Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191028_003
| IMAGING AND PHYSIOLOGIC LESION ASSESSMENT - Imaging: Intravascular | |
| Accidental Finding of Optical Coherence Tomography | |
| Pei Lin1, Chen Wei Huang2 | |
| National Cheng Kung University Hospital, Taiwan1, An Nan Hospital, Taiwan2, | |
|
[Clinical Information]
- Patient initials or identifier number:
08365634 Wu
-Relevant clinical history and physical exam:
This 72 year old man sufferedfrom anterior MI status post LAD BMS 12 years ago.He had recurrent angina two yearsago. Tl-201 myocardium stress test showed mixed viable andnon-viable myocardial tissues in anteroseptal,anterolateralwall, andapex. He refused coronary angiography at that time. After optimized medical treatmenthis symptom alleviated.
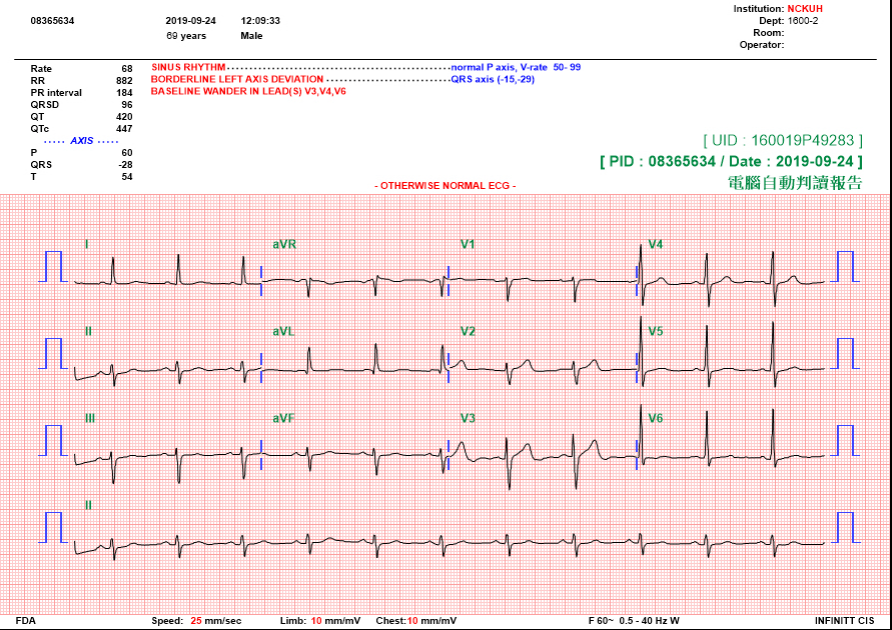
Angina recurred one month agowith response to nitroglycerin. No obvious changes in EKG. No active lesion in chest x-rayClear breathing sounds.  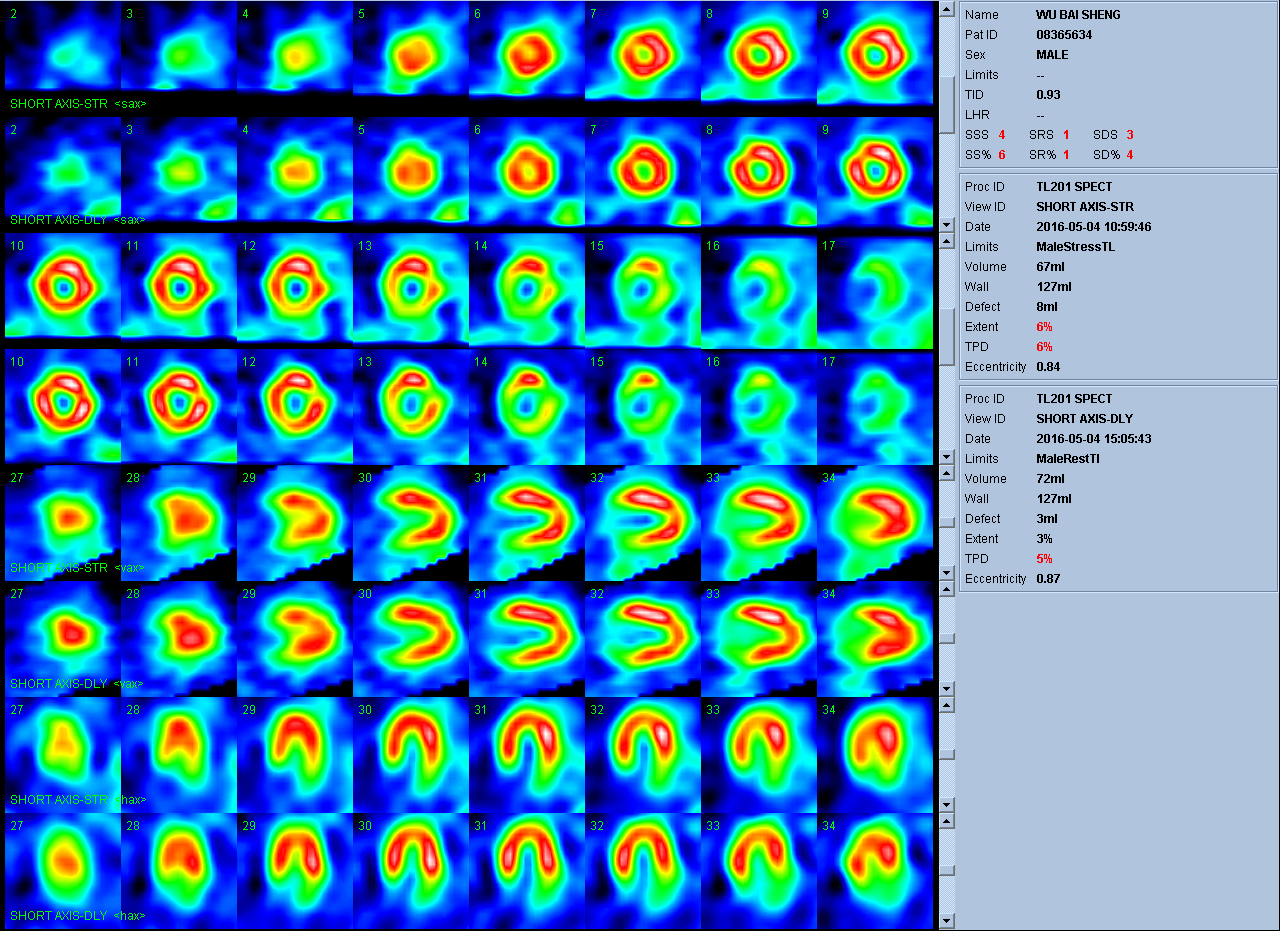 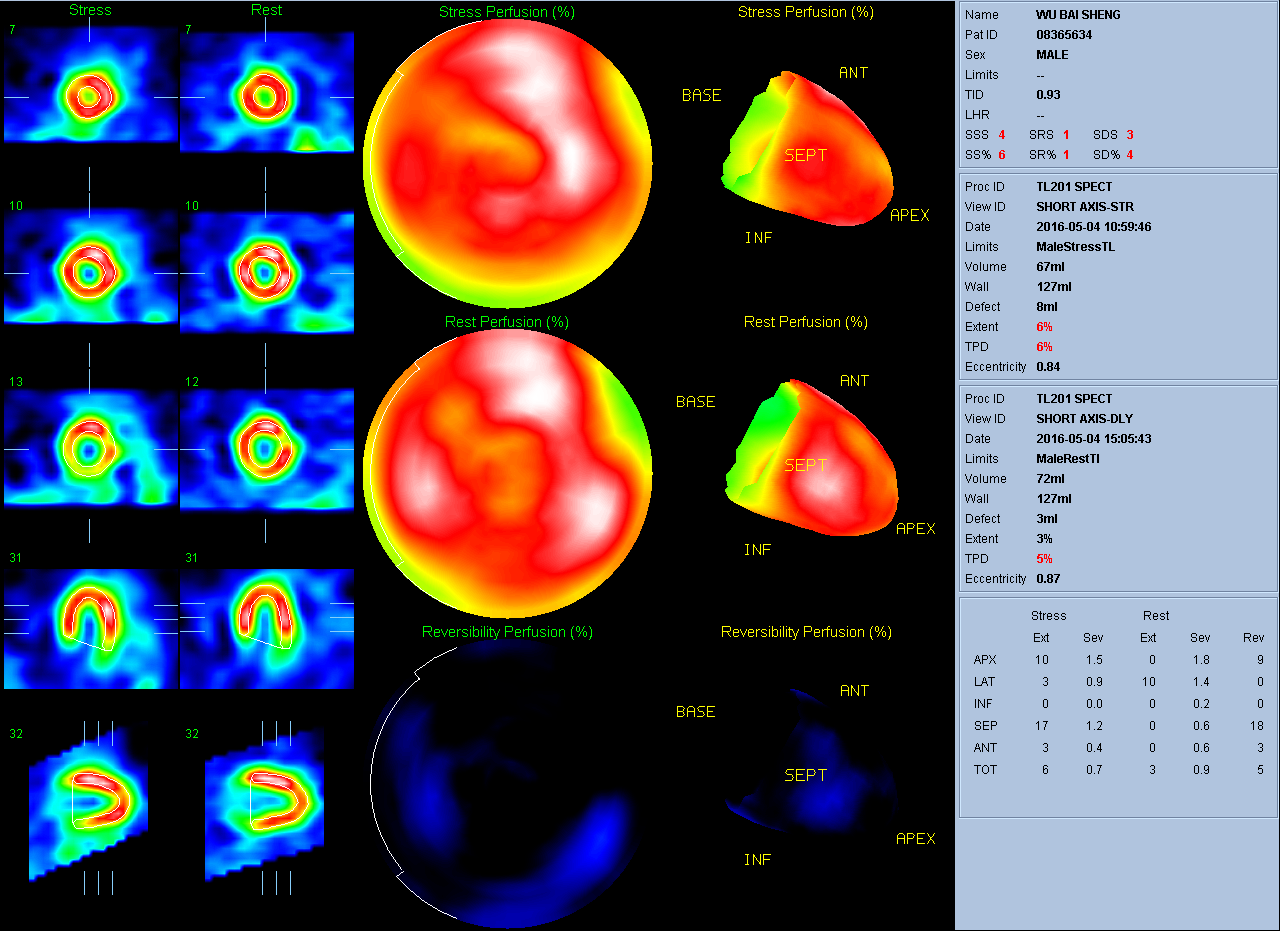 -Relevant test results prior to catheterization:
