Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-173
Coronary Angiography Using Gadolinium-Based Contrast Agents and Intravascular Ultrasound Guided Percutaneous Coronary Intervention
By Khalil Lebcira, Mohamed Saad-Eddine Bouzghaia, Chakib Lamraoui
Presenter
Khalil Lebcira
Authors
Khalil Lebcira1, Mohamed Saad-Eddine Bouzghaia2, Chakib Lamraoui1
Affiliation
Universitary Hospital of Bejaia, Algeria1, El Besma Private Hospital, Algeria2,
View Study Report
TCTAP C-173
OTHERS - Renal Insufficiency and Contrast Nephropathy
Coronary Angiography Using Gadolinium-Based Contrast Agents and Intravascular Ultrasound Guided Percutaneous Coronary Intervention
Khalil Lebcira1, Mohamed Saad-Eddine Bouzghaia2, Chakib Lamraoui1
Universitary Hospital of Bejaia, Algeria1, El Besma Private Hospital, Algeria2,
Clinical Information
Patient initials or Identifier Number
B.J.
Relevant Clinical History and Physical Exam
A 69 year-old female presented to the emergency department for several episodes of anginal chest pain occurring at rest for the last week.Her previous medical history was remarkable for hypertension, type 2 diabetes mellitus, atrial fibrillation, anaemia and stage 4 chronic kidney disease Previous medications include bisoprolol, ramipril, acenocoumarol and furosemide.The patient was haemodynamically stable, her blood pressure was 120/60 mmHg and her heart rate was 100 beats per minute (bpm).
Relevant Test Results Prior to Catheterization
ECG at presentation showed atrial fibrillation and a complete left bundle branch block.Echocardiography revealed anterior and septal hypokinesia, left ventricular ejection fraction (LVEF) was estimated to 30%.Emergency laboratory testings were remarkable for: estimated glomerular filtration rate (eGFR) = 18 mL/min, haemoglobin = 9 g/dL
and troponin I= 500 × upper reference limit (URL)
and troponin I= 500 × upper reference limit (URL)
Relevant Catheterization Findings
To avoid further deterioration of her renal function by contrast-induced nephropathy, we performed a coronary angiography using non-diluted Gadobutrol, a group 2 gadolinium-based contrast agent, as the only contrast agent.
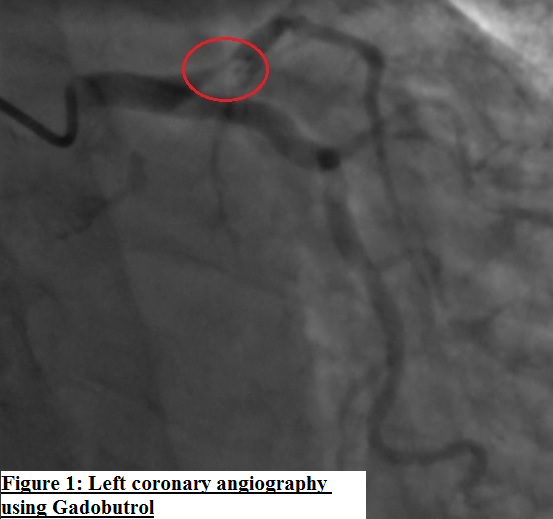
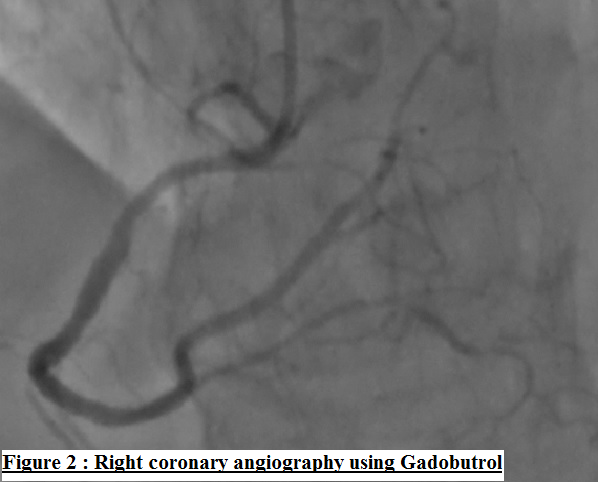
It revealed a 90% proximal to mid left anterior descending artery(LAD) stenosis (figure 1), which was the presumed culprit lesion, a severe stenosis of a diffusely diseased posterior descending artery (PDA) and a 40% stenosis of proximal to mid right coronary artery (figure 2).
