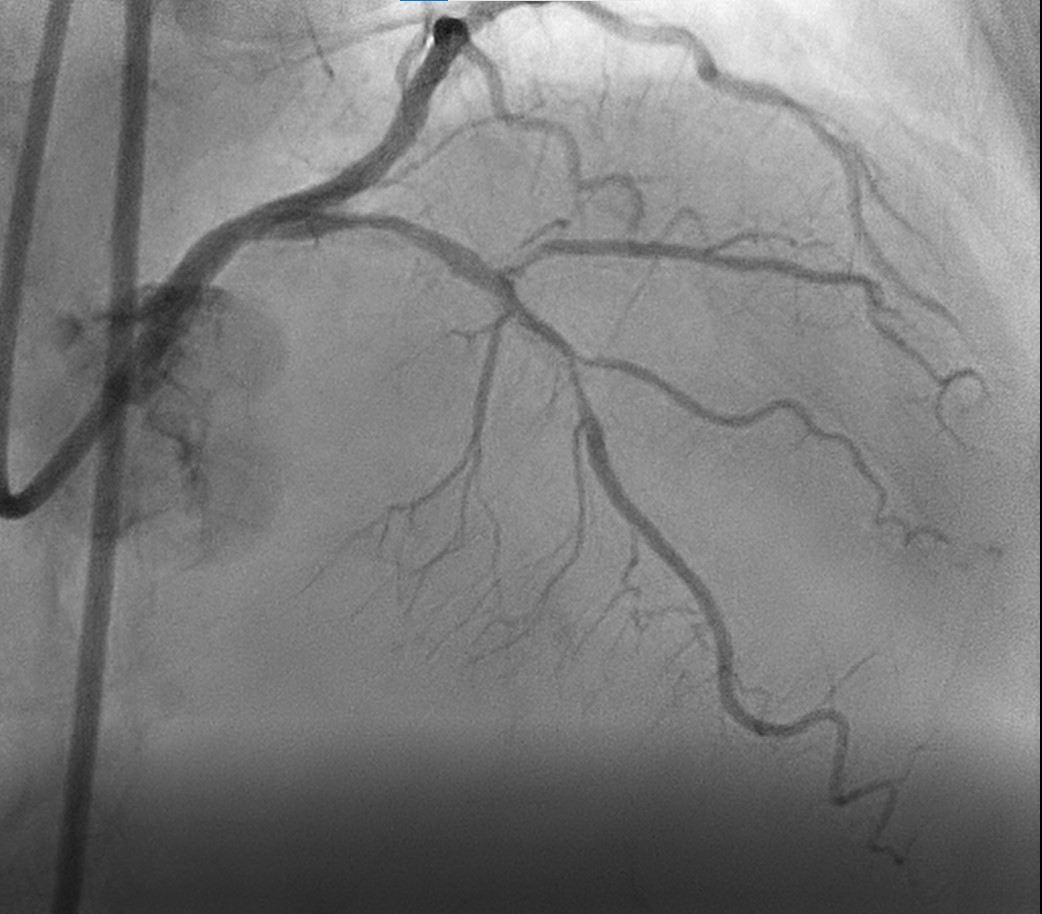
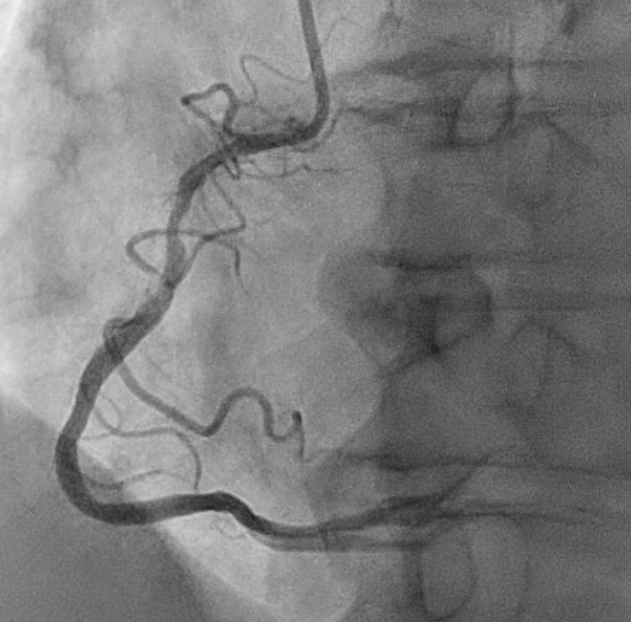
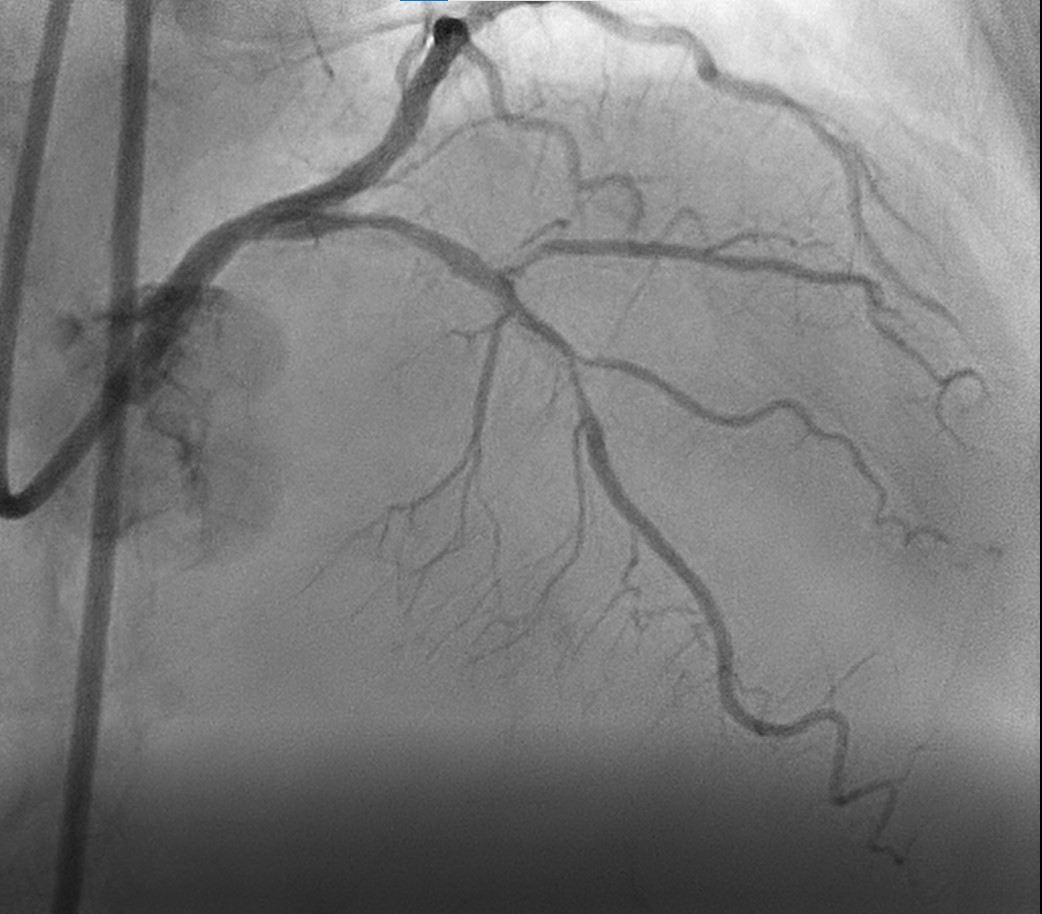
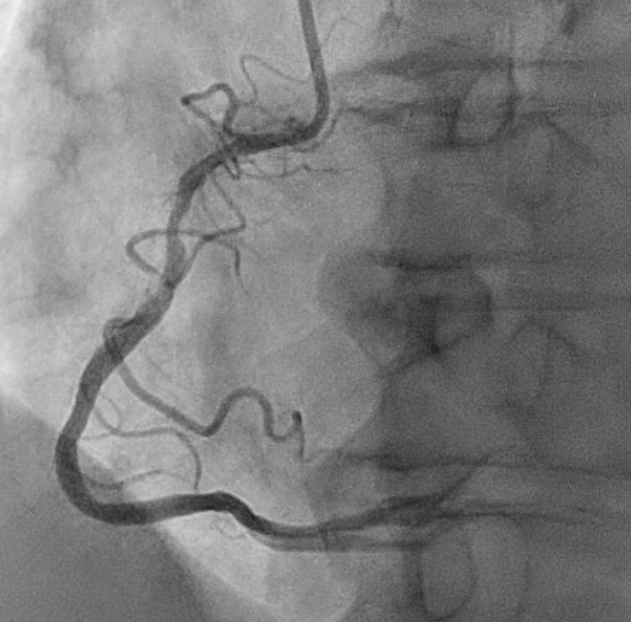
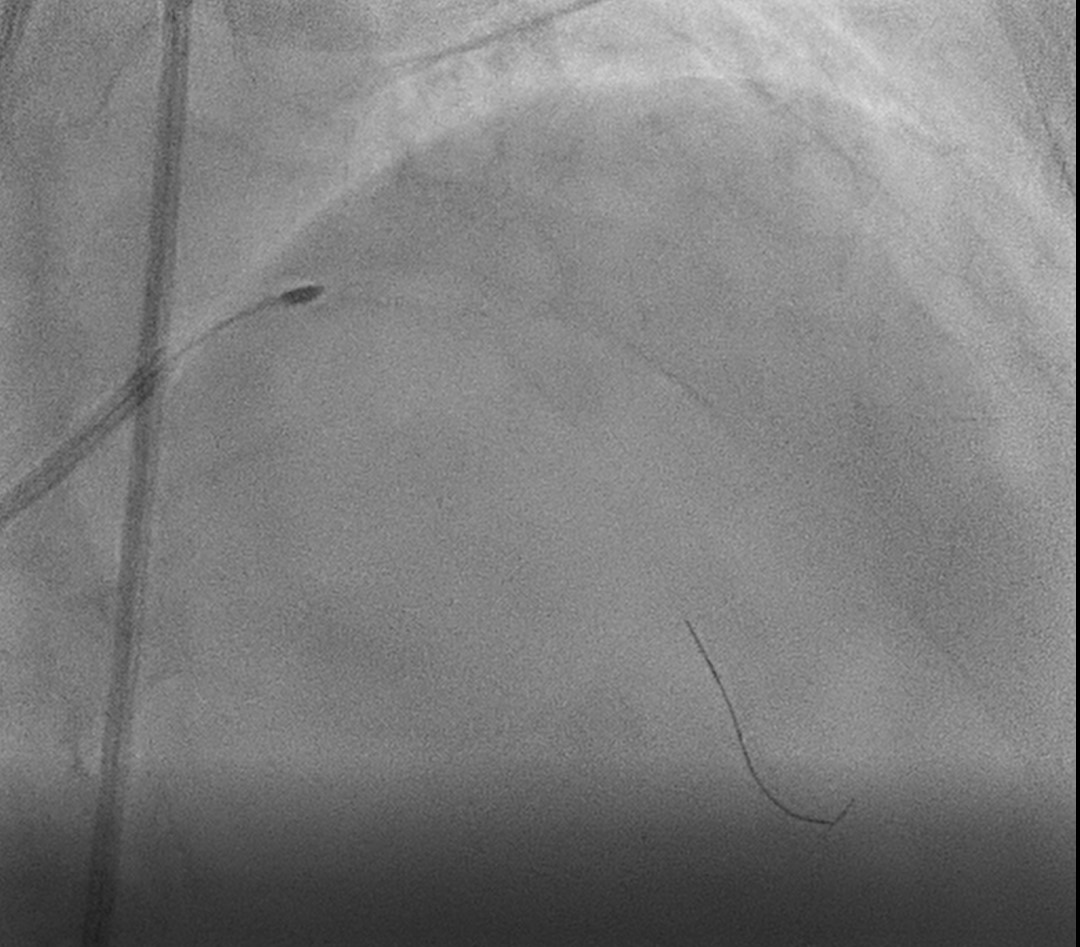
