Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191029_007
| IMAGING AND PHYSIOLOGIC LESION ASSESSMENT - Imaging: Intravascular | |
| Exploration of Image: The Key Role of Optical Coherence Tomography in Identifying an Atypical Unstable Angina Pectoris | |
| Hehe Cui, Hui Chen3 | |
| , Beijing Friendship Hospital, China3, | |
|
[Clinical Information]
- Patient initials or identifier number:
DJR
-Relevant clinical history and physical exam:
A 57-year-old postmenopausal woman was admitted to hospital because of no-cause intermittent chest pain without symptoms of exertional angina for one week. She has a history of mild hypertension and dyslipidemia for 5 years under lifestyle and diet control, and a smoking history (cessation for 10 years). Her younger brother was attacked by acute myocardial infarction in his 50s. Her physical examination was unremarkable.(Bp 138/66 mmHg, heart rate at 53 bpm, no vital positive sign)
-Relevant test results prior to catheterization:
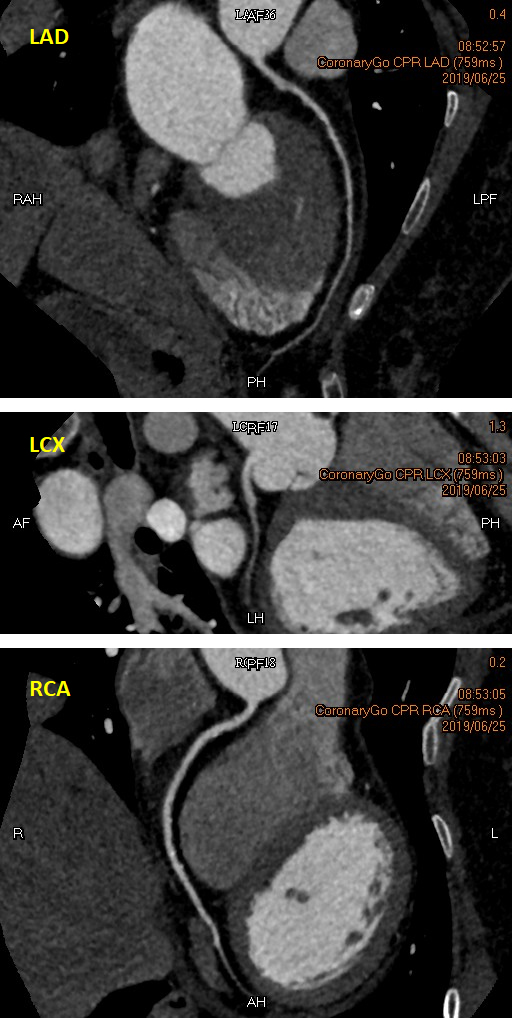
Cardiac troponin T, Cardiac troponin I, N terminal pro B type natriuretic peptide and creatine kinase-MB tests were negative. Echocardiogram showed good ejection fraction (78 %) and no wall motion abnormalities. Her electrocardiogram was normal. A non-invasive coronary computed tomographic angiography (CTA) showed an atherosclerotic plaque with a moderate stenosis in the proximal left descending artery (LAD). No obvious stenosis was found in other coronary arteries.
 - Relevant catheterization findings:
Although the coronary CTA showed mild lesions, the patient insisted to be examined by a coronary angiogram (CAG) because she was frightened by the heart attack on her brother. The CAG showed a 50 % - 60 % stenosis in the proximal to mid LAD, a normal left circumflex artery, and an atherosclerotic plaque without obvious stenosis in the proximal right coronary artery.