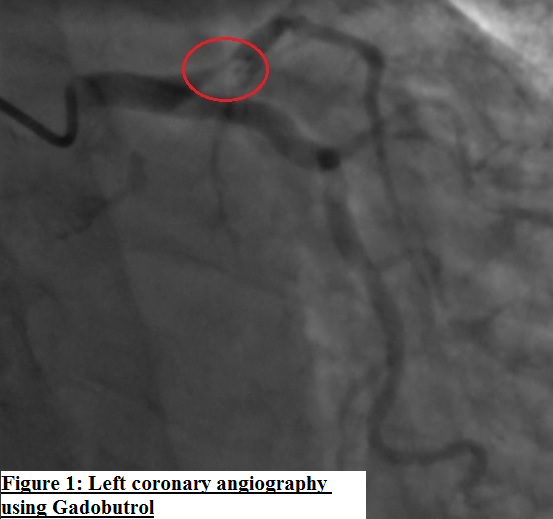
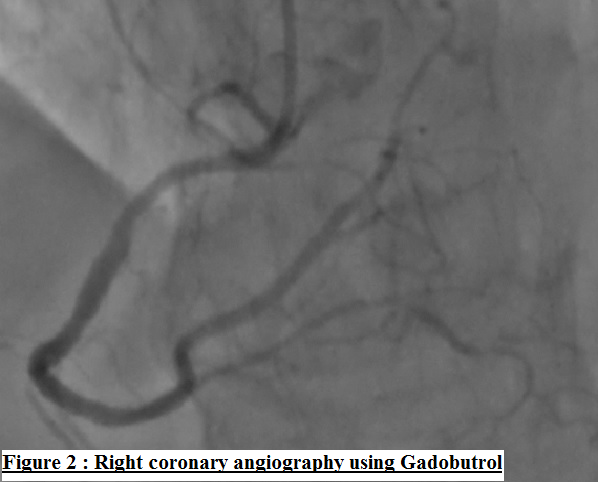
It revealed a 90% proximal to mid left anterior descending artery(LAD) stenosis (figure 1), which was the presumed culprit lesion, a severe stenosis of a diffusely diseased posterior descending artery (PDA) and a 40% stenosis of proximal to mid right coronary artery (figure 2).
