Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191110_001
| CORONARY - Adjunctive Procedures (thrombectomy, atherectomy, special balloons) | |
| A Dialysis Case of Treated with Rotational Atherectomy and Orbital Atherectomy for Calcified Nodule | |
| Mitsunori Muto1 | |
| Kikuna Memorial Hospital, Japan1, | |
|
[Clinical Information]
- Patient initials or identifier number:
1834167
-Relevant clinical history and physical exam:
A 74-year-old male was admitted with chest discomfort on effort. He had been undergoing dialysis for 4 years. Previously he received PCI in September 2017, and implanted 3.0/18 mm EES in mid LAD, 3.5/28, 3.0/38 mm SES in mid RCA following Rotablator. In Jun 2018, he received PCI again and implanted 2.75/24, 2.5/28 mm EES in distal LAD following Rotablator, 3.0/12 mm EES in mid LCX. For calcified nodule at proximal LAD, we ablated with 2.25 mm Rotablator, and finish up with DCB.
-Relevant test results prior to catheterization:
In ECG, ST depression was shown in lateral to inferior area, however there was no finding of congestive heart failure in chest X-ray. Diffuse hypokinesis of LV function was revealed by ultrasound cardiography.
- Relevant catheterization findings:
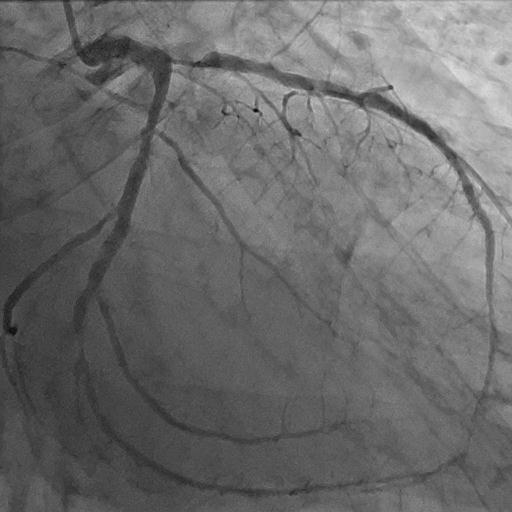
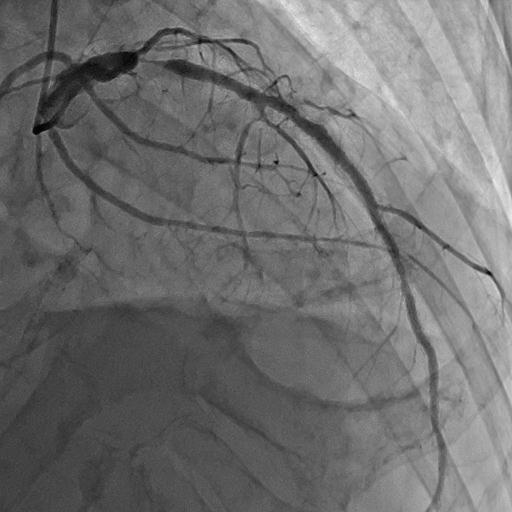
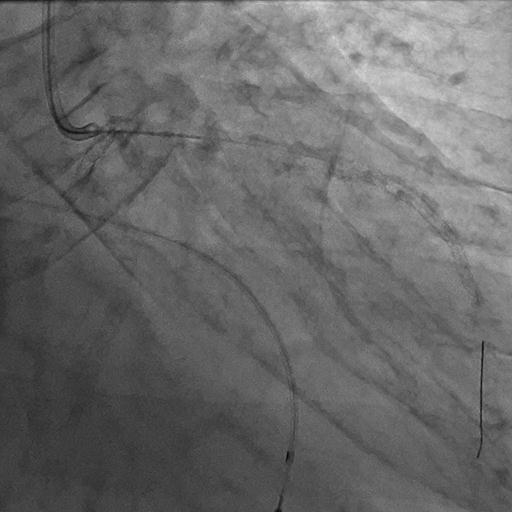
Because he was diagnosed recurrence of angina in September 2019, we performed coronary angiography. In RCA and LCX, there was no significant stenosis, however restenosis at proximal LAD lesion was revealed, so we performed PCI again for recurrence of calcified nodule.
   |
|
|
[Interventional Management]
- Procedural step:
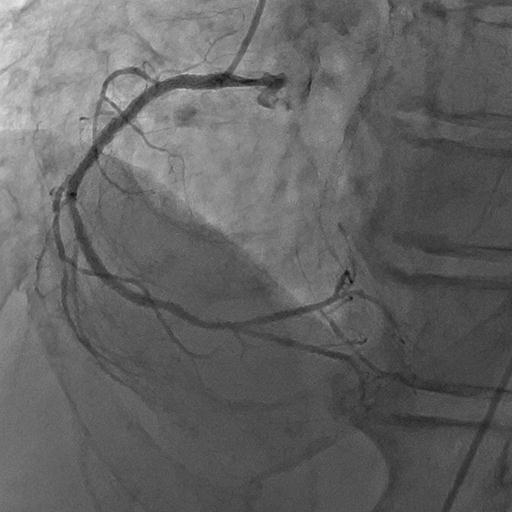
We used 8 French Q curve guiding catheter via femoral approach. Because in IVUS image mixture of soft plaque and calcified nodule were located at just proximal LAD, we tried ablation again with Rotawire Extrasupport and 2.0 mm Rotablator burr. We started ablation with 220,000 rpm. Wire bias was suitable for ablate the calcified nodule, however Rotablator was not effective in this time, because stable contact of the burr to calcified nodule was disturbed by large space at distal LMT. We considered that ablation during pulling movement would solve this problem, so we switched to ablation by orbital atherectomy with pulling movement. Following 1.25 mm orbital atherectomy with 80,000 rpm and 120,000 rpm, effective sanding of calcified nodule was revealed by IVUS. We dilated with 3.5 mm Cutting balloon repeatedly, and then finished up with 3.5 mm DCB.
   - Case Summary:
Evaluation of guide wire bias is crucial for debulking with Rotablator or Diamondback for calcified lesions. Because position of an IVUS catheter within the lumen and guide wire bias during rotational atherectomy is similar, ablation site would be predictable. In Rotablator, guide wire bias can be controllable by guiding catheter manipulation, location of platform, motion speed bias, and choice of Rotawire. If debulking device cannot keep stable contact to calcium like this case, choice of Rotablator or Diamondback might improve guidewire bias by selection of debulking direction.
|
|