Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-159
Type IV In-Stent Restenosis Strategy by Optical Coherence Tomography Guided.
By Cheng-Cheng Kan, Wei-Che Tsai
Presenter
Cheng-Cheng Kan
Authors
Cheng-Cheng Kan1, Wei-Che Tsai2
Affiliation
Tri-Service General Hospital (TSGH), Taiwan1, Tri-Service General Hospital, Taiwan2,
View Study Report
TCTAP C-159
IMAGING AND PHYSIOLOGIC LESION ASSESSMENT - Imaging: Intravascular
Type IV In-Stent Restenosis Strategy by Optical Coherence Tomography Guided.
Cheng-Cheng Kan1, Wei-Che Tsai2
Tri-Service General Hospital (TSGH), Taiwan1, Tri-Service General Hospital, Taiwan2,
Clinical Information
Patient initials or Identifier Number
2377305
Relevant Clinical History and Physical Exam
54-year-old male had history of ST-segment elevation myocardial infarction, status post percutaneous coronary intervention with bare metal stents in Nov. 2021, and dual antiplatelet therapy (DAPT: aspirin & clopidogrel); diabetes mellitus, and hyperlipidemia.
He presented with bilateral lower limbs swelling, and dyspnea on exertion in recent weeks.
Relevant Test Results Prior to Catheterization
ECG showed normal sinus rhythm, right axis deviation.Echocardiography revealed generalized hypokinesia of LV with LVEF: 31%.LDL-Cholesterol: 212mg/dL, HbA1c: 6.6%.
Relevant Catheterization Findings
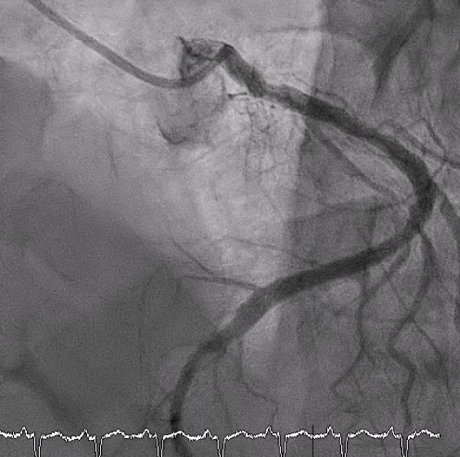
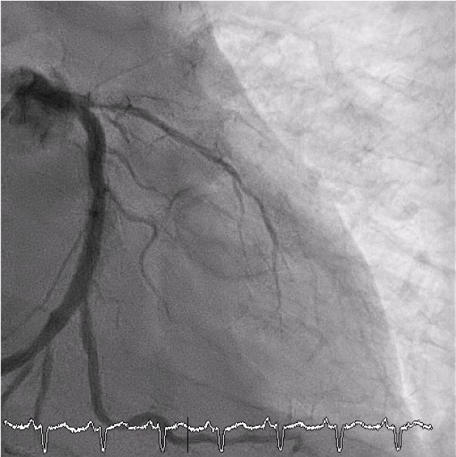
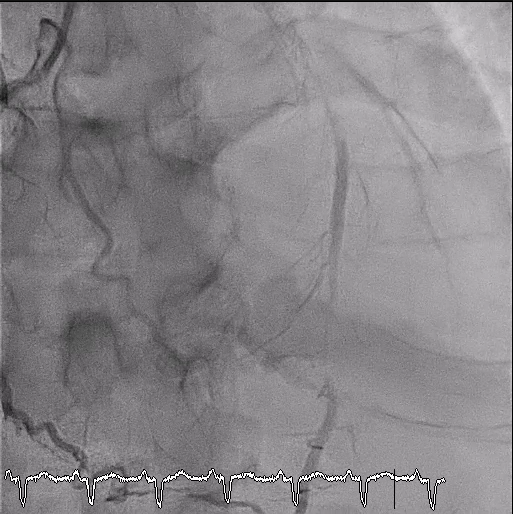
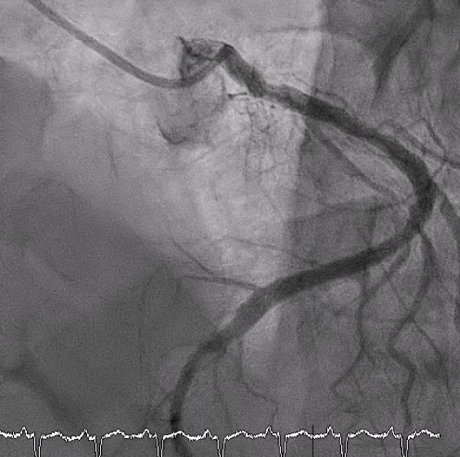
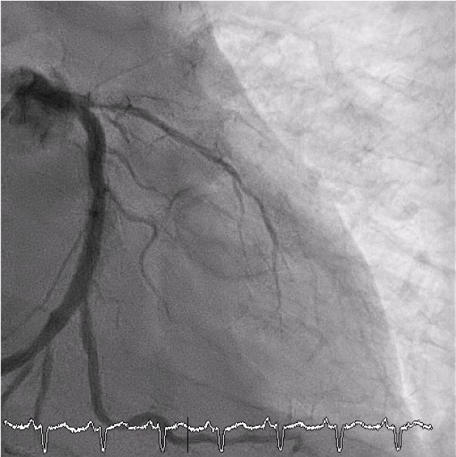
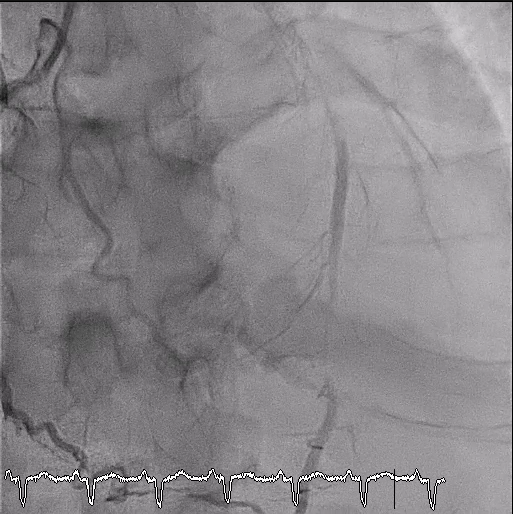
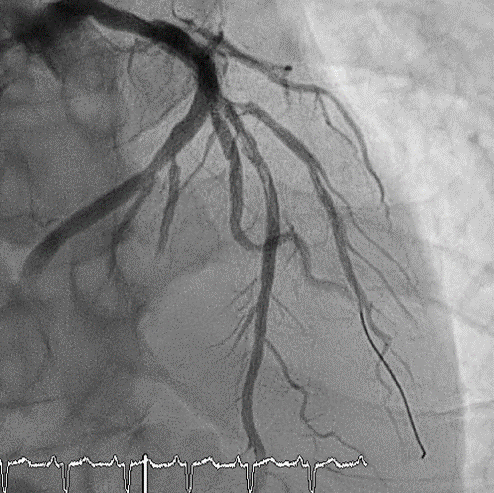
LMCA: PatentLAD: Luminal irregularity(LI)-P/3~M/3: Status post stenting with type IV in-stent restenosis (ISR), receiving retrograde collateral flow from conus branch of RCA via septal branchLCX: Dominant vessel with LI-P/3~M/3: Status post stenting with 40% type II ISR-D/3: Segmental 60% eccentric stenosis -OM2: Discrete 60% eccentric stenosis at ostiumRCA: Non-dominant with LI-Conus branch: Giving retrograde collateral flow to P/3~M/3 LAD-D/3: Giving retrograde collateral flow to M/3~D/3 of LAD
Interventional Management
Procedural Step
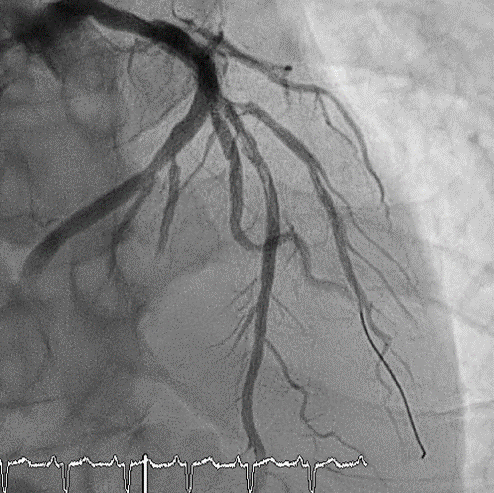
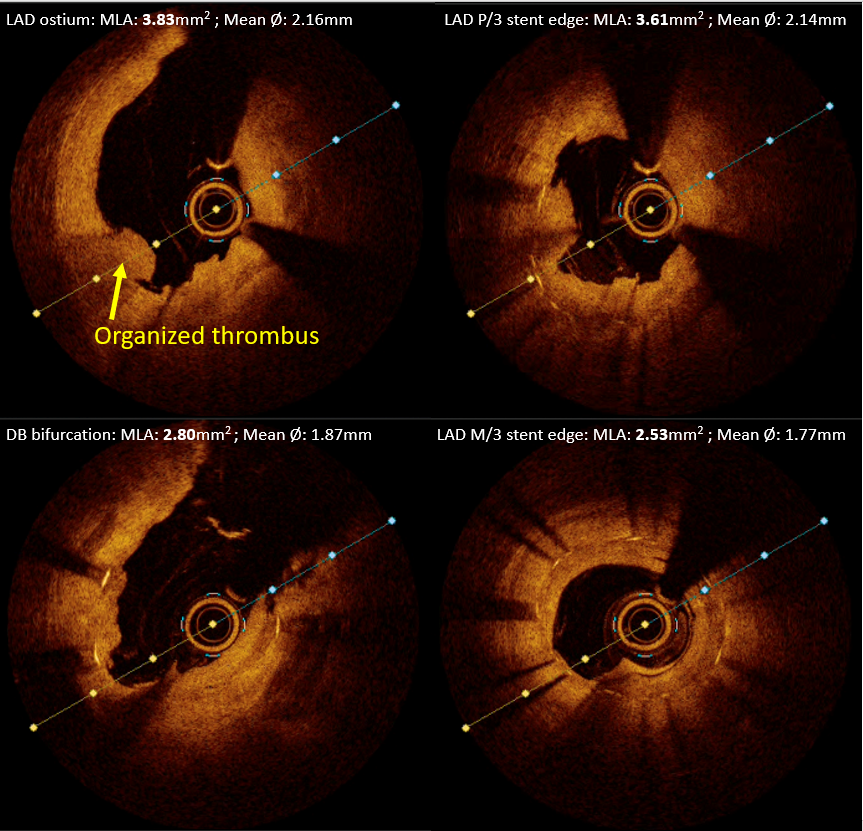
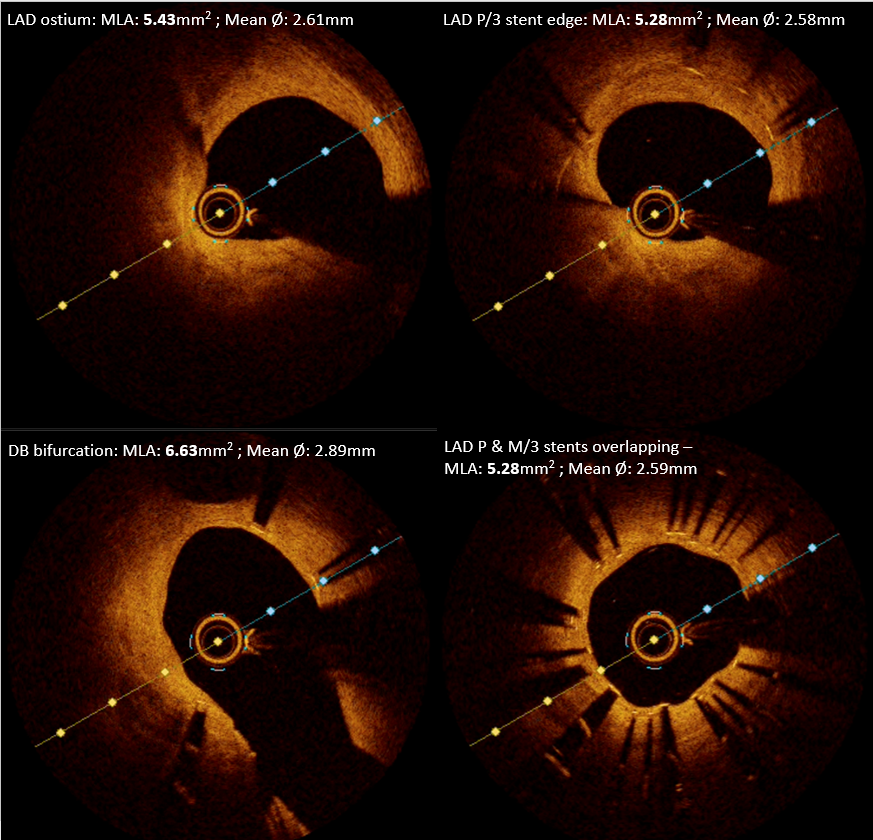
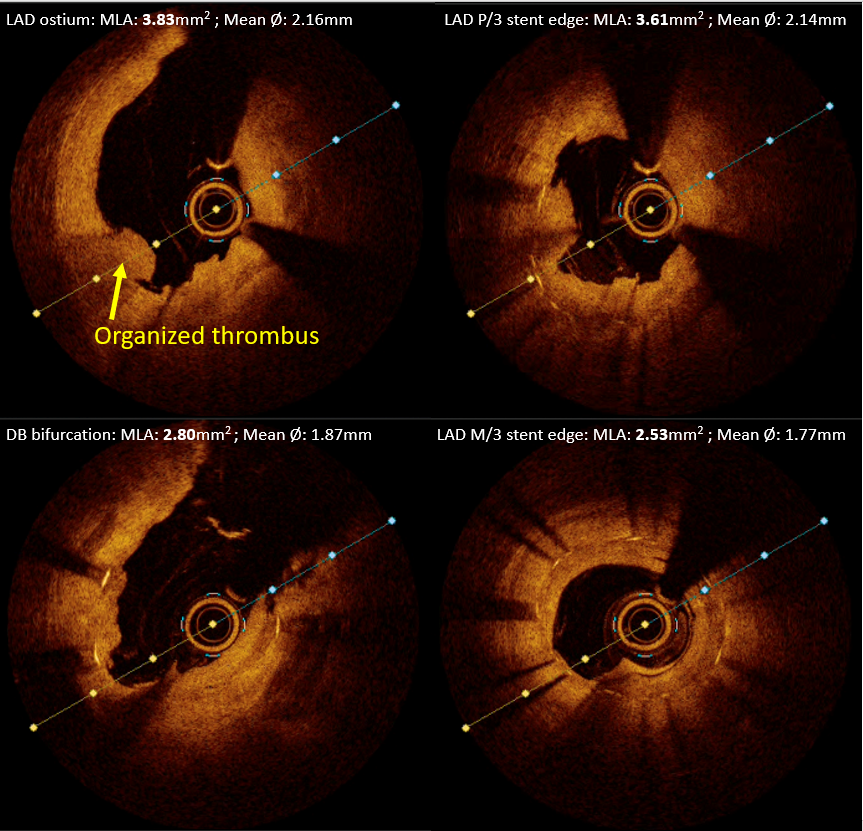
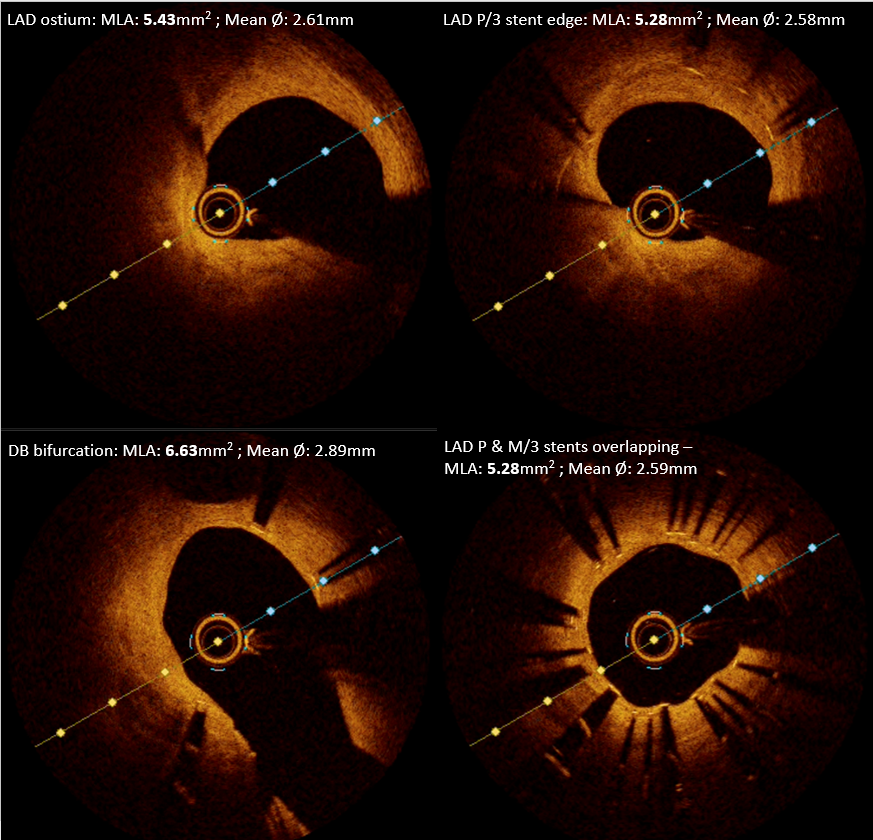
1.Under EBU 3.5 guiding catheter, Fielder FC wire, loaded in microcatheter, was wiring to the proximal cap of ISR at P/3 LAD.2.Changed wire to Gaia 2nd to across the CTO site successfully, then, microcatheter was push to M/3 LAD.3.Changed to SION wire, and was wiring to D/3 LAD.4.The microcatheter was removed by trapping balloon technique.5.After