Interventional Management
Procedural Step
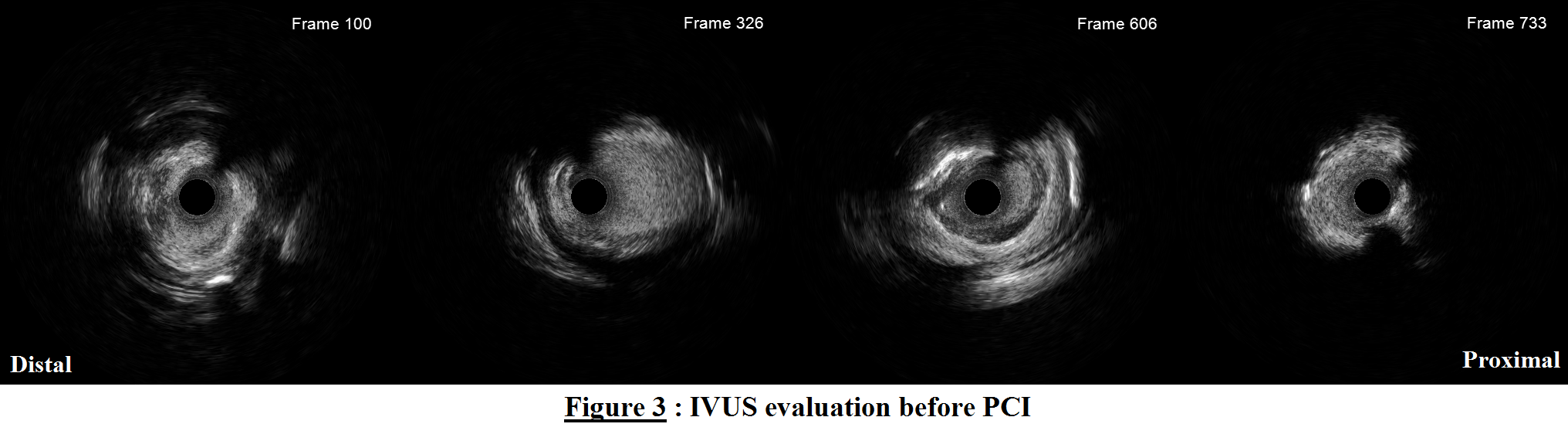
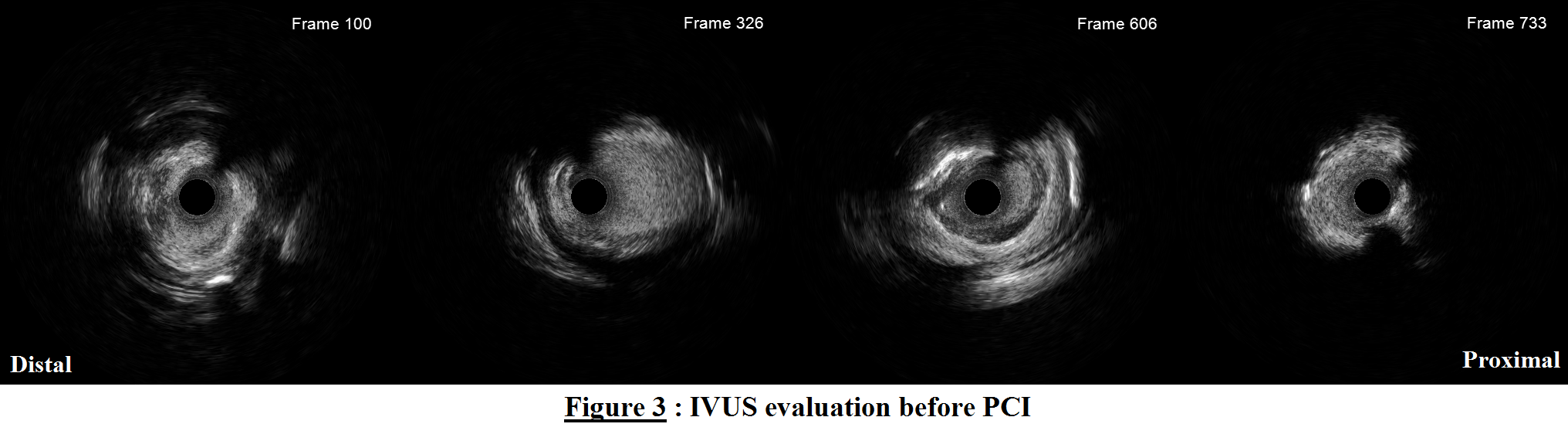
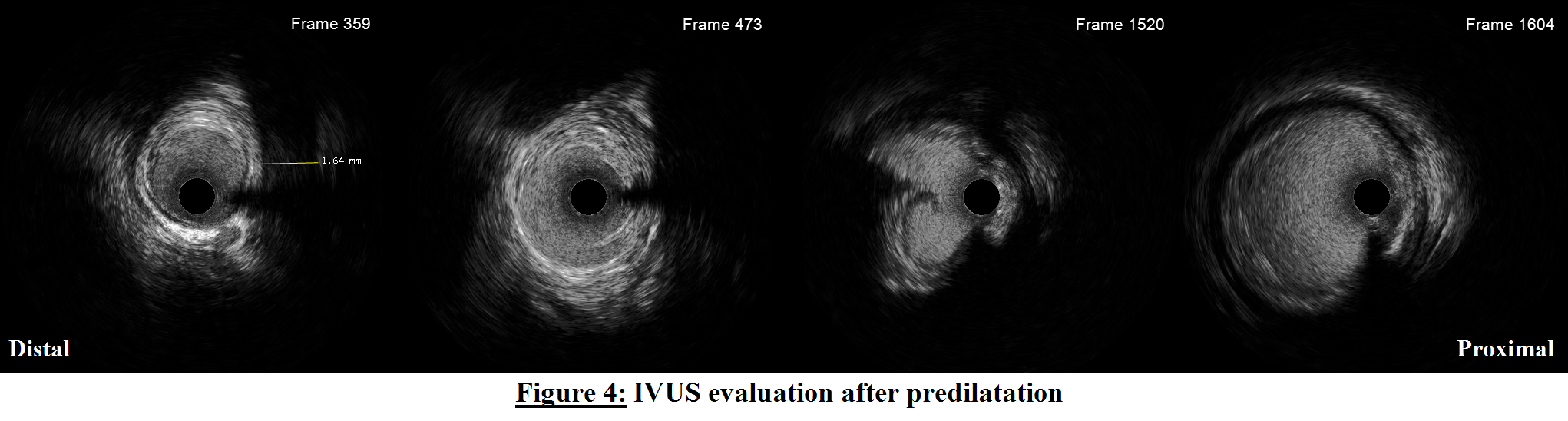
LAD intravascular ultrasound (IVUS) evaluation revealed a tandem lesion with plaque rupture and thrombus in the more distal lesion (figure 3, frame 100) and a thrombus containing mixed plaque (fibroatheroma, non circumferential calcifications, deep and superficial attenuated plaque) in the more proximal lesion (figure 3, frames 606 and 733). Minimal luminal area was 1.6mm².Lesion predilatation with 4.0/15mm cutting balloon was performedSubsequent IVUS evaluation identified a 2 mm long and less than 60° angle intimal dissection (figure 4, frame 473) in a deep myocardial bridge (MB) segment (figure 4, frame 359), a large dissection (figure 4, frame 1520) with hematoma at the proximal lesion site.
