Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20191018_001
| CORONARY - Stents (bare-metal, drug-eluting) | |
| The Patient at High Risk of Bleeding Is Indicated for Percutaneous Coronary Intervention, What Should We Do? | |
| Quan Manh Nguyen1, Hung Manh Pham1 | |
| Vietnam National Heart Institute, Vietnam1, | |
|
[Clinical Information]
- Patient initials or identifier number:
Luu Quang B.
-Relevant clinical history and physical exam:
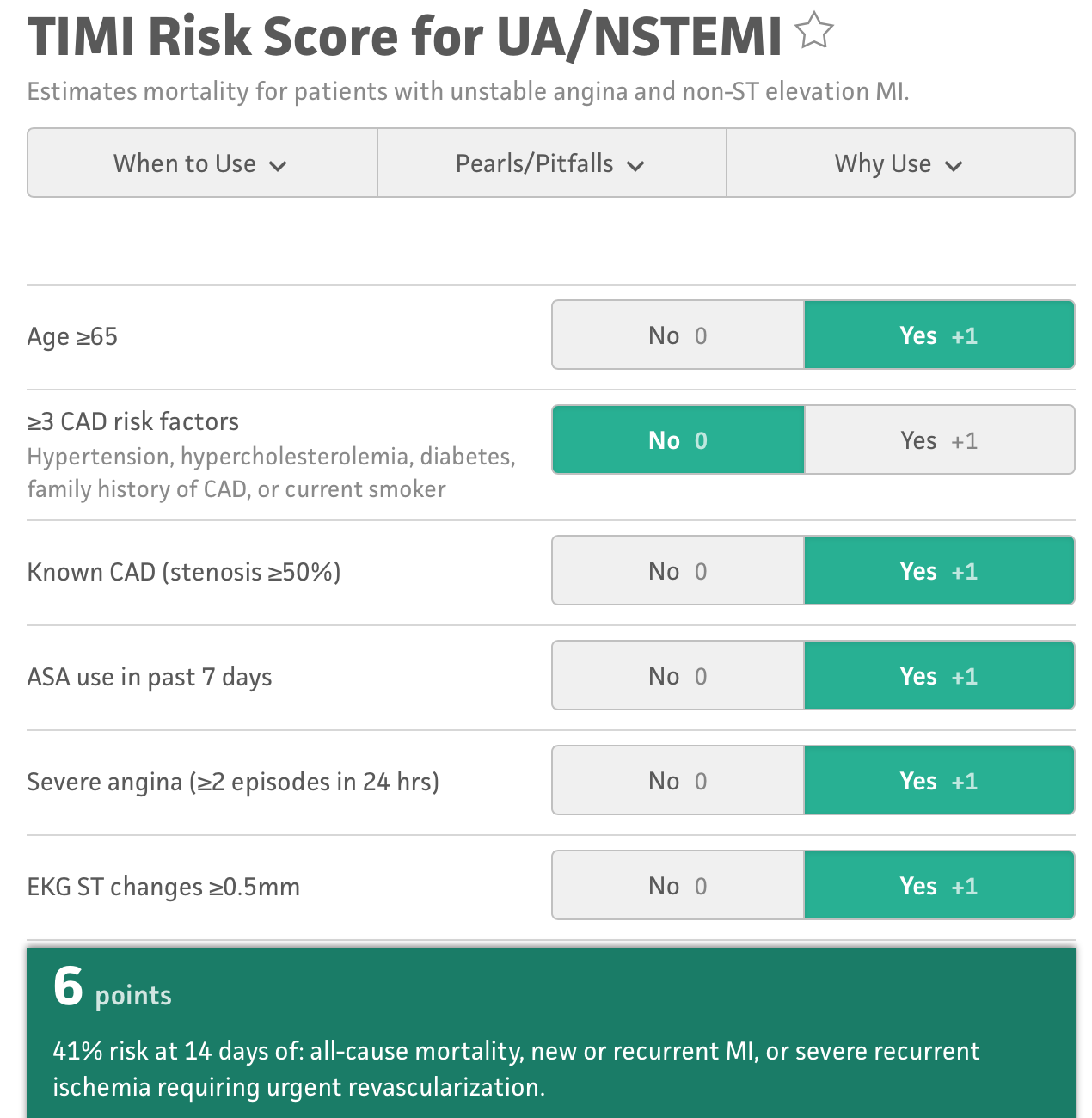
Male, 89 years old, presented to hospital with agina and black stool.History: hypertension and coronary