Echocardiography showed adequate LV systolic function without regional wall motion four months ago.EKG showed sinus rhythm with borderline left axis deviation.
 - Relevant catheterization findings:
Left Main: Atherosclerosis with 40%stenosis at distal part of LM LAD: Diffuse atherosclerosis with 75% stenosis of de novo lesion atthe middle part of LAD LCX: Chronic total occlusion from the proxiaml part ofLCX RCA: Diffuse atherosclerosis with 80% stenosis at the proximal part of RCAand a critical stenosis at the small branch of PL
Catheterization diagnosis: CAD-3VD with LAD de novo lesion progression. |
|
|
[Interventional Management]
- Procedural step:
1.We used a EBU 4.0 SH guiding cathete to engage LM orifice.2.The Fielder FC wire to distal LAD.3.OCT couldn't pass the proximal part of LAD. We thought that our wire might pass through the stent strut of the previous stent so we rewired again. After rewiring the OCT could pass smoothly.4.OCT showed two deformation sites of previous stent and our wire was in the false lumen (out side the previous stent). The most stenosis site was 2.5mm. The diameters of distal normal landing zone was 3.5 mm.5.We rewired back to the true lumen and dilated middle LAD with SapphireII balloon (1.5*15 mm). 6.After balloon dilatation the OCT could pass smoothly to the true lumen.7.We checked OCT again to confirm that we were in the true lumen.8.We used an NC Quantum Apex balloon (3.5*15 mm) to dilate proximal to middle LAD with 24 bars and an NC Euphora balloon (4.0*12 mm)to dilate proximal LAD with 16-20 bars.9.A Kaname stent (3.5*2 8 mm) deployed at proximal to middle LAD.10.We used an NC Euphora balloon (4.0*12 mm) to post dilate proximal to middle LAD with 20 bars and an NC Euphora balloon(4.5*8 mm) to post dilate proximal LAD with 16-18 bars.11.Final angiography and OCT showed a good result with well-positioned and fully expanded stent.
- Case Summary:
Final angiography and OCT showed a good result withwell-positioned and fully expanded stent.
|
|