sequential balloon dilation, type B dissection at M/3 LAD was noted(fig.A).6.Intravascular OCT(fig.B) demonstrated 1) plaque erosion with organized thrombus at proximal edge of LAD stent; 2)diffuse neointimal hyperplasia over middle portion of LAD stent; 3) under expansion at distal stent edge. 7.Balloon dilation and stent implantation at M/3 LAD with proximal edge overlapping the distal part of previous LAD stent. 8.The drug-coated balloon was inflated at P/3 LAD stent, covered organized thrombus at proximal edge of P/3 stent.9.Intravascular OCT demonstrated less thrombus burden at proximal edge of P/3 LAD stent with minimal stent area: 4.71mm2. 10.The final angiography showed <10% residual stenosis over the P/3~M/3 LAD stents.After 4 months DAPT with aspirin & ticagrelor, follow-up CAG:1.Intravascular OCT(fig.C):1)Good result without stenting over proximal edge of P/3 LAD stent with resolved thrombus.2)P/3 LAD stent showed fully endothelialization with MSA: 3.91mm23)M/3 LAD stent showed fully endothelialization with MSA: 3.96mm22.Finally, there was no need for further intervention, and kept dual antiplatelet therapy.
Case Summary
1. The intravascular optical coherence tomography is a practical tool to assess ISR about lesion length, severity and mechanism, which helpful to guide the treatment . 2. Prevention of ISR by proper bed preparation, adequate lesion coverage, and use of intravascular imaging to guide stent placement is preferable.3. According to EROSION III trial, plaque erosion treated with drug-coated balloon, without stenting, could be a optimal choice.4. We checked patient's CYP2C19 genotype showed *1/*2 alleles, which meant intermediate metabolizer of Clopidogrel, and shifted Clopidogrel to Ticagrelor after first time PCI, also provided better outcome for the patient.


