Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191022_005
| CORONARY - Acute Coronary Syndromes (STEMI, NSTE-ACS) | |
| So Close, Yet So Far | |
| Yuen Fung Yiu1, Ping Tim Tsui2 | |
| Princess Margaret Hospital, Hong Kong, China1, Gleneagles Pro-HEART Cardiac Centre, Hong Kong, China2, | |
|
[Clinical Information]
- Patient initials or identifier number:
MH
-Relevant clinical history and physical exam:
A 54-year-old man with diabetes, hypertension and a history of ischemic stroke was admitted in September 2019 for NSTEMI. On admission, he was hemodynamically stable. He had 2 episodes of acute coronary syndrome with PCI performed in 2014 and 2018 respectively, with a total of three stents placed in the LAD. Both procedures were performed at another hospital and the angiograms were not accessible in our centre.
-Relevant test results prior to catheterization:
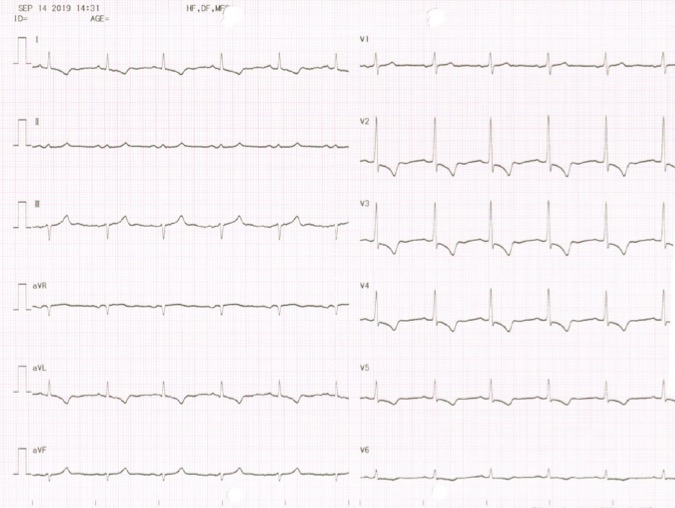
ECG showed ST segment depression and T wave inversion over V2-V5. Troponin I was elevated at 2000 ng/L.
 - Relevant catheterization findings:
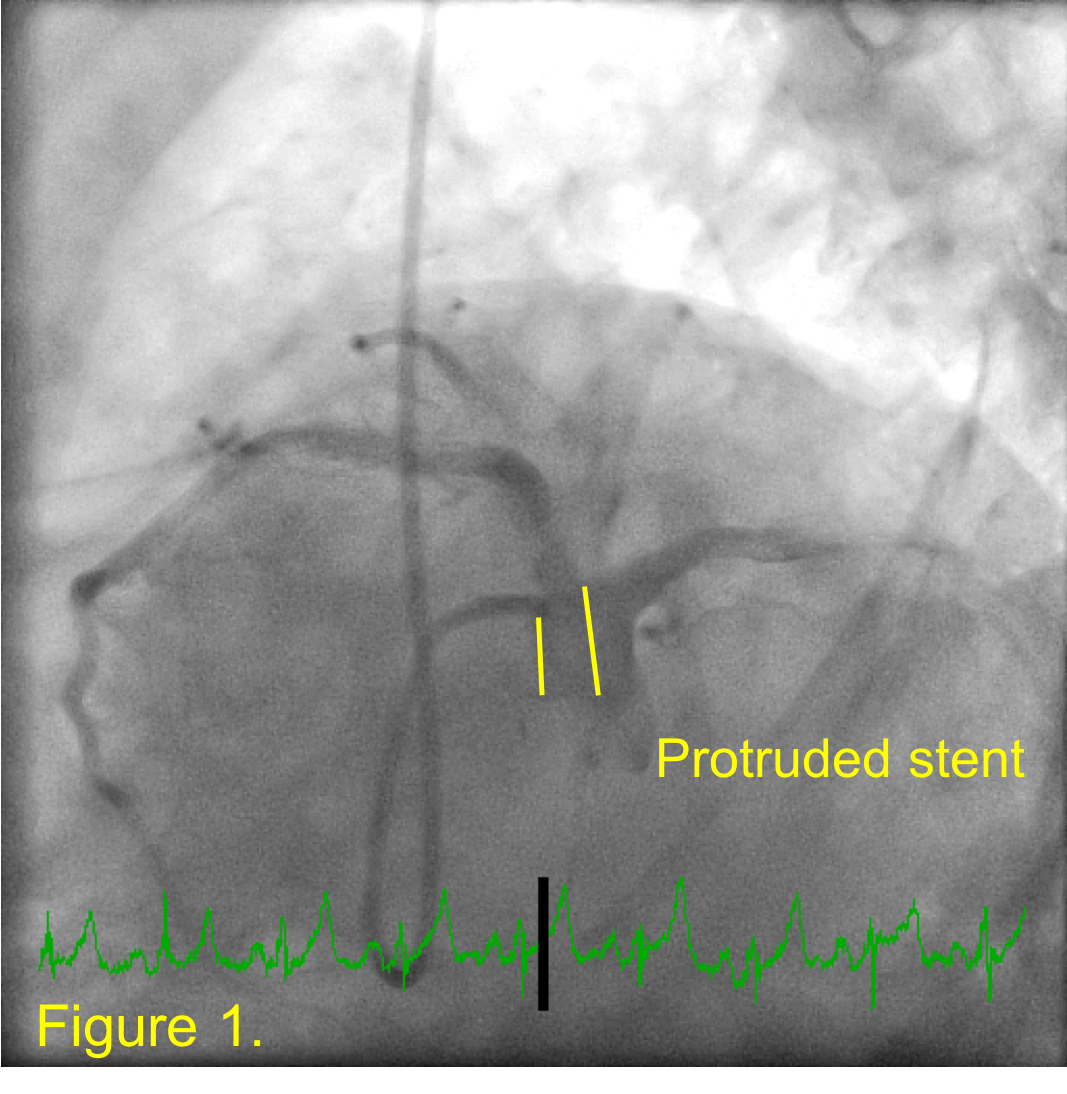
Urgent coronary angiogram was performed and showed separate origins of LAD and LCX. JL 3.5 and JL 4 diagnostic catheters were used to engage LAD and LCX respectively. The ostial LAD stent has protruded into the aortic root by approximately 6mm (Figure 1), which was not mentioned in the previous record. There was a severe in-stent restenosis over proximal LAD and moderate diffuse in-stent restenosis over middle part of LAD (Video 1). There was only mild disease in the LCX and RCA.
 |
|
|
[Interventional Management]
- Procedural step:
A 6 Fr radial sheath was inserted through the left radial artery. Difficulties was encountered while engagement of the LAD using IL3.5 guide catheter due to significant stent protrusion. A wire was used to pass through the side struts of the protruded stent but IVUS catheter or PTCA balloon could not be advanced. To avoid crushing or damaging the stent, we re-attempted to engaged the ostium of the protruding stent.
However, repeated attempts to engage the stent ostium using different guiding catheter (IL3.5, JL3.5, EBU3.0, EBU3.5) by both left radial and femoral approach with and without guide extension were unsuccessful (Video 2). Wiring the stent ostium with the help of double-lumen catheter also failed. Eventually, a 6 Fr JL3.5 diagnostic catheter was able to intubate the protruding stent after manipulation. Sion Blue wire was passed into LAD and connected to an extension wire. Under fluoroscopic guidance, the diagnostic catheter was carefully removed while maintaining the distal tip position of guidewire. The JL 3.5 guiding catheter was successfully advanced through the wires and coaxially engaged the protruded stents (Video 3). After IVUS confirmation, the proximal LAD lesion was stented with a 3.5/22mm DES and the middle part of LAD was treated with 3.0/30mm drug-coated balloon with good results (Video 4). - Case Summary:
This case illustrates the challenges of intervention of a significantly protruded aorto-ostial stent and highlights the importance of clear documentation of any stent protrusion at the end of procedure. In our patient, the presence of separate LAD and LCX ostia further complicated the procedure as the guide catheter had a tendency to bias towards the LCX. Despite having the same JL curve, only the diagnostic catheter could engage the stent ostium. This demonstrated that diagnostic catheters tend to engage better than guide catheters due to better flexibility and recoil properties and the above technique can be used when difficulty in engaging guide catheter is encountered.
|
|