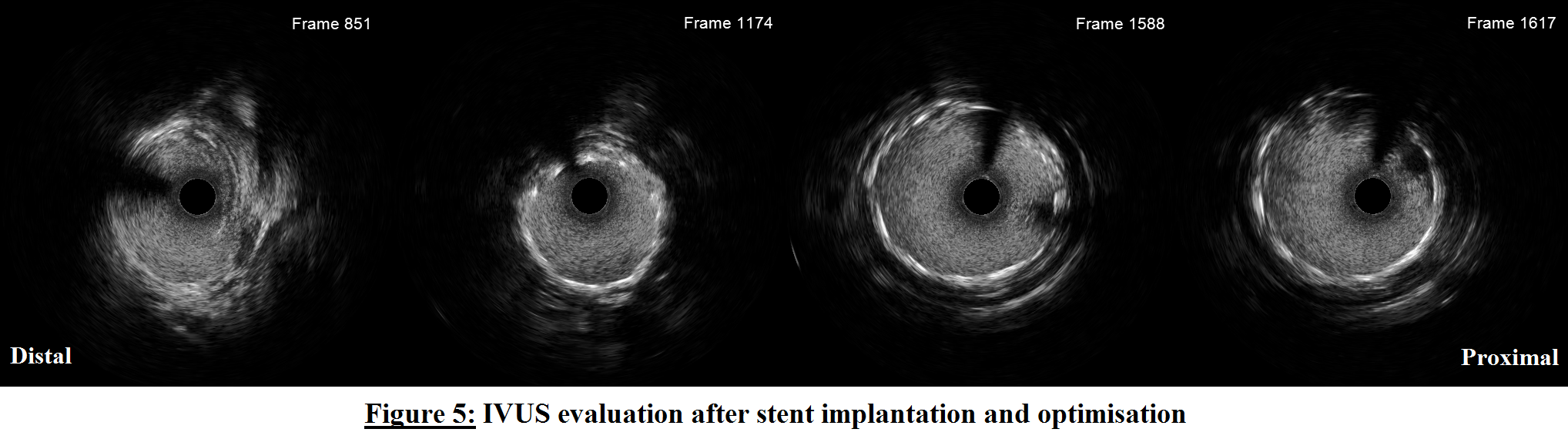
Luminal diameters at distal and proximal landing zones were respectively (4.0 and 5.5 mm). Since distal dissection exhibited none of the unfavorable evolution criteria, we decided to not cover it to avoid landing a stent in a deep MB . Lesion Length was 35 mm based on IVUS pullback measurement.A 4.0/38 mm drug-eluting stent was positioned with gadobutrol injection guidance and proximally post-dilated with a 5.5/12 mm non compliant balloon.Post-PCI IVUS showed good stent apposition ( figure 5, frames 1174 and 1588), no edge dissection, no worsening of the non-covered distal dissection (figure 5, frame 851) and some tissue protrusion ( figure 5, frame 1617). Minimal stent area was 8.9 mm².Final angiography with gadobutrol confirmed TIMI 3 flow and no distal perforation.