disease, treated with aspirin 100mg/day.Esophageal gastroscopy: gastrointestinal hemorrhage Forrest IIb.The patient got positive medical treatment in 6 days, and the condition of gastrointestinal was stable.But during the time in hospital, the patient had typical aginaHemodynamic was stableTIMI Risk Score for UA/NSTEMI = 6
 -Relevant test results prior to catheterization:
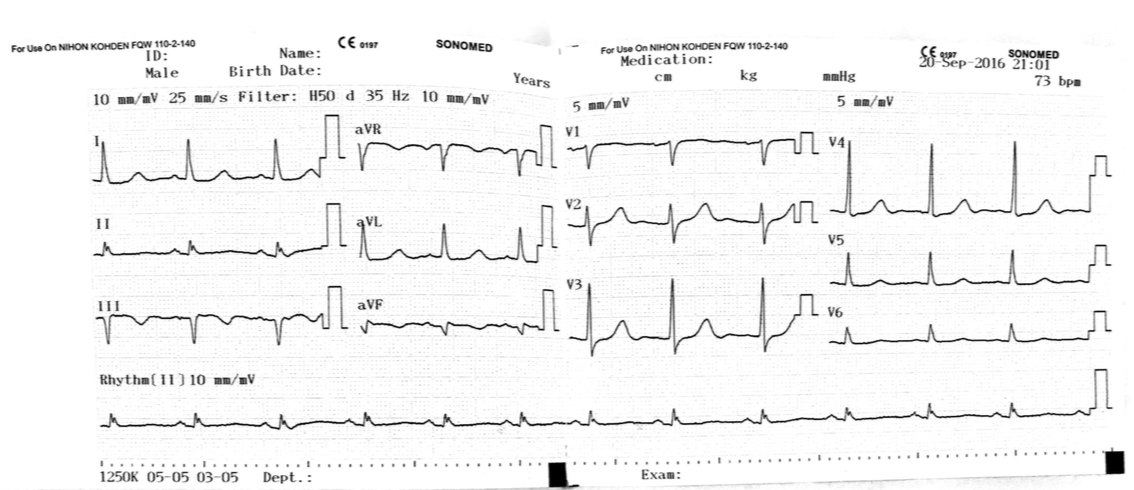
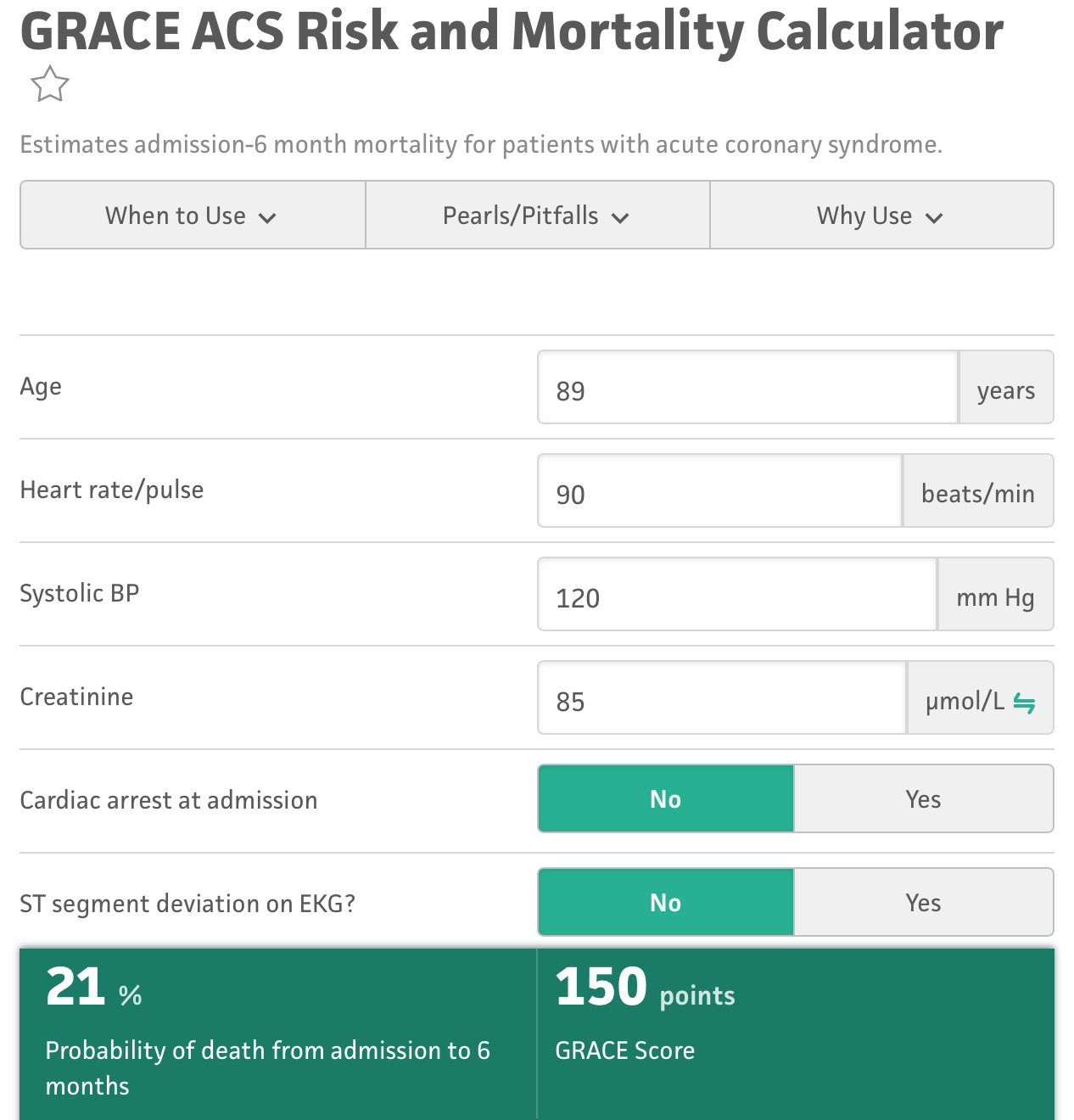
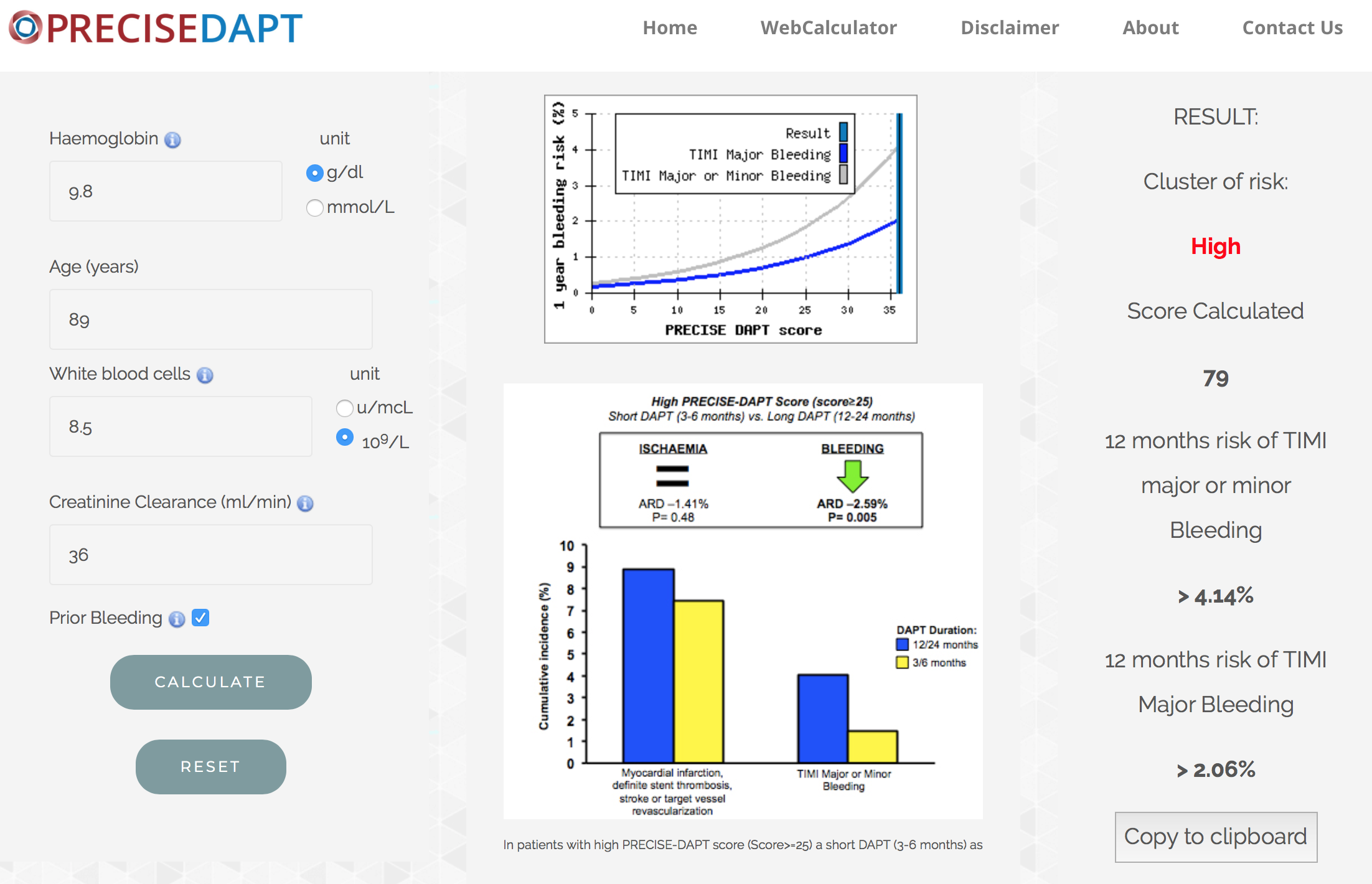
troponin T increased 250 ng/l --> 399 ng/l --> 504 ng/l. ECG: ST slighly raised in II, III, avF; echo