Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191113_011
| CORONARY - Bifurcation/Left Main Diseases and Intervention | |
| Percutaneous Coronary Intervention to Severe Triple Vessel Disease with Total Left Main Occlusion Under Intra-Aortic Balloon Pump Support in Patient with Recent Anterior Myocardial Infarction | |
| Ho Ling Tsoi1, King Fun Tang2, Kwok Hing Yiu1 | |
| North District Hospital, Hong Kong, China1, Hong Kong Baptist Hospital, Hong Kong, China2, | |
|
[Clinical Information]
- Patient initials or identifier number:
CKS
-Relevant clinical history and physical exam:
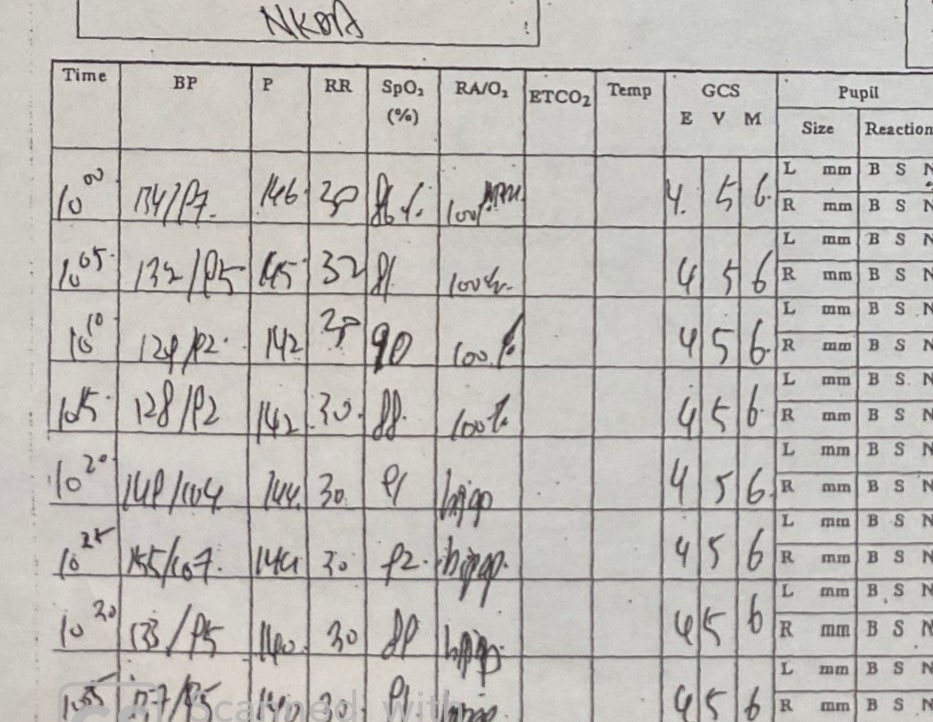
56/ M. Mr. CKS had history of HT, DM, IBD and hepatitis B. He experienced central chest pain for 10 days, which was non-exertional and was associated with dyspnea. On arrival to emergency department, his GCS was 15 / 15; BP 132 / 93mmHg; P 69 bpm; RR 26 / min; SpO2 86 % on 10 L / min O2. General physical examination showed cold peripheries and raised JVP. Chest auscultation noted bilateral basal crepitations, no audible heart murmur was heard. No lower limb edema was noted.
