Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191031_016
| CORONARY - Acute Coronary Syndromes (STEMI, NSTE-ACS) | |
| Primary Percutaneous Coronary Intervention in a Calcified Left Anterior Descending Artery | |
| Julian Tey1, Abdul Raqib Abd Ghani1, Kamaraj Selvaraj2 | |
| Hospital Serdang, Malaysia1, Sultan Idris Shah Serdang Hospital, Malaysia2, | |
|
[Clinical Information]
- Patient initials or identifier number:
MSA
-Relevant clinical history and physical exam:
A 62-year-old male with cardiovascular risks of hypertension and chronic active smoker, presented to district hospital with acute onset severe chest pain. ECG showed ST elevation on leads V1-V4, acute anterior ST elevation myocardial infarct. Clinically, blood pressure 130/80 mmHg, heart rate 90 beats per minute. Cardiovascular and lungs examinations were unremarkable. He was consented and referred to hub hospital for primary percutaneous coronary intervention via STEMI Network.
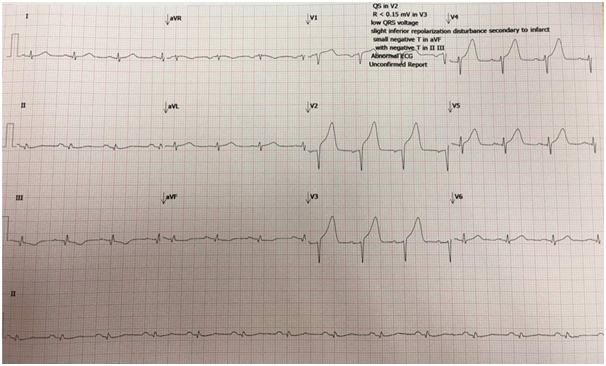 -Relevant test results prior to catheterization:
- Relevant catheterization findings:
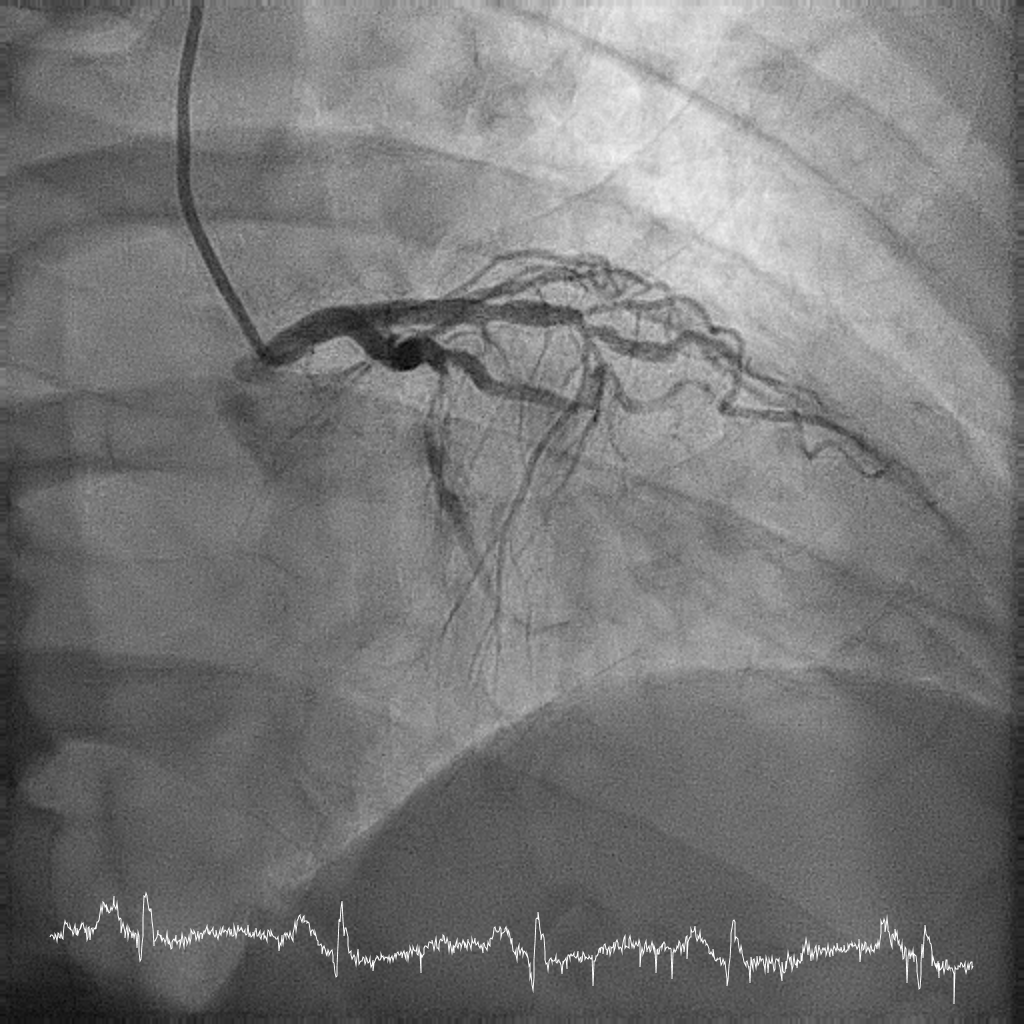
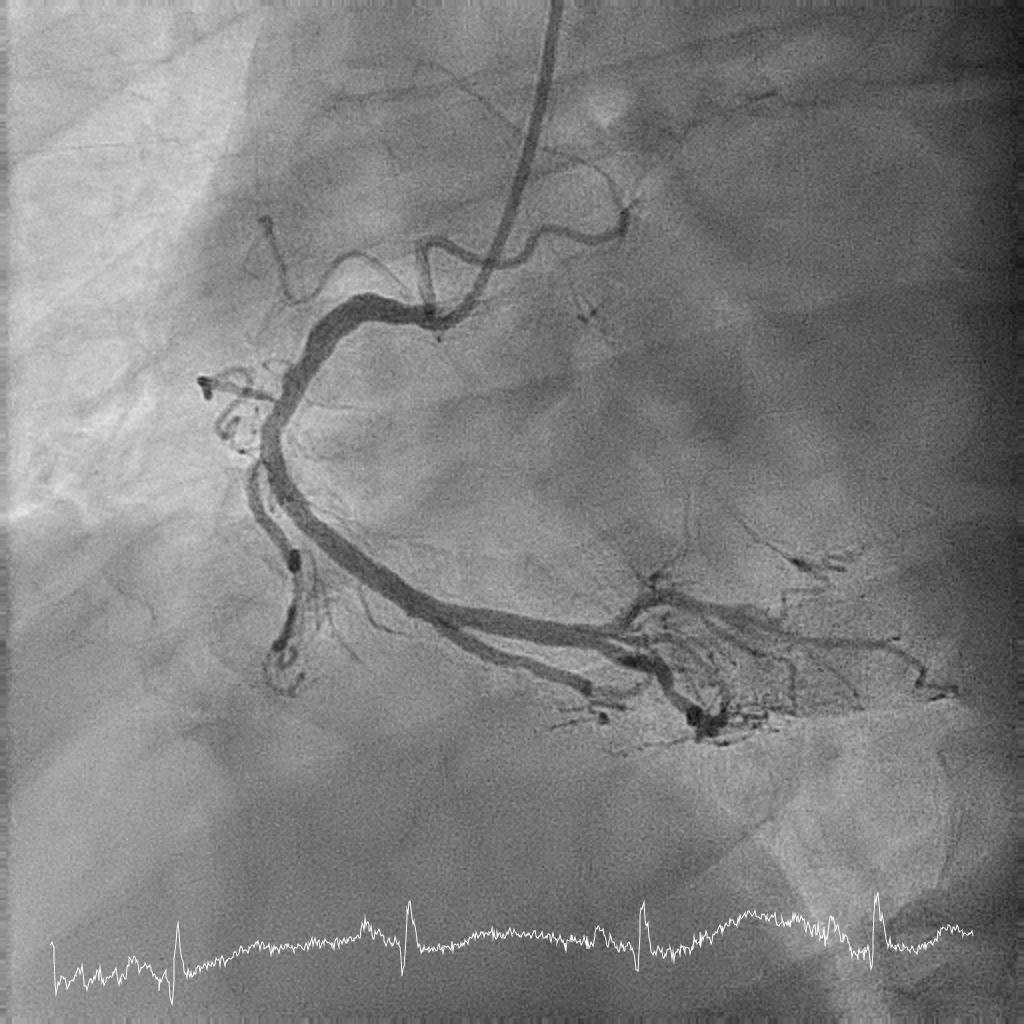
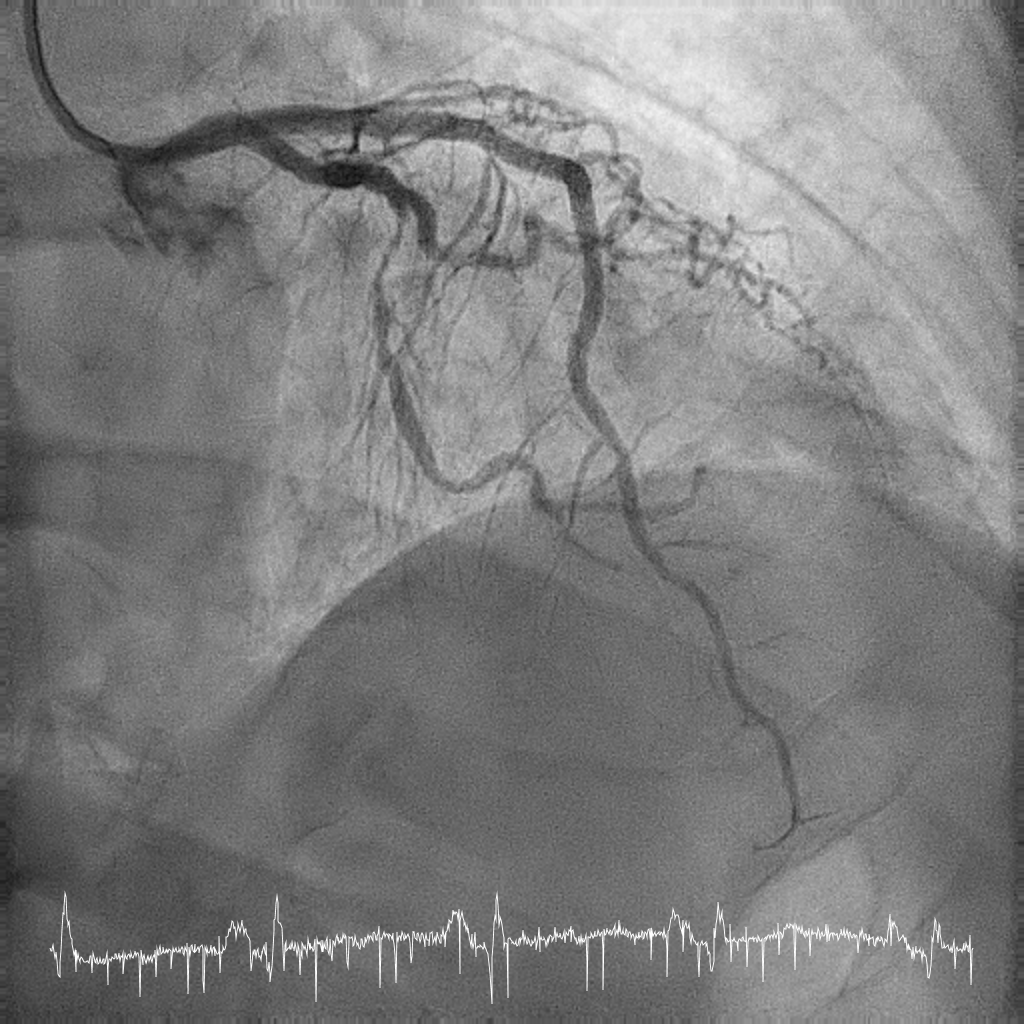
Right radial approach diagnostic coronary angiogram showed smooth left main stem, acute total occlusion at mid left anterior descending (LAD) culprit artery, there is also 90% stenosis at mid to distal left circumflex artery (LCX) and mild disease at proximal right coronary artery (RCA).
