Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
ABS20191115_0004
| Acute Coronary Syndromes (STEMI, NSTE-ACS) | |
| Determining the Efficacy of Different Double Antiplatelet Strategies Using Platelet Aggregometer in Patient Admitted with Acute Coronary Syndrome | |
| Muhamad Razi Zulkufli1, Shawal Faizal Mohamad2 | |
| MEDICAL, Malaysia1, Hospital Canselor Tuanku Muhriz UKM, Malaysia2 | |
|
Background:
Different Double Antiplatelet (DAPT) strategies among patient admitted with Acute Coronary Syndrome (ACS) and underwent Percutaneous Coronary Intervention (PCI) is a common practice in Universiti Kebangsaan Malaysia Medical Centre (UKMMC). However, its efficacy in term of incidence of high on-treatment platelet reactivity (HPR) is still not clear. The aim of this study is to observe and determine the efficacy of 3 different DAPT strategies practiced in UKMMC for patients admitted for ACS and underwent PCI by measuring the HPR. We also evaluate the clinical major adverse cardiovascular events (MACEs) and safety of each DAPT strategies.
|
|
|
Methods:
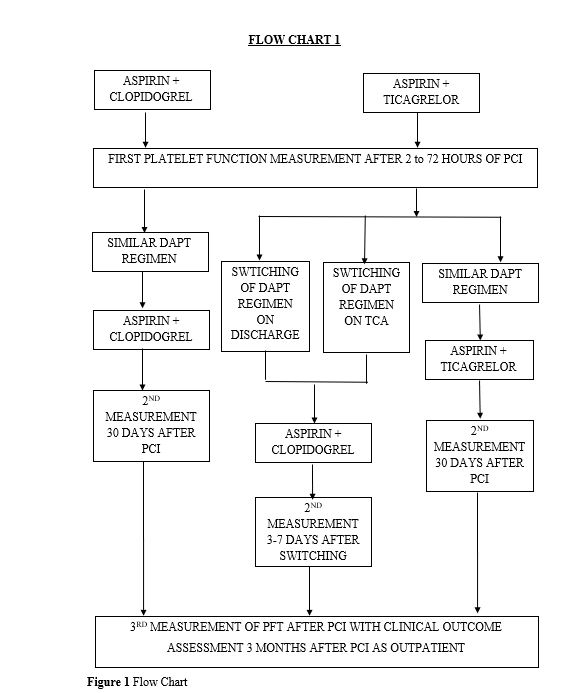
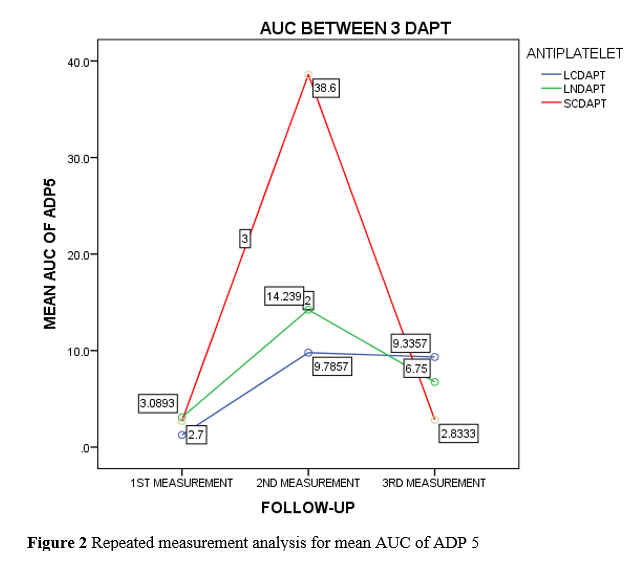
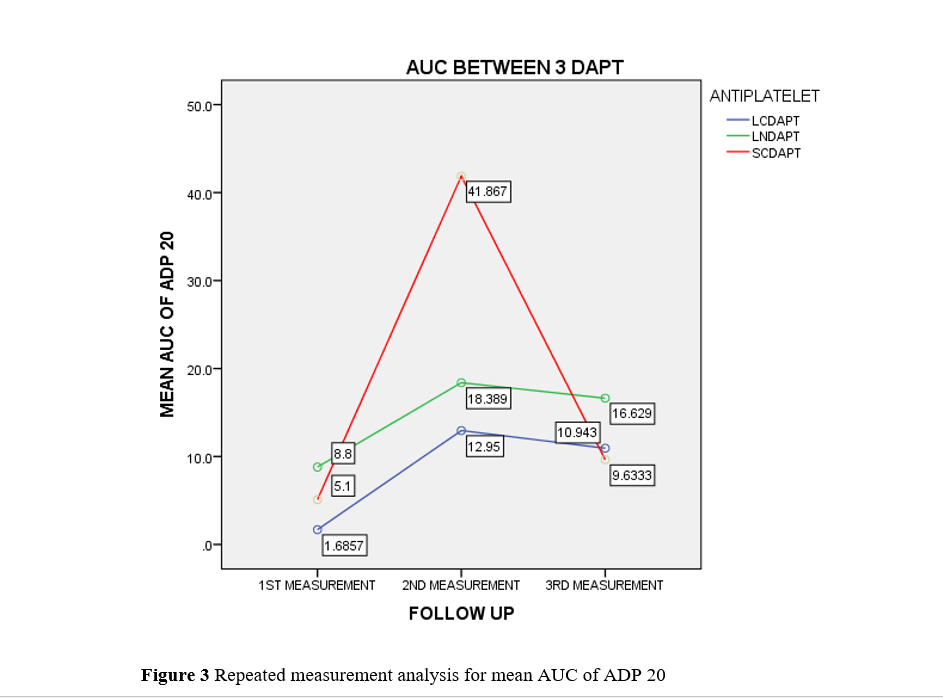
This was an observational study which recruited patients admitted to UKMMC for ACS and underwent PCI from March 2019 to September 2019. We observed 3 different DAPT strategies, longterm conventional DAPT, i.e Aspirin plus Clopidogrel, long term new DAPT, i.e Aspirin plus Ticagrelor and Short term new DAPT, i.e Aspirin plus Ticagrelor then switch to Aspirin plus Clopidogrel. We measured the area under the curve (AUC) of HPR to ADP on 3 different period of time using the Light Transmission Aggregometry (LTA) (ChronoPar). We examined adverse cardiovascular events (MACEs), re-admission for ACS, Stent Thrombosis (ST) or In-stent Re-stenosis (ISR) and also incidence of thrombolysis in myocardial infarction(TIMI) bleeding. Repeated measurement analysis was used to detect changes of platelet aggregation on each occasion.
