Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191114_019
| CORONARY - Complications | |
| Cardiogenic Shock Post Successful PCI to CTO | |
| Yen-Lien Chou1, Jun-Ting Liou1 | |
| Tri-Service General Hospital, Taiwan1, | |
|
[Clinical Information]
- Patient initials or identifier number:
2638941
-Relevant clinical history and physical exam:
68-year-old man, non-smoker
-Relevant test results prior to catheterization:
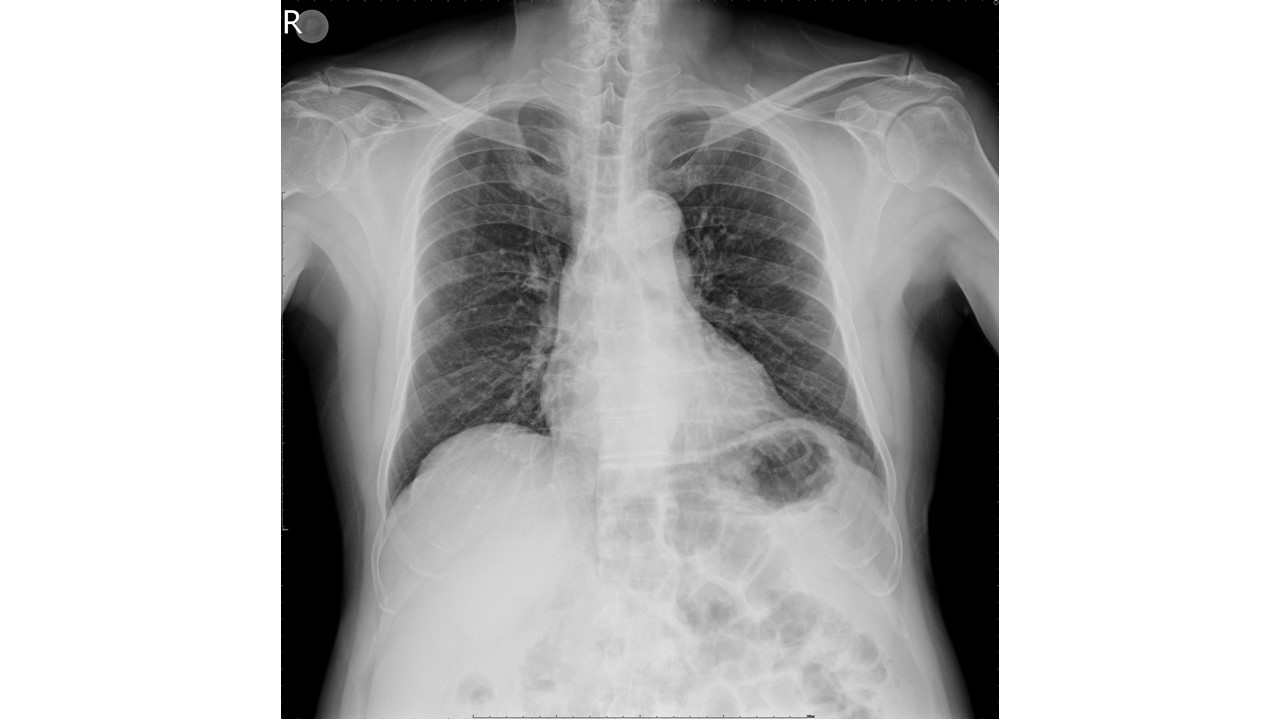
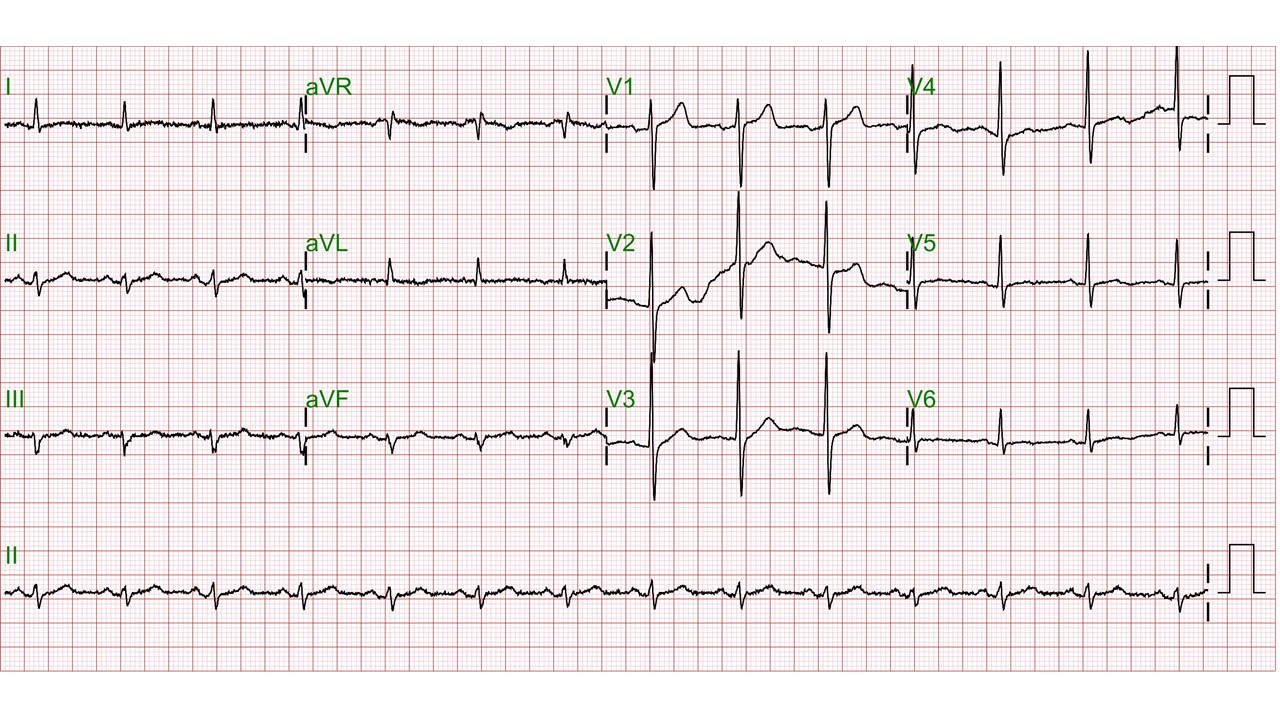
ECG: Sinus rhythm, NSSTTCCXR: Emphysema, normal heart borderCoronary CTA: 2-vessel disease with critical stenosis over LAD at p-m LAD > 90% stenosis, 30% narrowing at RCA, 40%narrowing at d-LCx, and 50% at RI
