Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
ABS20191101_0009
| Valvular Intervention: Aortic | |
| Clinical Predictors and Impact of Leaflet Thrombosis Following TAVI with 320-Multislice CT at Medium Term Follow-Up | |
| Hashrul Rashid1, Nancy Khav2, Sean Tan2, Arthur Nasis3, James Cameron3, Rob Gooley3 | |
| Monash University, Australia1, Monash Health and Monash University, Australia2, MonashHeart and Victorian Heart Institute, Australia3 | |
|
Background:
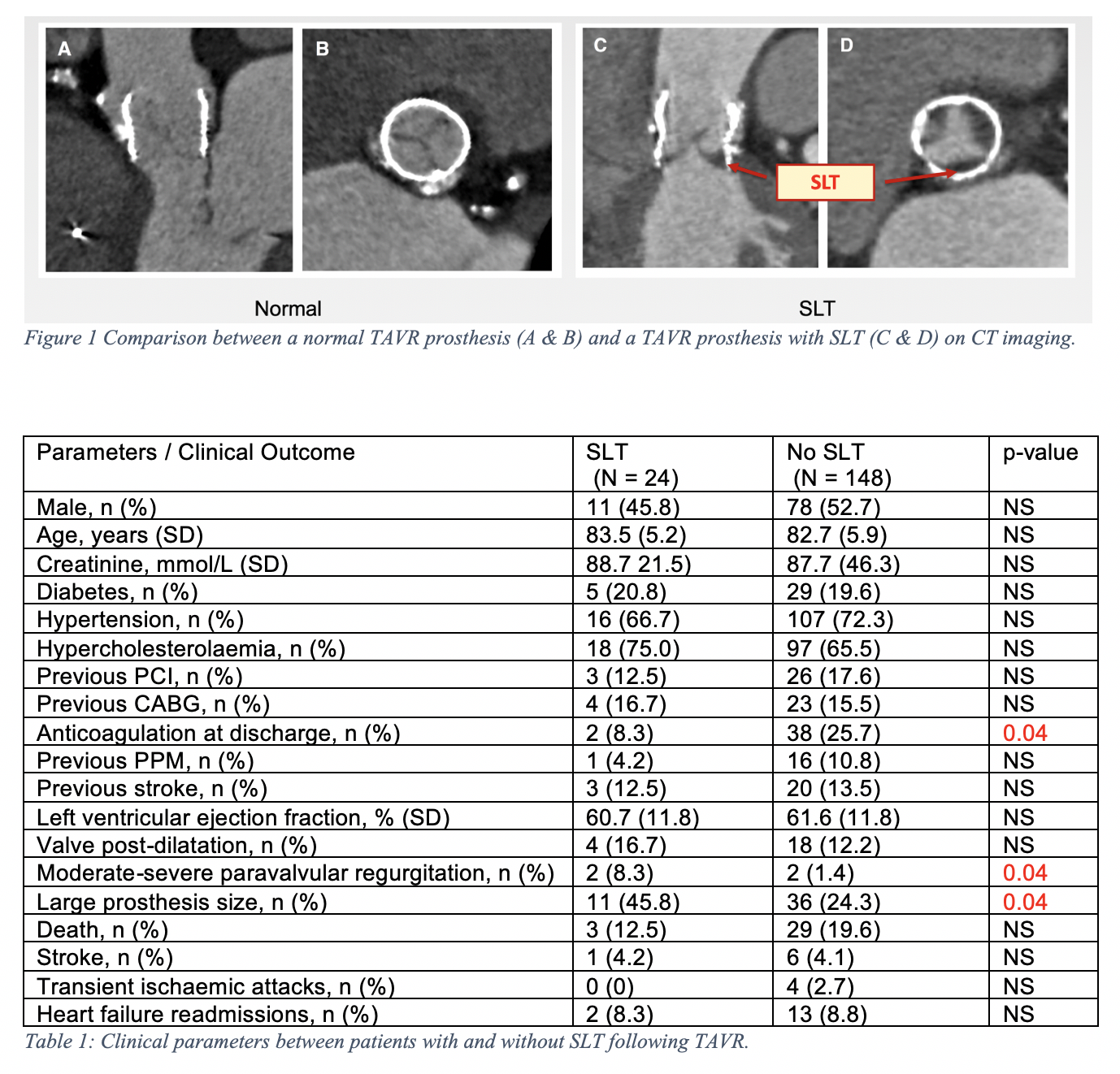
Computed tomography (CT) defined subclinical leaflet thrombosis (SLT) following transcatheter aortic valve implantation (TAVI) has recently been described. There is limited data on this condition.
|
|
|
Methods:
Patients were evaluated prospectively with CT following TAVI. All examinations were performed with a 320-multislice CT (Aquilion One, Canon) with ECG-gated acquisition. Images were assessed on a dedicated workstation (3Mensio, Pie Medical Imaging) with multiplanar reconstruction for presence of SLT, defined as hypo-attenuating leaflet thickening. No patients had clinical leaflet thrombosis (overt heart failure with high prosthesis gradients).
|
|
|
Results:
172 patients [89 (51.7%) male, mean age 82.8¡¾5.7 years, STS score 5.1¡¾2.1%] were included in this analysis [Lotus valve 54%, Core valve 32% and Sapien valve 14%], with median CT-scan of 6 weeks post TAVI. Characteristics and potential associates of SLT are shown in the table. The overall prevalence of SLT was 14% (24 cases) with a trend towards lower rates of SLT with Core valve (7.3%), in comparison to Lotus (17.2%) and Sapien valves (16.7%) (p = 0.07). Patients who developed SLT were less likely to be on anticoagulation at discharge (8.3% vs 25.7%, p = 0.04), received larger TAVI prostheses (45.8% vs 24.3%, p = 0.04) and higher rates of moderate-severe paravalvular regurgitation (PVR) with SLT (8.3% vs 1.4%, p = 0.04). There no difference in the rates of death, stroke or transient ischemic attacks at median follow-up of 2 years.
 |
|
|
Conclusion:
Absence of anticoagulation, large TAVI prosthesis and moderate-severe PVR were predictors of SLT. There was a trend towards lower rates of SLT with Core valve. SLT did not lead to increased adverse outcome. Further studies are warranted to determine the long-term impact of SLT following TAVI.
|
|