showed that the posterior myocardial area decreased motion, EF 43%.Hb 98 G/LCreatinin 85 umol/l --> CrCl = 36 ml/minGRACE score = 150 pointsPRECISE DAPT score = 79 points
   - Relevant catheterization findings:
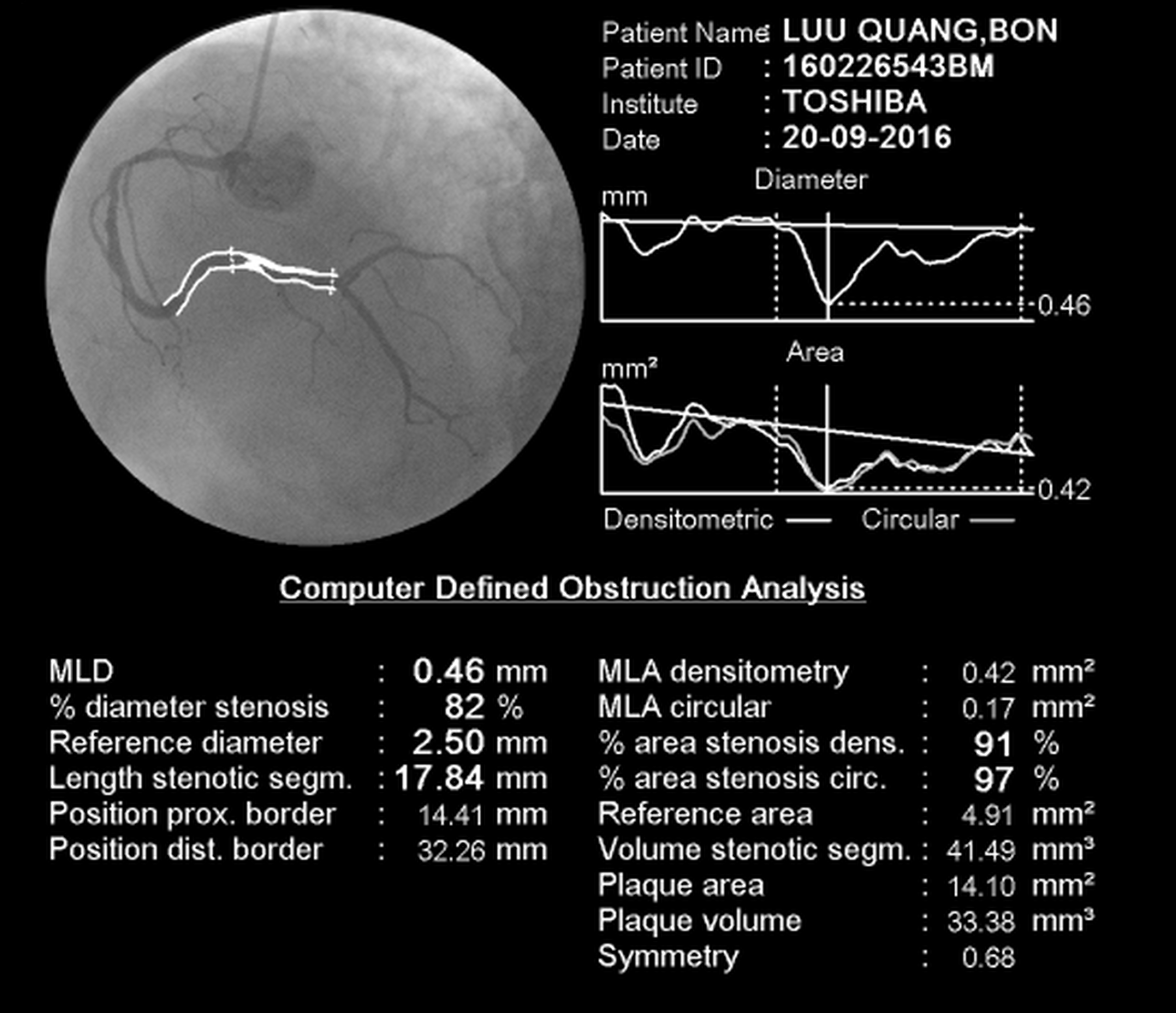
Angiography: lesion 90% RCA3, 70% LAD2 and CTO Lcx2, collateral circulation from LAD to Lcx.
 |
|
|
[Interventional Management]
- Procedural step:
We have three choices: 1- Stenting with DES and DAPT maybe used to 6-12mo Stenting with BMS and DAPT maybe used in 1 mo, after that use SAPT, but patient would accepted high risk of stent restenosis.2- Stenting with no-polymer drug-coat stent such as Biofreedom, DAPT maybe used in 1 mo, but risk of stent restenosis decreased.3-Medical treatment and no intervention.
We choosed 2 - using drug-coat stent BRF 2.75x33 for RCA3, Aspirin 81mg + Clopidogrel 75mg per day in one month after PCI. After that, we used Clopidogrel 75mg/day alone and take angiography after one year. The result was good, no re-stenosis, the patient was stable, no symptoms of bleeding, NYHA II, CCS I.He continued to use clopidogrel 75mg/day but three months later, he was diagnosised ulcer cancer. His family did not want to treat cancer because the patient was too old and he had been treated coronary disease with clopidogrel 75mg/day for 2 years and he died at 92 years old because of ulcer cancer. - Case Summary:
At least 20% of PCI patients are High bleeding risk (HBR), but in fact, mostly HBR patients excluded from device and APT trials, never specifically studied and current guideline recommendations: BMS + one month DAPT or DES + "shortened" DAPT.So No-polymer Drug-coated stent such as Biofreedom with advantages of both BMS and DES may be a good choice for High risk of bleeding patients undergoing PCI.
|
|