Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-194
Successful Endovascular Treatment for a Systemic to Pulmonary Artery Fistula Presenting With Pulmonary Hypertension
By Anish Hirachan, Prabesh Neupane
Presenter
Anish Hirachan
Authors
Anish Hirachan1, Prabesh Neupane2
Affiliation
Nepal Mediciti Hospital, Nepal1, Shahid Dharmabhakta National Transplant Centre, Nepal2,
View Study Report
TCTAP C-194
STRUCTURAL HEART DISEASE - Pulmonary Intervention: CTEPH, PHTN
Successful Endovascular Treatment for a Systemic to Pulmonary Artery Fistula Presenting With Pulmonary Hypertension
Anish Hirachan1, Prabesh Neupane2
Nepal Mediciti Hospital, Nepal1, Shahid Dharmabhakta National Transplant Centre, Nepal2,
Clinical Information
Patient initials or Identifier Number
Mrs JB
Relevant Clinical History and Physical Exam
A 32-year-old postpartum female presented with dyspnea and limb swelling for 5 days. She had an eventful postpartum state with massive postpartum hemorrhage requiring multiple blood transfusions. Clinical examination showed BP 100/60 mmHg, Pulse 108 /min, bipedal edema, and Spo2 95 % onroom air. She had equal air entry on both lung fields with normal heart sounds and no murmurs audible. She had no significant medical history of any chronic illness in the past.




Relevant Test Results Prior to Catheterization
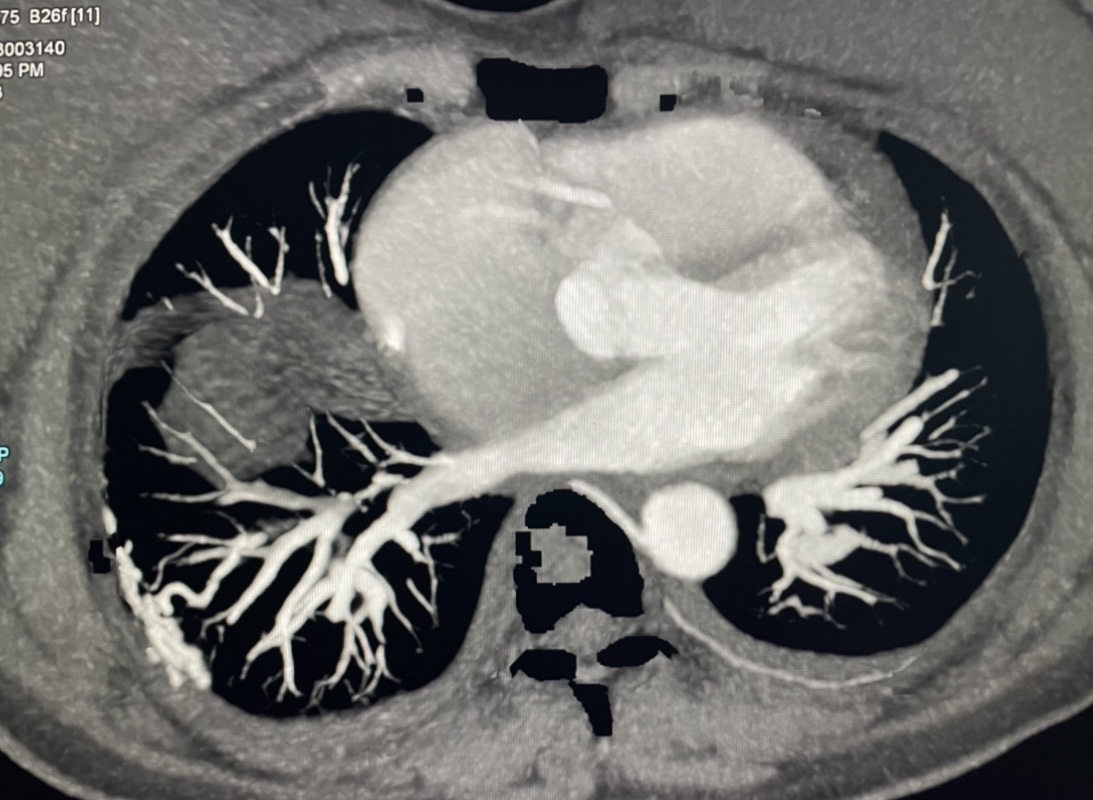
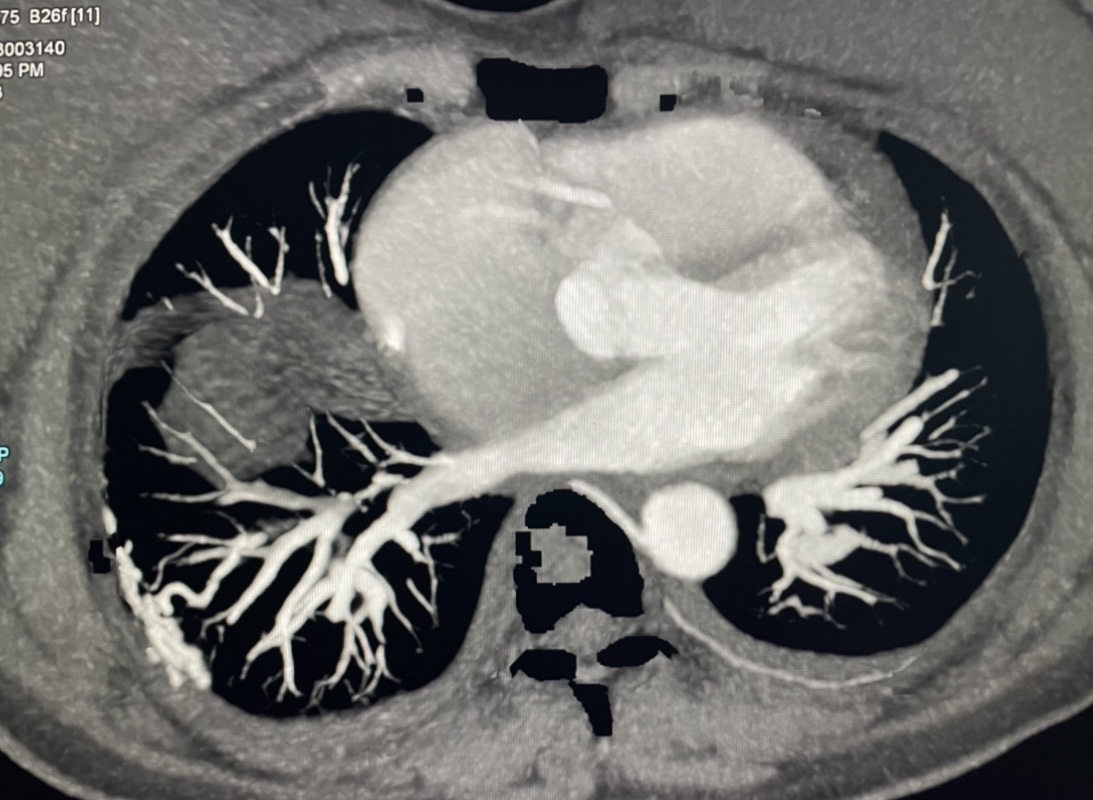
Her lab parameters showed - Hb-10g/dl, ESR -64mm/hr, ANA - >500IU/ml, AntiU1 RNP antibody -positive, viral serologies including HIV negative.She had her NT proBNP level of 998pg/ml with a negative venous doppler of the lower limb . Her echocardiogram revealed dilated RA and RV with moderate TR with moderate pulmonary hypertension (63 mmHg). Contrast-enhanced CT showed evidence of intercostal-pulmonary arterial fistula ( 6th and 7th intercostal branch) with dilated right atrium and ventricle.