   -Relevant test results prior to catheterization:
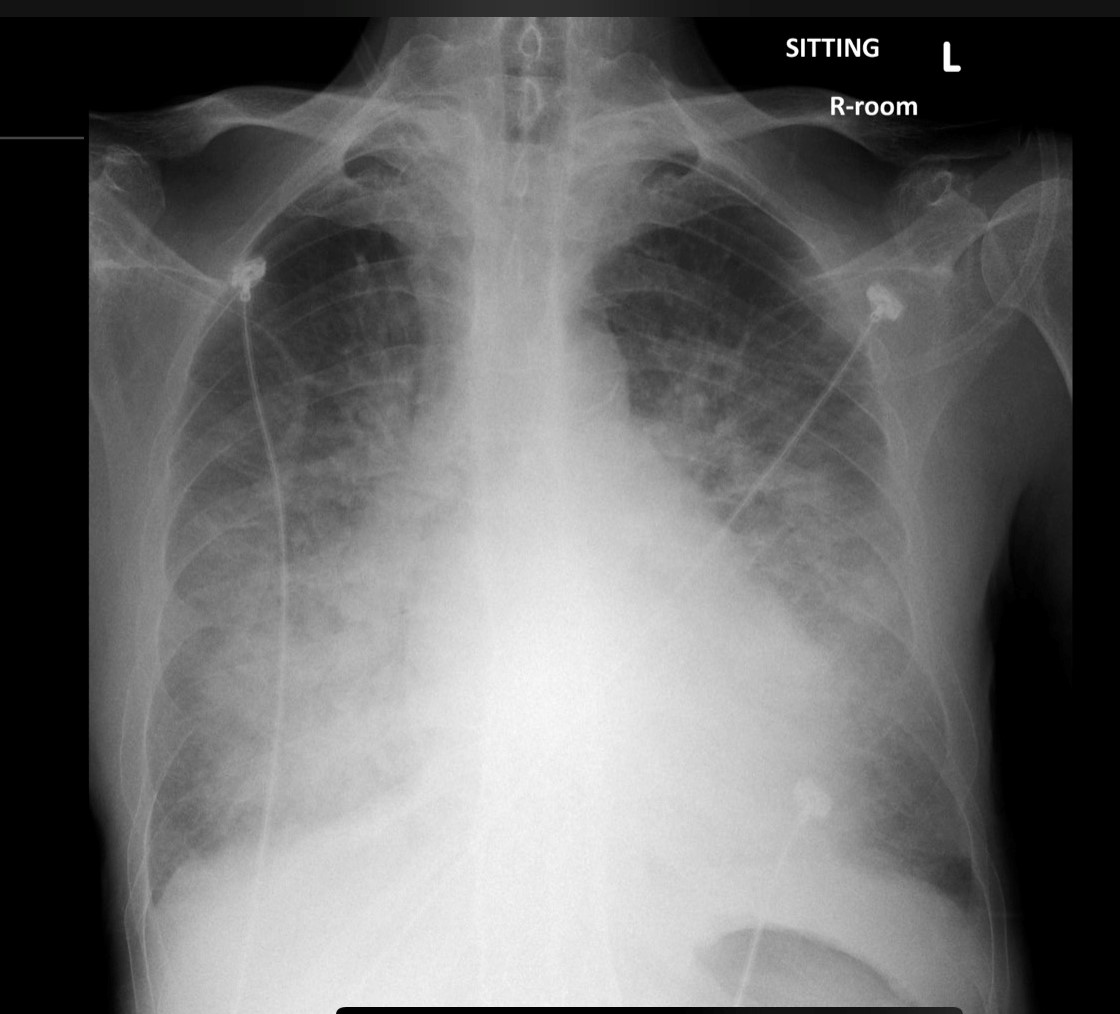
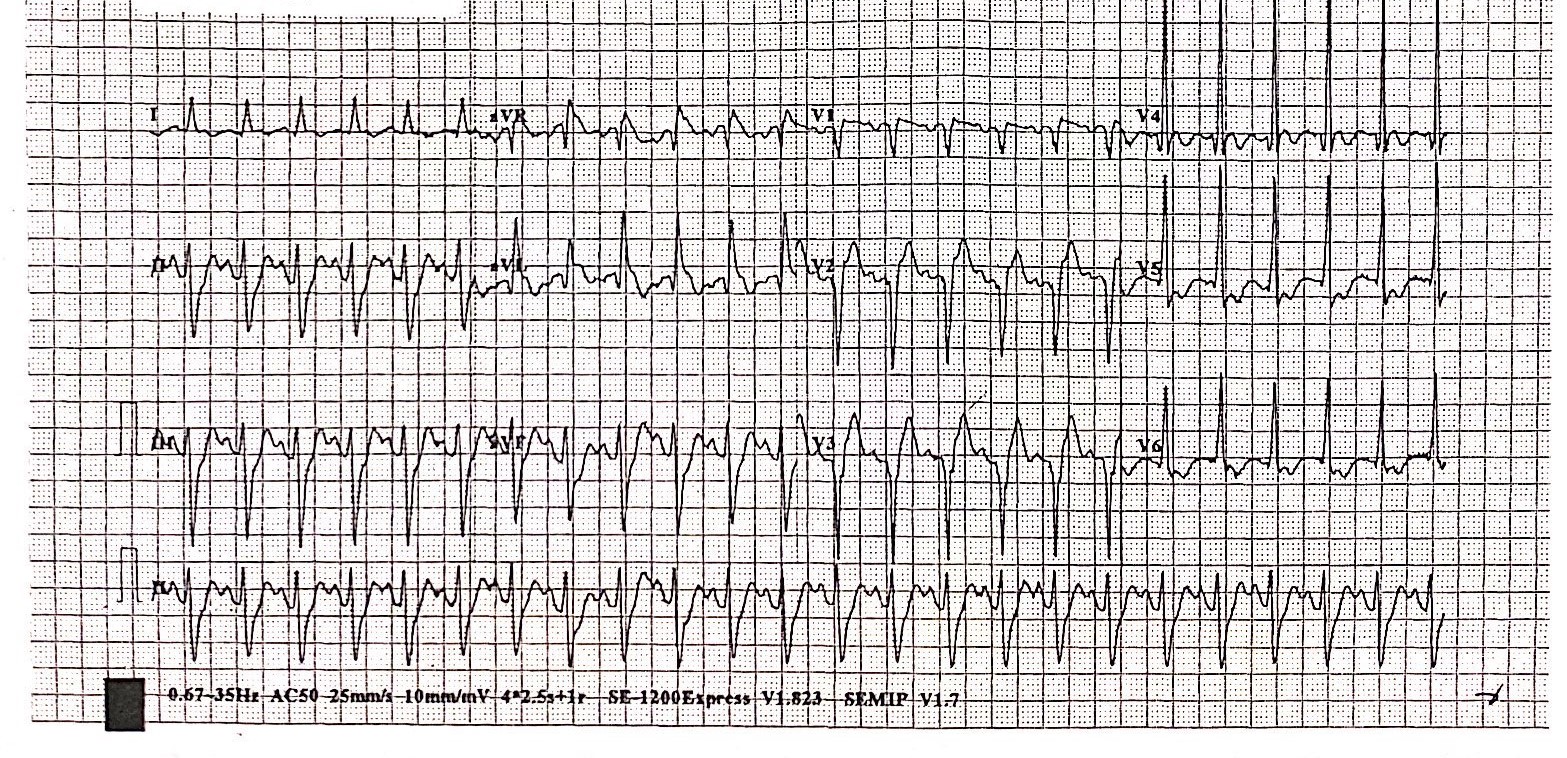
Blood capillary glucose 15 mmol / L and blood gas analysis showed type II respiratory failure. CXR: congested lung fields. ECG: sinus tachycardia 140 bpm, Q wave over anteroseptal leads with ST elevation. Bedside echo: Severe hypokinetic anterior and anteroseptal wall with LVEF 35%, mild MR and engorged IVC. Blood result revealed raised Troponin T level 871 ng / L; SCr 86 umol / L; ALT 111 U /L; Hb 14 g / dL; WBC 13 x10^9 / L. Clinical diagnosis was recent anterior myocardial infarction.
- Relevant catheterization findings:
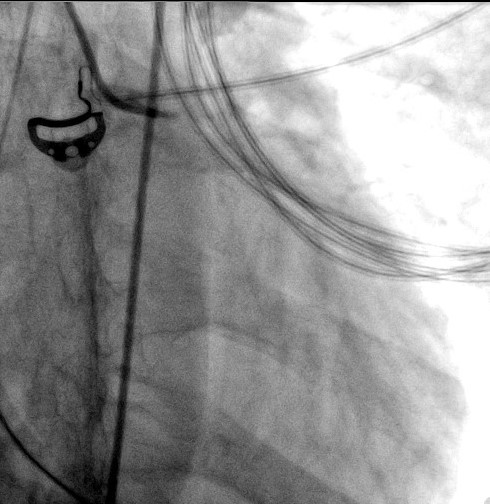
After initial stabilization in ICU, urgent coronary angiogram was done.
