Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
CASE20190927_001
| IMAGING AND PHYSIOLOGIC LESION ASSESSMENT - Imaging: Intravascular | |
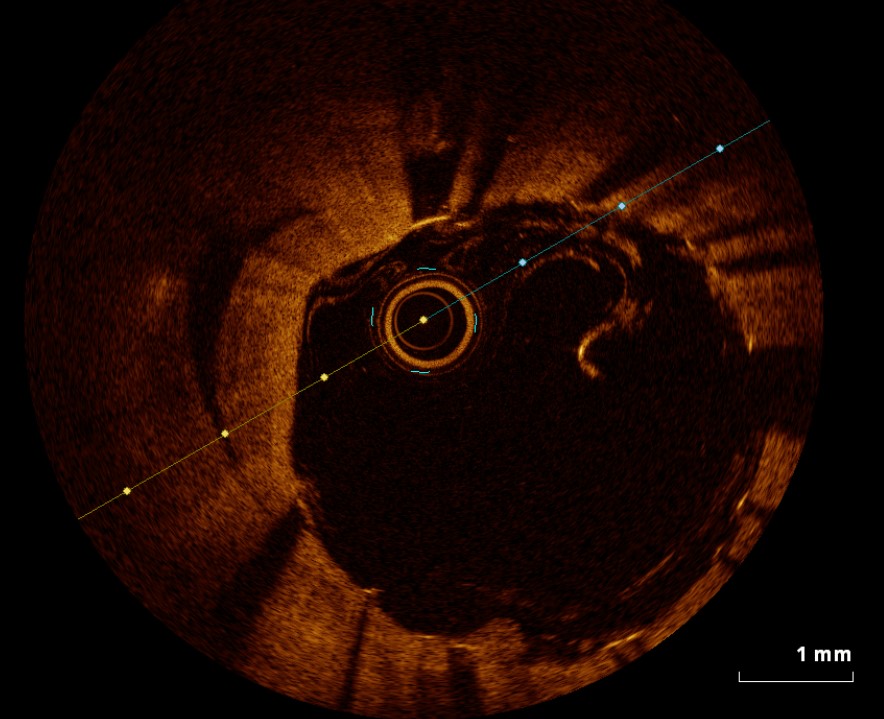
| An Amazing Optical Coherence Tomography Finding in Chronic Total Occlusion | |
| Ming-Shyan Lin1, Pochang Wang2 | |
| CGMH, Taiwan1, Chang Gung Memorial Hospital Chiayi, Taiwan2, | |
|
[Clinical Information]
- Patient initials or identifier number:
Mr. Li
-Relevant clinical history and physical exam:
The 47-year-old male teacher with dyslipidemia and hypertension presented to our clinic for intermittent effort tightness within recent 3 months. He denied habits of smoking or drinking. Physical examination was non-specific.
-Relevant test results prior to catheterization:
The echocardiography showed adequate LV systolic function (LVEF 67%) with hypokinesia at LAD territory, trivial MR, TR and AR. The ECG showed normal sinus rhythm with non-specific ST-T change. The treadmill reported positive of ischemic change during stage 3 exercise.
- Relevant catheterization findings:
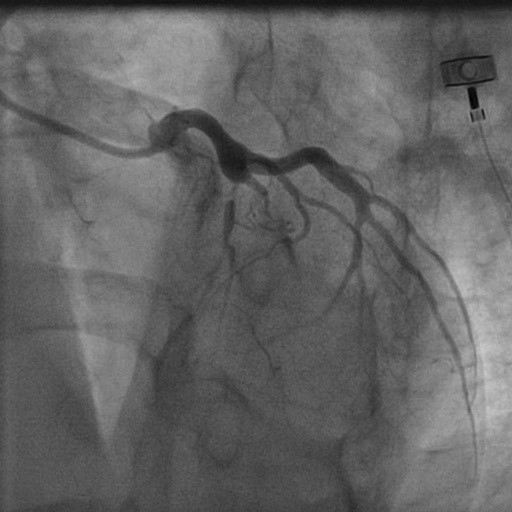
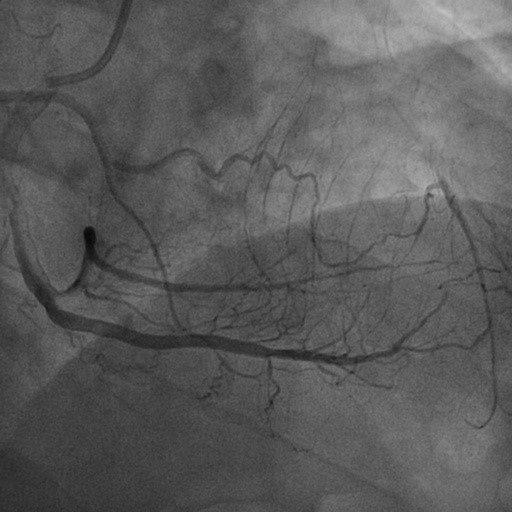
Coronary catheterization was scheduled on January 14, 2019. Beyond patency of left circumflex artery and right coronary artery, coronary angiography showed chronic total occlusion of proximal left anterior descending artery (since first septal branch) with collateral from right atrial branch (Rentrop grade 2).