  - Relevant catheterization findings:
LMCA:
|
|
|
[Interventional Management]
- Procedural step:
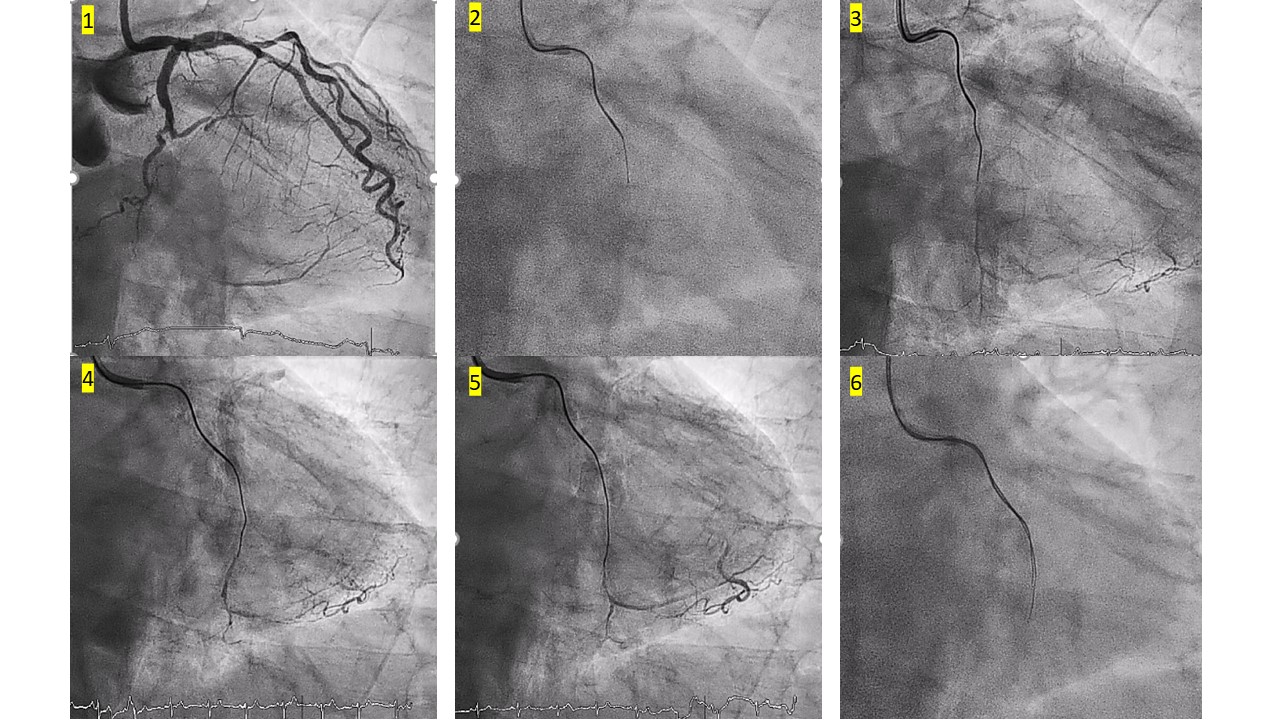
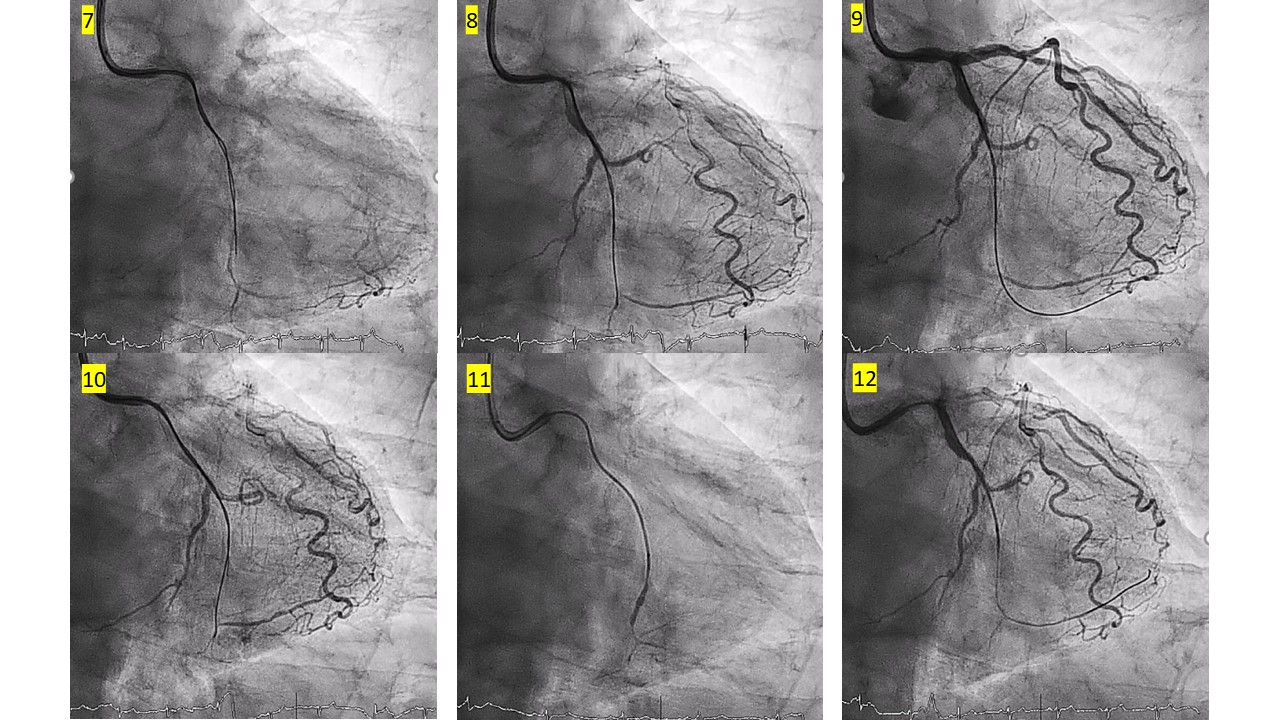
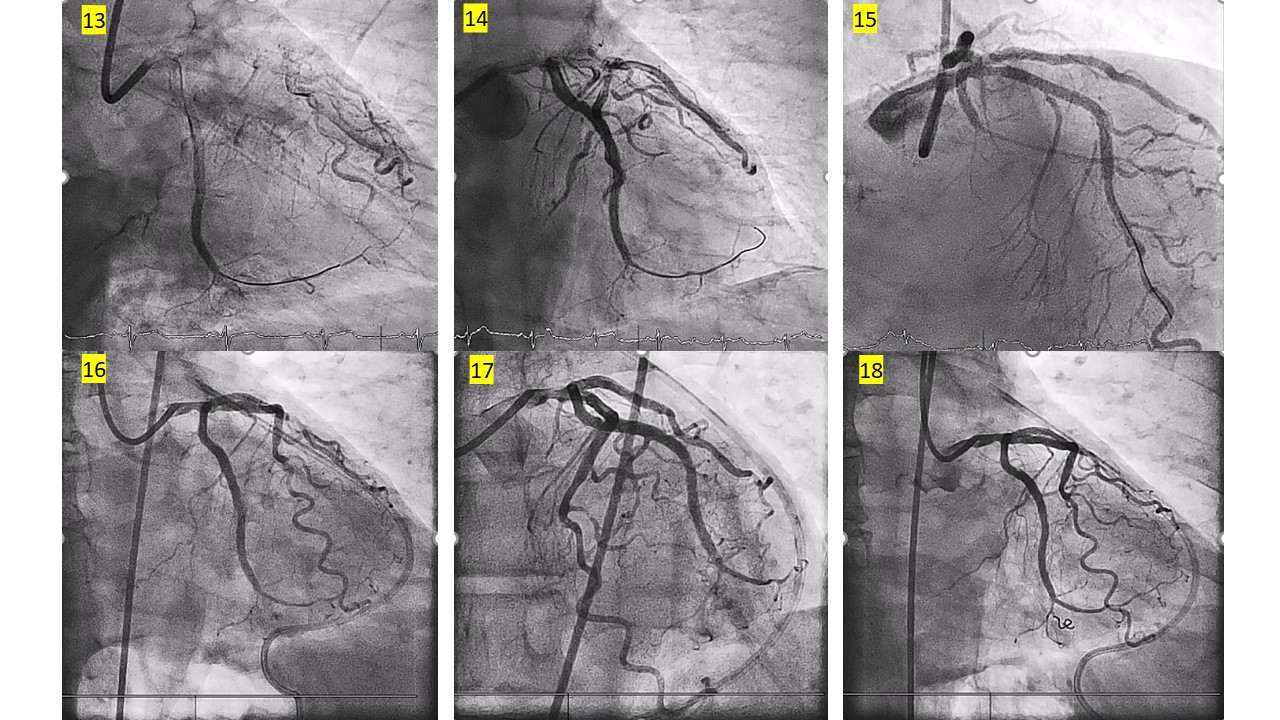
The 7 Fr EBU 3.5 guiding catheter was used. First attempt with XTR but failure because the hard proximal CTO cap. After changing to Gaia 1st wire, we penetrated the proximal CTO cap through the lesion to the middle part, but the Gaia 1st wire was in the subintimal space. We penetrated the distal CTO cap with parallel wire technique by Gaia 2ndwire. Following angiogram showed little contrast extravasation over the distal branch. The Gaia 2nd wire was in the false lumen. We pulled back Gaia 2nd wire a little then manipulated it to the distal true lumen. PCI with balloon and stenting was done over from the distal to proximal part of LCx. Contrast extravasation and staining with quick dissipation along small channel out of the distal branch of LCx after completing PCI to LCx. No symptoms or hemodynamic change. Echocardiography showed no pericardial effusion. Spontaneous healing was expected and following PCI with stenting over LAD and RI was proceeded. Patient had developed dizziness, cold sweating and paleness after getting up from bed at ward, about 40min after completing PCI. Cardiac tamponed and shock was confirmed and emergent pericardiocentesis was done (total 300 cc bloody pericardial effusion). Following angiography showed persistent coronary perforation at distal LCx branch with contrast staining. Good hemostasis was achieved after deploying two coils at the perforation channel at distal LCX branch. Following angiography showed no more contrast staining or extravasation.
   - Case Summary:
1. Coronary perforation is the one of the challenging issues and complication during CTO PCI.
|
|