 |
|
|
Results:
A total of 50patients were recruited and their mean age was 57.92 ¡¾ 11.4 years. Majority of the patients recruited were Chinese (44%, n=22), followed by Malay (42%, n=21). About 80%, n=40 patients were male. The main type of ACS was STEMI (60%, n=30) with common type of lesion was PCI to LAD (66%, n=33). Delayed PCI or Pharmaco-invasive strategy was the main type of PCI done (40%, n=20). We observed 3 different DAPT strategies, Long term conventional DAPT (LCDAPT);30%, n=15, Long term new DAPT (LNDAPT);58%, n=29 and Short term new DAPT (SNDAPT)(12%, n=6). The switching of Ticagrelor to Clopidogrel within 3 months were infrequent and the overall incidence HPR was only 12%, n=6 throughout the study period with no significant outcome of MACEs or bleeding. However, analysis for SNDAPT group, there were 3 (50%) of 6 patients (p<0.001) who were switched from Ticagrelor to Clopidogrel were documented to have HPR on 2nd measurement of blood samples. 2(33.3%) of 6 patients (p<0.047) were admitted for recurrent ACS (USA) after switching was made. Both of them developed incidence of HPR after early switching (7 days post PCI). This outcome was significantly correlate with the incidence of HPR after early switching from Ticagrelor to Clopidogrel with p value of 0.005.
  |
|
|
Conclusion:
The analysis found that difference DAPT strategies were infrequent practice in UKMMC during first 3 months after PCI and did not result in overall increase in significant outcome of MACEs or bleeding. However, specific group SNDAPT which switched from Ticagrelor to Clopidogrel at day 7 post PCI did result in increased incidence of HPR and recurrent admission for ACS.
|
|