|
|
|
[Interventional Management]
- Procedural step:
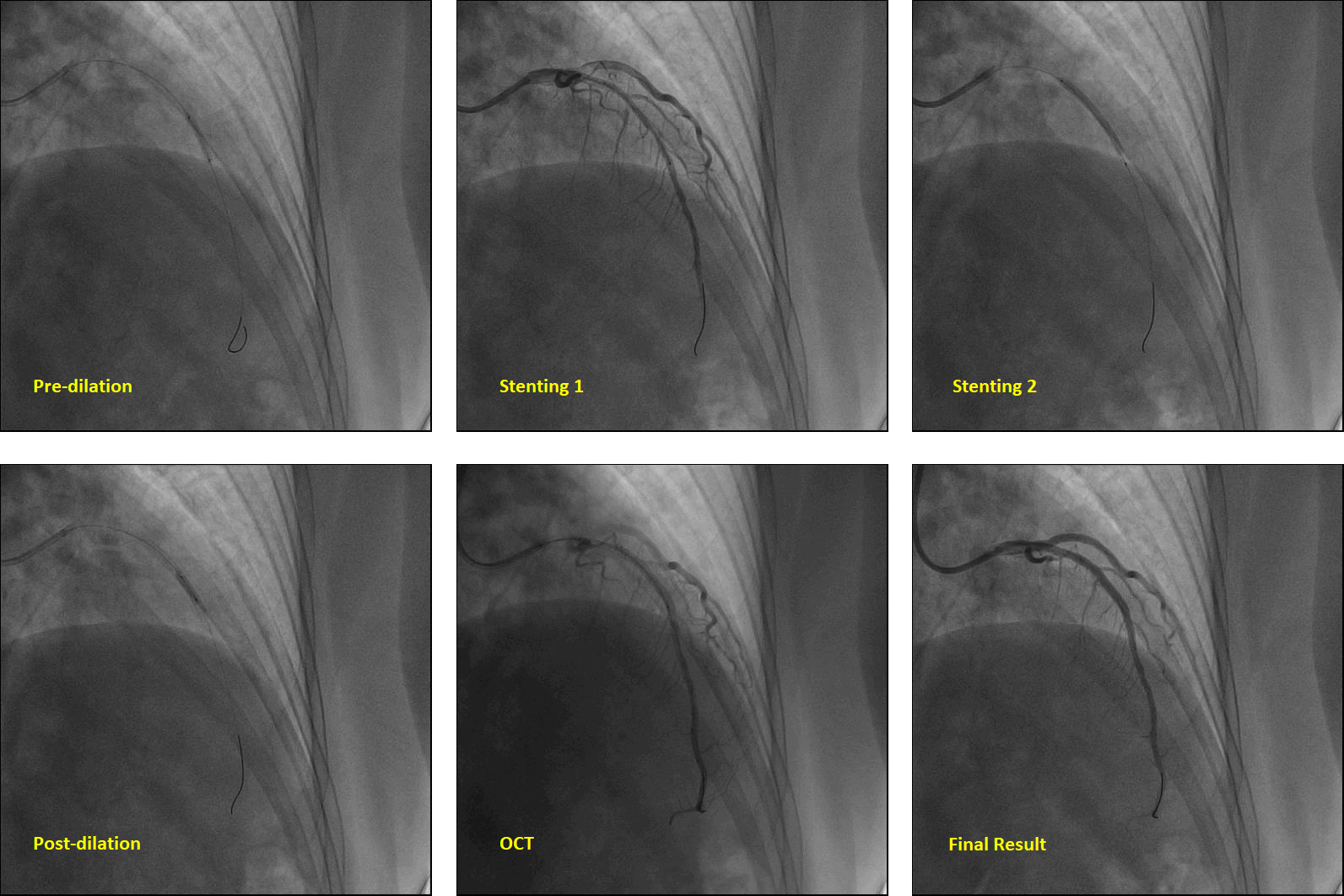
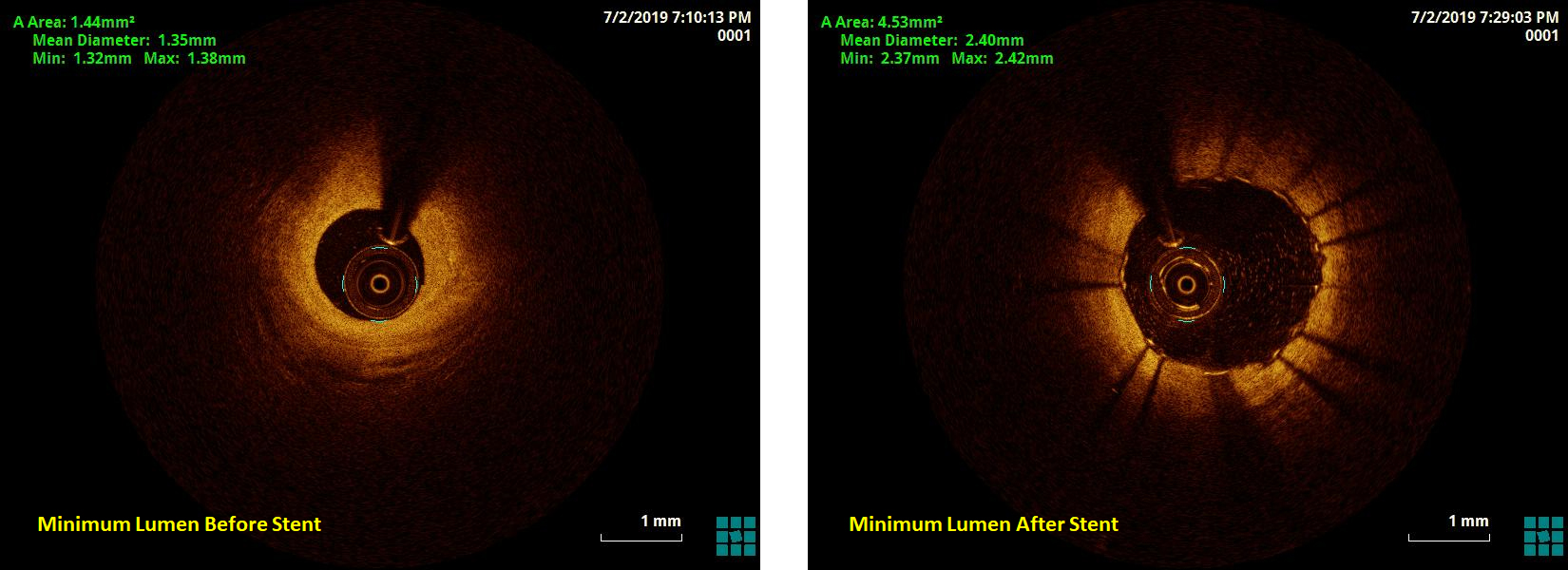
We performed optical coherence tomography (OCT) to clarify the borderline lesions in LAD. The result found a surprisingly severe stenosis in the proximal to mid LAD. The minimum area is only 1.44 mm2 (77% narrowing of proximal reference lumen), the mean diameter is 1.35 mm. The lesion is a mixed plaque with a fibrous cap, some lipid content, a little calcification and intraplaque vasa vasorum as the OCT movie showed. Then revascularization was performed. A pre-dialation balloon (2.5 * 15 mm, Cordis, Hialeah, Florida 33014, United States) was used for predilation at 10 atmospheric pressure (atm). A stent (2.5 * 32 mm, Promus PREMIER, Boston Science, Marlborough, MA 01752) was deployed at 8 atm into the proximal to mid LAD, and a non-compliance balloon (2.75 * 9 mm, NC Sprinter, Metronic, Minneapolis, MN 55432) was used to post-dialate the stent at 16-18 atm. OCT image after stenting showed the minimum intra-stent lumen area was 4.53 mm2, and the stent was well attached.
  - Case Summary:
During follow-up, the patient complained the symptoms were completely relieved. Optical coherence tomography provides a superior resolution (10 ¥ìm) of plaque morphology. Compared with CT and angiogram, Additional use of intracoronary imaging techniques facilitates the diagnosis of coronary artery disease and the management of lesions in uncertain cases.
|
|