 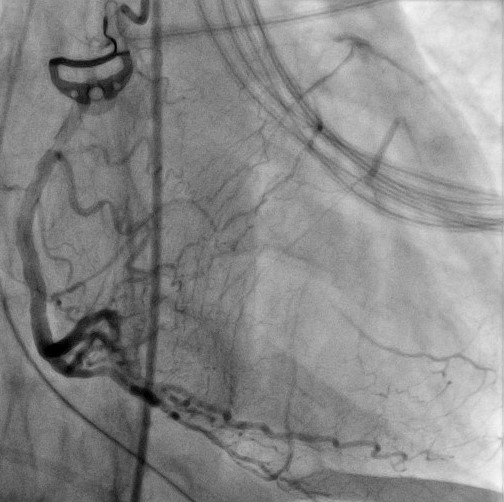 |
|
|
[Interventional Management]
- Procedural step:
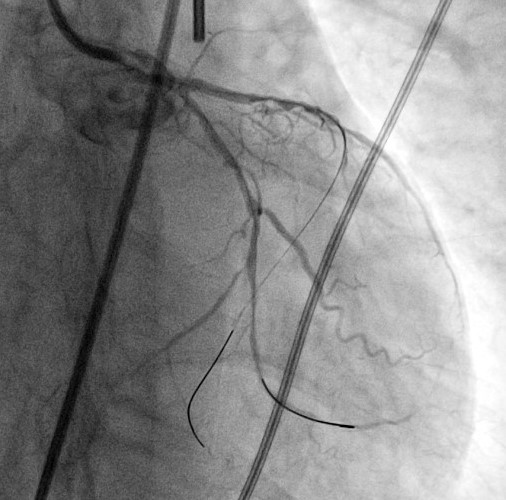
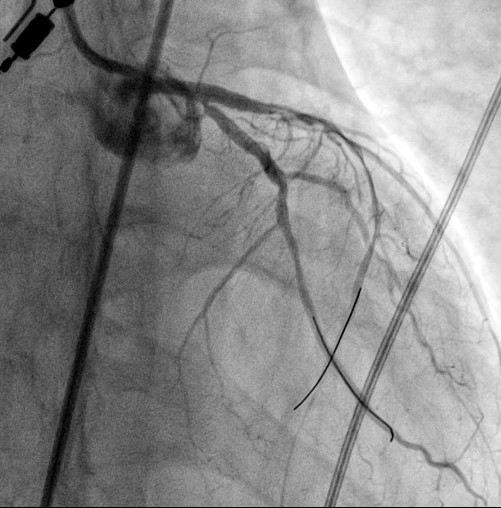
PCI was performed with femoral approach under IABP support. 6F JL4 guide was used.
  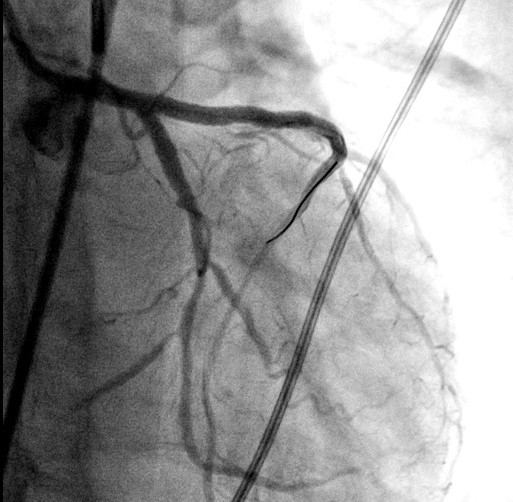 - Case Summary:
Patient eventually weaned off IABP support post PCI and heart failure medication was titrated. Cardiac rehabilitation was given post procedure and discharged home 10 days after PCI. Repeated Echo 3 months later showed improved LVEF 53% without regional wall motion abnormality.
|
|