  |
|
|
[Interventional Management]
- Procedural step:
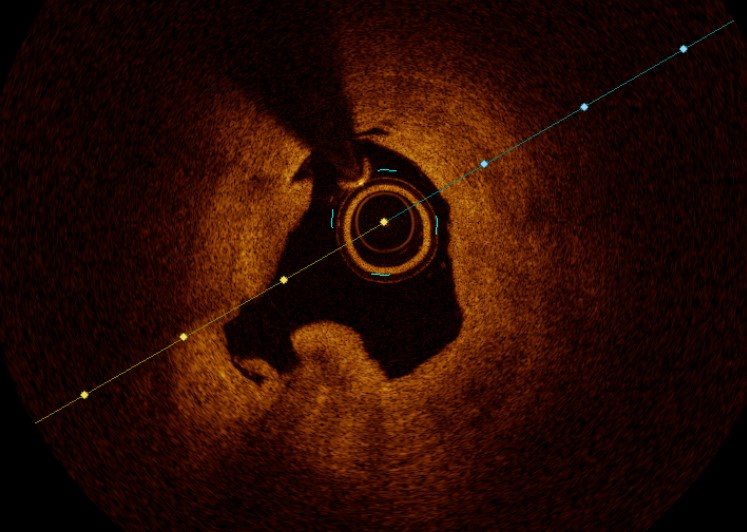
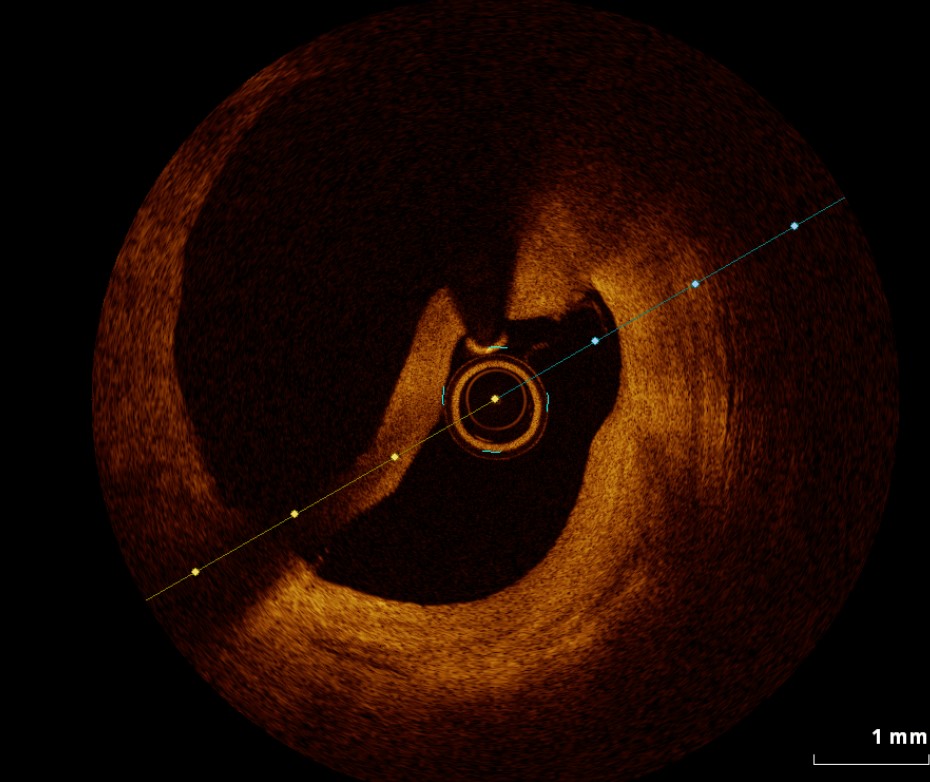
Initially, we attempted antegrade intervention for occluded LAD under 6F Medtronic EBU 3.5SH guiding catheter; however, the advance of wire (ASAHI Gaia second) failed to across the blunt entry stump. We tried retrograde re-wiring under Boston Excelsior MC support via tortuous RA branch to distal LAD, and then manipulated the Gaia second wire passing through the calcified cap into proximal LAD without Reverse CART technique. We completed externalization by an ASAHI RG3 wire, the first ballooning for critical CTO lesion, and put an antegrade wire into distal LAD smoothly. After POBA, the first 2.5*48mm DES was deployed at distal LAD and we performed OCT for lesion evaluation. OCT showed optimal apposition of the first stent over distal LAD and variable vessel size differences between p-CTO to proximal LAD (3.0 to more than 5.0 mm). In addition, one super huge dissection flap was swimming within proximal LAD and the working wire localized in true lumen. We considered significant vessel size variation and chose the second DES deploying between CTO to mid segment. We checked second OCT for stent expansion and chose the third stent according to proximal vessel size (> 5 mm), flap range and perfect stent length. As a result, we deployed a large sized DES to cover huge flap at ostial to proximal segment of LAD. Finally, we completed final OCT to check attachment of dissection flap and post PCI complications. The patient tolerated whole procedure and had absent angina until now.
   - Case Summary:
The problem of intervention for LAD chronic total occlusion with proximal huge dissection flap is to select adequate stent size. The OCT is a necessary to identify the vessel size of chronic total occlusion to ostial LAD, the origin of flap and optimizing of PCI with stenting.
|
|