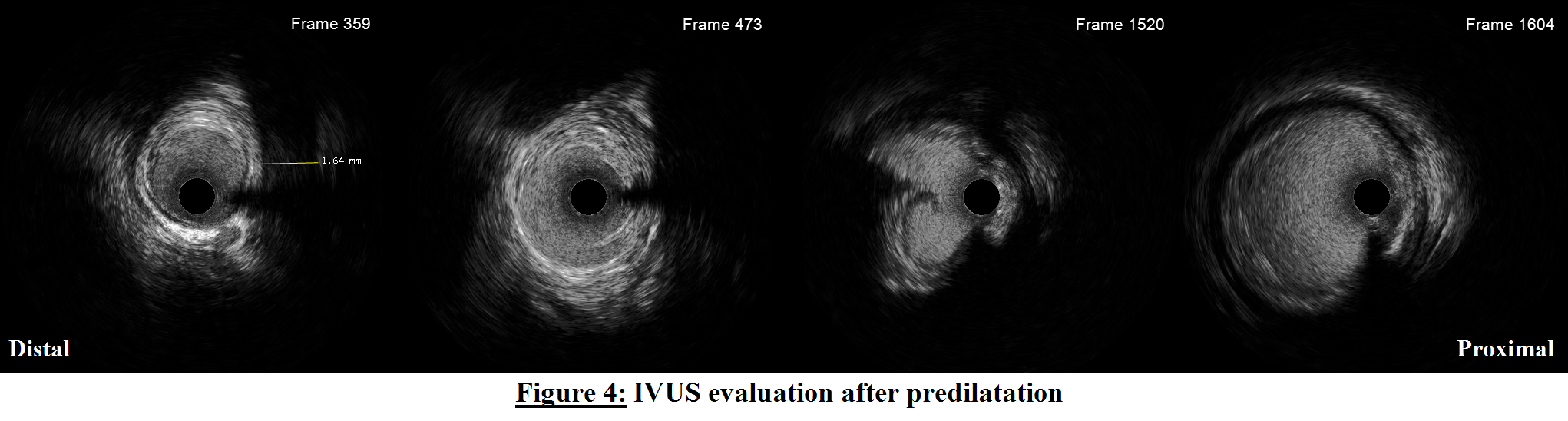
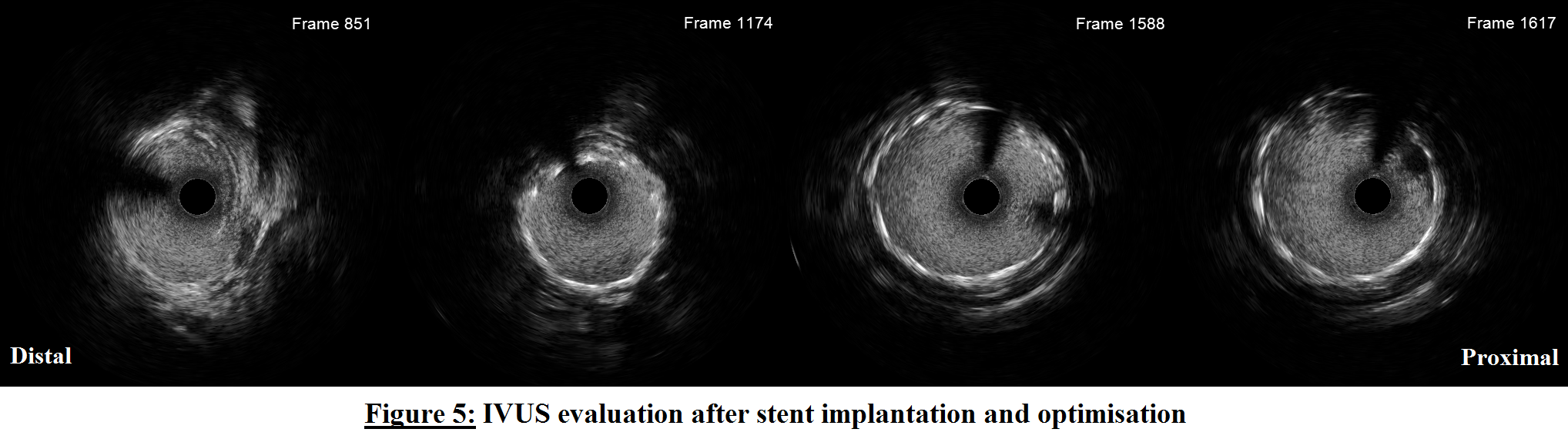
Luminal diameters at distal and proximal landing zones were respectively (4.0 and 5.5 mm). Since distal dissection exhibited none of the unfavorable evolution criteria, we decided to not cover it to avoid landing a stent in a deep MB . Lesion Length was 35 mm based on IVUS pullback measurement.A 4.0/38 mm drug-eluting stent was positioned with gadobutrol injection guidance and proximally post-dilated with a 5.5/12 mm non compliant balloon.Post-PCI IVUS showed good stent apposition ( figure 5, frames 1174 and 1588), no edge dissection, no worsening of the non-covered distal dissection (figure 5, frame 851) and some tissue protrusion ( figure 5, frame 1617). Minimal stent area was 8.9 mm².Final angiography with gadobutrol confirmed TIMI 3 flow and no distal perforation.
Case Summary
Coronary angiography using group 2 gadolinium-based contrast agents provides acceptable quality angiograms sufficient to identify significative lesions and to guide critical steps of PCI. Serial IVUS evaluations (before angioplasty, after lesion preparation and after stent implantation) allow adequate tools selection for lesion preparation, landing zones determination, stent sizing and perprocedural strategy ajustements to optimise results without the need of repeated contrast injections. The combination of the two techniques allows a safer zero iodinated contrast angiography and PCI in patients at high risk of contrast induced nephropathy or iodinated contrast allergy.


