Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
ABS20191114_0007
| Gender Difference in Long-term Clinical Outcomes After Percutaneous Coronary Intervention - A Propensity-matched Analysis of National Health Insurance Data in the Republic of Korea | |
| Seunghwa Lee1, Eun-Seok Shin2, Jin Ho Choi3, Joo Myung Lee3, Taek Kyu Park3, Jeong Hoon Yang3, Young Bin Song3, Joo-Yong Hahn3, Seung Hyuk Choi3, Hyeon-Cheol Gwon3, Sang Hoon Lee3 | |
| Wiltse Memorial Hospital, Korea (Republic of)1, Ulsan University Hospital, Korea (Republic of)2, Samsung Medical Center, Korea (Republic of)3 | |
|
Background:
Despite the advances in the interventional technology, devices, and pharmacotherapy which have translated into better clinical outcome of patients undergoing percutaneous coronary intervention (PCI), there is still a disparity in the clinical outcome between women and men undergoing PCI.
|
|
|
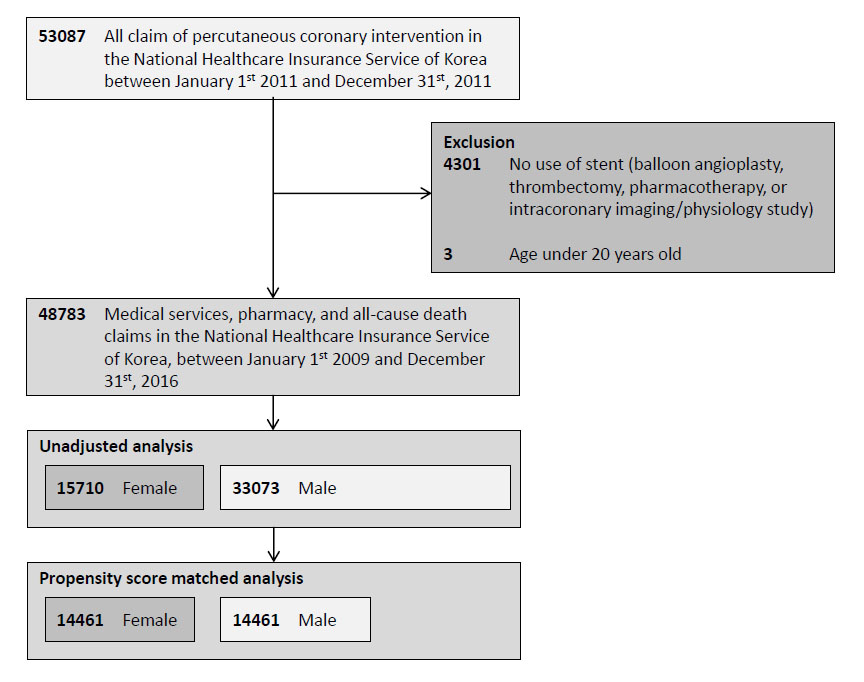
Methods:
We retrospectively enrolled a nationwide cohort of all Korean PCI performed in year 2011. Primary outcome was 5-year cumulative incidence of major adverse clinical event (MACE) consisting of all-cause death, revascularization, critically ill cardiovascular status, or stroke. Outcomes adjusted with age and propensity for clinical characteristics were additionally compared.
 |
|
|
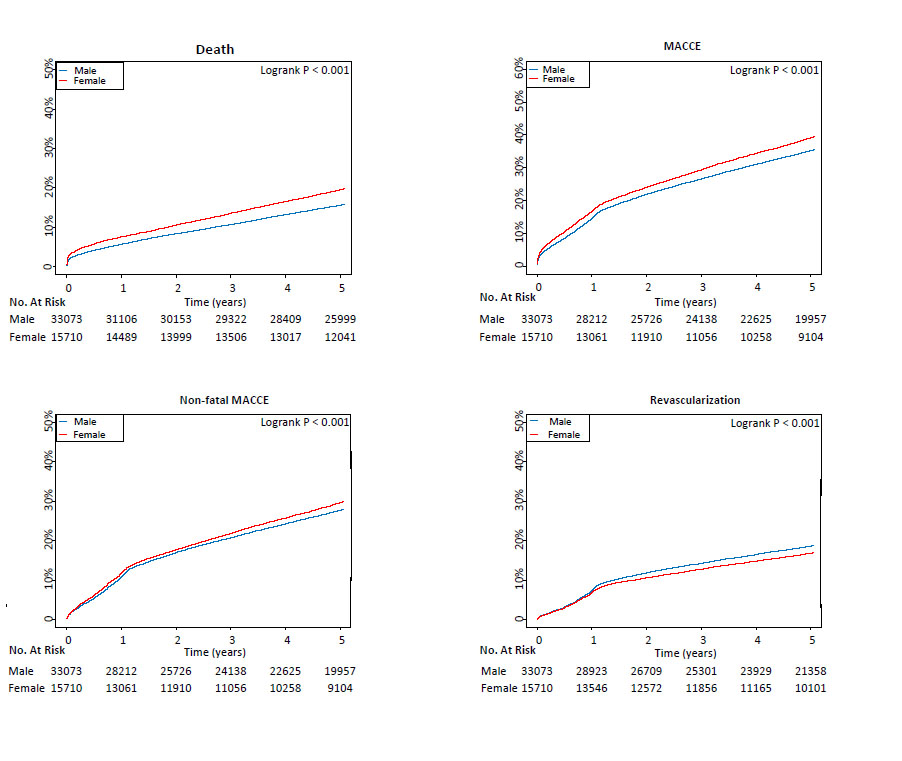
Results:
In unadjusted analysis, female (N=15710) were older (69.7¡¾9.7 versus 62.0¡¾11.1year, p<0.001) and had higher frequency of comorbidities including hypertension, hyperlipidemia, and diabetes compared to male (N=33073) (p<0.001, all). female had higher 5-yearcumulative incidence of MACE than men (21.8% versus 17.3%; hazard ratio [HR] 1.29, 95% confidential interval [CI] 1.23 ? 1.34; p<0.001). However, in the analysis of age and propensity score-matched 14461 pairs, women had lower 5-year mortality risk (20.3% versus 26.1%, HR 0.85, 95% CI 0.82-0.88, p<0.001). This finding was consistent in subgroup analyses of age, risk factors, and clinical presentation such as acute myocardial infarction or stable angina (p<0.05, all).
  |
|
|
Conclusion:
The apparent worse outcome in women can be explained by older age and more common comorbidities in women. After adjusting these disadvantages, women had better outcome after PCI than men.
|
|