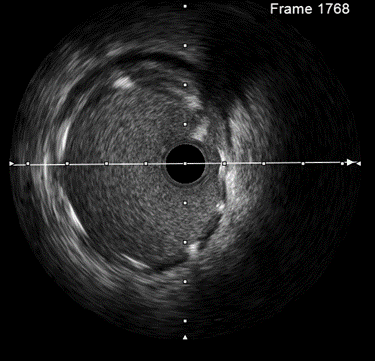
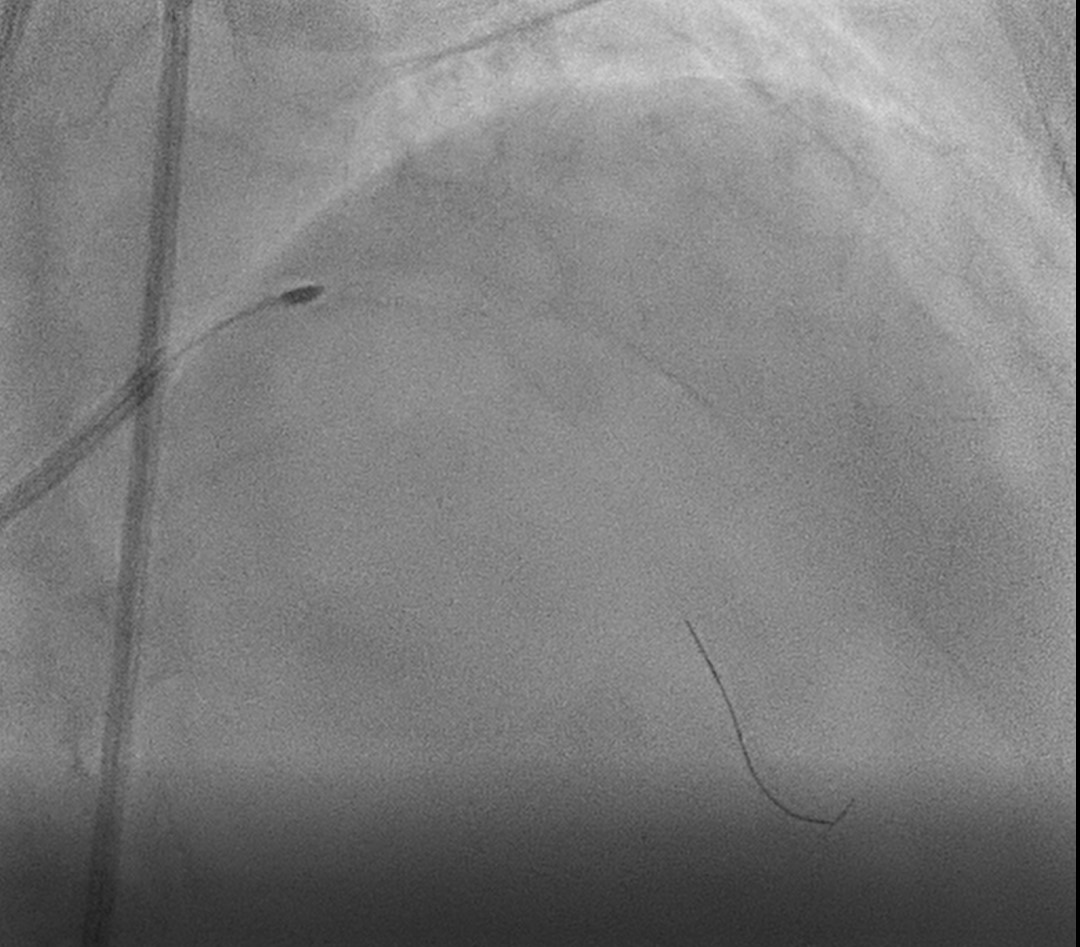
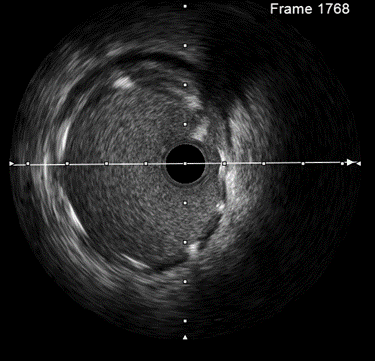
Coronary Angiogram done via right radialapproach , 6F sheath, 5F Optitorque catheter used
Patientdeclined CABG. In view of NSTEMI and persistent chest pain in ward, offeredhigh risk PCI to LAD with atherectomy and staged PCI to RCA later. Patient and family agreed.

Patientdeclined CABG. In view of NSTEMI and persistent chest pain in ward, offeredhigh risk PCI to LAD with atherectomy and staged PCI to RCA later. Patient and family agreed.

Interventional Management
Procedural Step
PCI to LM / LAD / Diagonal withAtherectomy


Case Summary
Learning points