Relevant Catheterization Findings
She underwent invasive angiography from the right femoral artery which demonstrated tortuous and tangling vessels draining into branches of the right inferior pulmonary artery through the right 6th and 7th intercostal branches of the descending aorta . Her right heart catheterization study revealed tracings as - RA pressure ( 25/10 (15 mmHg ), PCWP - 16/6( 9 mmHg), RV / ( pulmonary artery ) PA- Pre-procedure - 52/31(38mmHg) and PA - Post procedure 50/15 ( 27mmHg ), Aorta - 130/90( 72 mmHg).
Interventional Management
Procedural Step
Procedure - After the angiogram of the right 6th and 7th intercostal arteries and its abnormal fistulous communication to the inferior pulmonary artery branches, the super selective cannulation into the 6th and 7th intercostal branches distally was done with a microcatheter, and successful embolization was done with a combination of lipiodol and glue injected into the distal feeding branches. Post-embolization angiography demonstrated the absence of flow into the vascular nidus and branches of pulmonary arteries. A repeat right heart catheterization was done to check for an immediate drop in pulmonary pressure which revealed that mean PA pressure dropped from 38 mmHg to 27 mmHg.
Case Summary
Traditionally, resection of the fistula and the involved lung parenchyma is considered the definitive treatment of SA-PAFs. The embolization of the involved feeder, and arteries is an alternative treatment since major surgery and general anesthesia are unnecessary and the loss of lung parenchyma is minimal. In addition, in the case of SA-PAFs with multiple involved vessels, like in our case, embolization is more useful to control these multiple lesions. Our patient is in a one-year follow-up with the last repeat CT angiogram showing no evidence of fistula and an Echocardiogram showing normal cardiac chambers with normal pulmonary pressure and normal LV function.