  |
|
|
[Interventional Management]
- Procedural step:
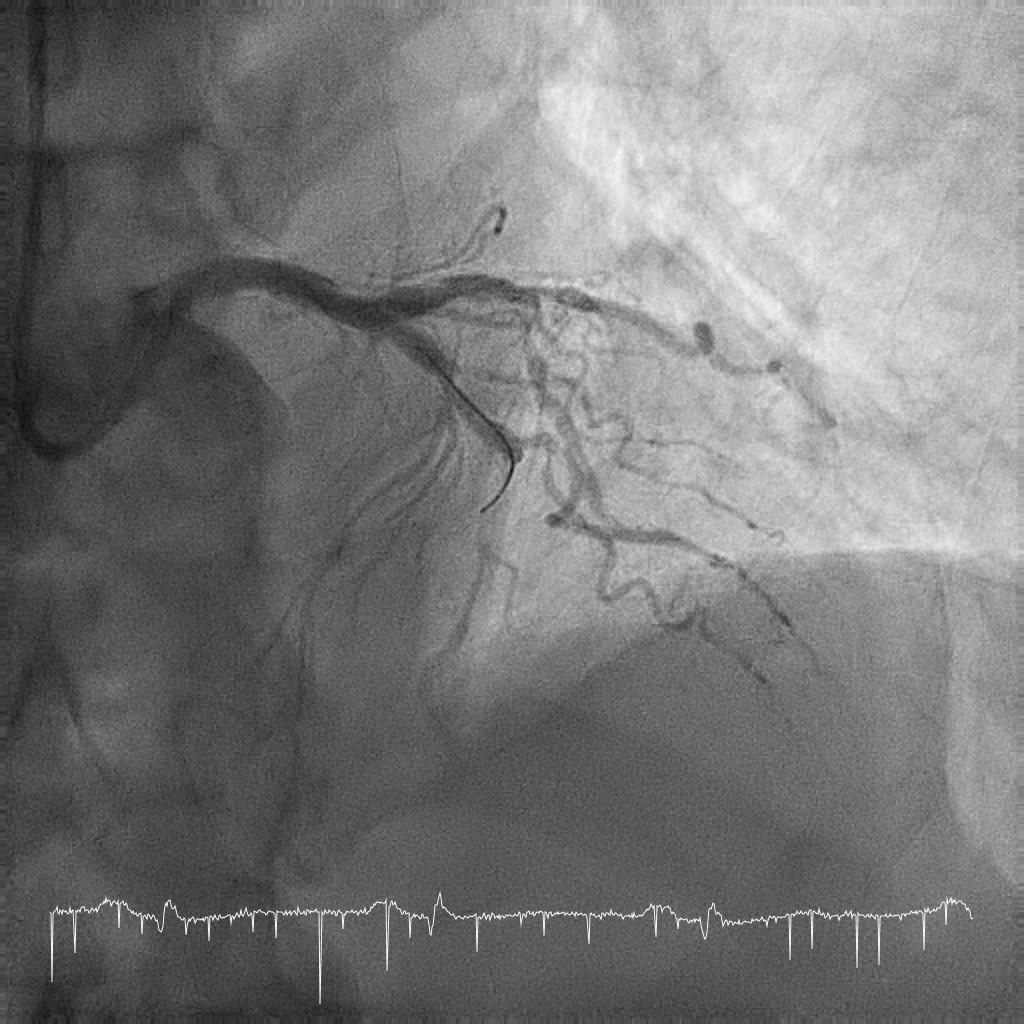
Patient was loaded with dual antiplatelet (Aspirin and Ticagrelor) and was given bolus dose of intravascular glycoprotein IIb/IIIa inhibitor (Tirofiban). Soft coronary wire (BMW) wired down LAD and followed with thrombus aspiration with (Export Advance). Post aspiration angiogram revealed a significant stenosis from proximal to mid LAD with heavy calcification. TIMI 3 flow achieved distally. Sequential pre-dilatation with semi-compliant balloon (Tazuna) 2.5 mm x 15 mm and later on upsized to scoring balloon (Scoreflex) 2.5 mm x 15 mm. The dilating balloons were not fully expanded and stenotic area remained tight. Decision to modify the calcification segment with rotational atherectomy was made. (BMW) wire exchanged to Rota floppy wire using microcatheter (Finecross). Rotablation atherectomy performed with 1.5 mm burr size at 180000 rpm smoothly. Wire exchanged back to BMW. Subsequent dilatation with 2.5 mm x 15 mm non-compliant balloon (Euphora NC) was easier with full expansion. Well prepared vessel implanted with drug eluting stent (Resolute Onyx) 2.75 mm x 36 mm at the mid to distal LAD while another drug eluting stent (Resolute Onyx) 3.0 mm x 30 mm overlapped at proximal to mid LAD and followed with post dilatation with non-compliant balloon (Euphora NC) size 3.5mm x 15mm at high pressure. Final result showed a good TIMI 3 flow without immediate complications.
   - Case Summary:
Patient was stable and sent back to spoke hospital as there was shortage of CCU and HDW beds in the hub hospital. He was discharge 3 days later and remained well on subsequent follow up. Rotational atherectomy is rarely performed in primary PCI as it may complicate with slow flow, distal embolization of thrombus and risk of perforation in an angry and fragile vessel. But in a crucial situation like in this case, radial approach rotational atherectomy is needed to modify a calcified vessel prior to successful stents implantation and good outcome. Indeed, the procedure was done very cautiously in experienced hands with anticipation of all possible complications that may arise.
|
|