Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191018_005
| CORONARY - Bifurcation/Left Main Diseases and Intervention | |
| Solving the Ostial Left Anterior Descending Restenosis Puzzle with Intracoronary Imaging | |
| Ashok B. Malpani1, Krishnarpan Chatterjee2 | |
| BM Birla Heart Research Centre, India1, University Hospital Southampton NHS Foundation Trust, United Kingdom2, | |
|
[Clinical Information]
- Patient initials or identifier number:
Mr SEM
-Relevant clinical history and physical exam:
Fifty seven yearknown diabetic with history of angioplasty to RCA (2005) and LAD(2015) for CCS class II stable angina, presented with angina at rest lasting 30 mins. He was diagnosed with unstable angina atanother centre and managed conservatively. He was stabilizedmedically with dual antiplatelets, enoxaparin, statins andantianginals. Coronary angiogram was done at the admitting centrewhich showed patent stent in RCA with in-segement restenosisinvolving ostial LAD and referred for PCI.
-Relevant test results prior to catheterization:
ECG (during episodeof angina) - dynamic ischaemic ST-T changes in anterior leads, whichhad reverted to baseline with medical management prior to PCI.Echocardiography:Normal LV systolic function, no regional wall motion abnormality.Quantitativetroponin T was not raised (<0.006 ng/mL)Complete blood countand renal function were within normal limits.
- Relevant catheterization findings:
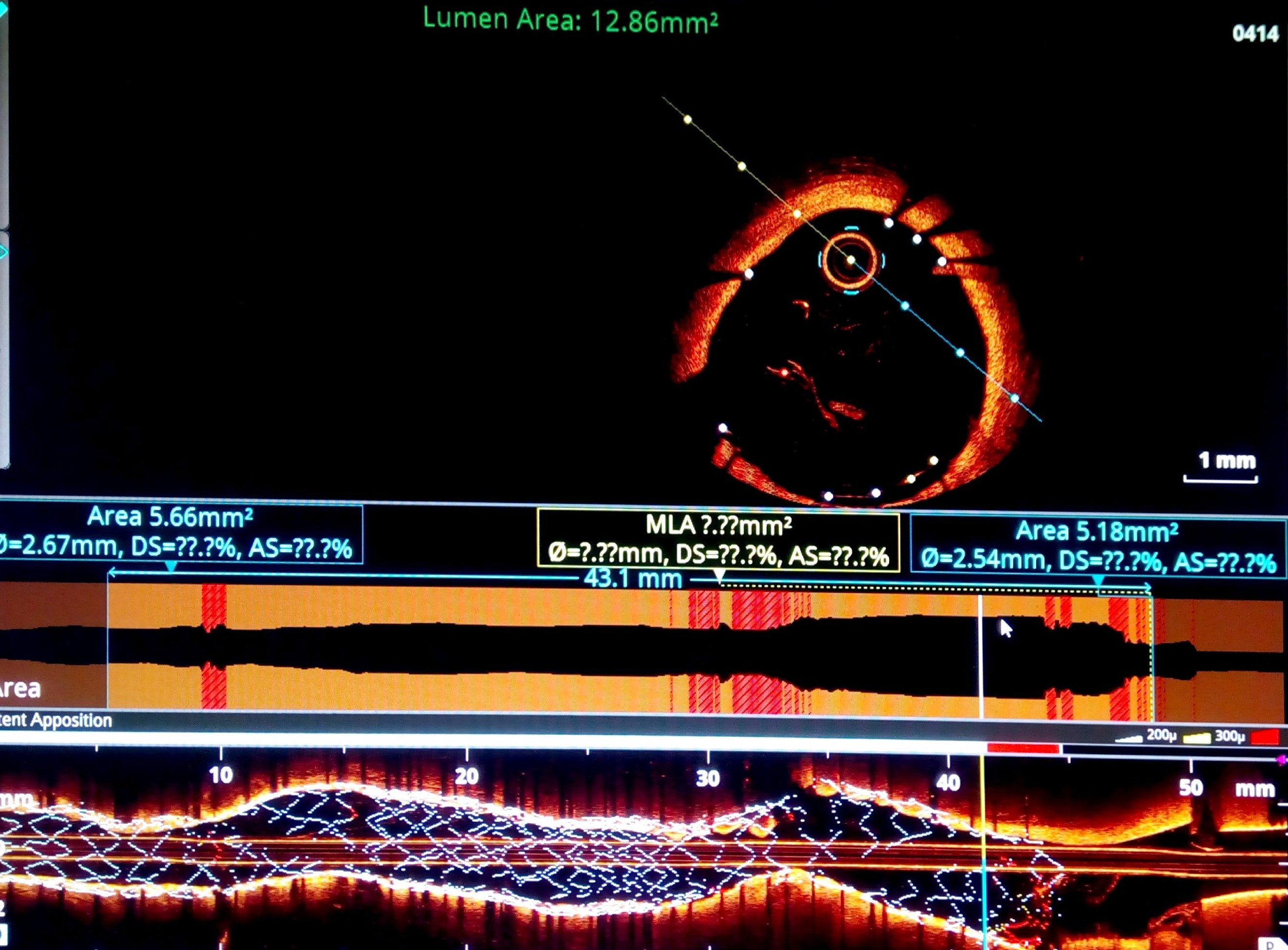
Severe in-segmentrestenosis extending from proximal LAD stent edge to ostium of LADwith heavy calcium. Plaque extending into distal left main. Ramusostia was free of disease. Pre PCI OCT pullback from LAD to LM showedchunk of calcium in ostial LAD (4-6 o'clock) with Ramus ostia free ofdisease. Medina (0,1,0). Ostioproximal LAD luminal area was 2.99 sq mm, distal LMluminal area was 7.67 sq mm. Average diameter of proximal LAD landingzone was 3.3 mm and LM shaft landing zone was 4.1 mm.
|
|
|
[Interventional Management]
- Procedural step:
Provisional LM to LAD stenting with a 3 x 26 zotarolimus eluting stent (Resolute Onyx) was planned as per the pre PCI OCT. Stent was deployed at nominal pressure after which ostial LAD remained underexpanded. LAD ostia was post-dilated at 24 atm pressure with 3x10 noncompliant balloon. There was plaque shift leading to compromise of ramus ostia. Ramus ostia was recrossed and kissing balloon dilation done with 3 mm balloon in LAD and 2.75 mm balloon in ramus. LM was then post-dilated with 4x10 semi-compliant balloon. Post PCI OCt revealed a well expanded and apposed stent with widely open ramus ostia. Ostial LAD luminal area was 7.47 sq mm and distal LM was 12.06 sq mm.
 - Case Summary:
This case shows why ostial LAD lesions require meticulous planning with intracoronary imaging. OCT allowed precise characterization of the lesion and assessment of the calcium at the LAD ostia.
As the calcium subtended an angle of around 60%an upfront strategy of atherectomy was not considered necessary. Even though post-dilation of LAD ostia led to plaque shift into the ramus ostia, this was managed with recrossing wire into ramus and kissing balloon dilation. Post PCI OCT showed precisely how the stent had apposed well to the differing luminal diameters of the LAD and LM. Ostial LAD lesions should ideally be manged with a provisional single stent approach with OCT guidance. |
|