Lots of interesting abstracts and cases were submitted for TCTAP & AP VALVES 2020 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don¡¯t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
* The E-Science Station is well-optimized for PC.
We highly recommend you use a desktop computer or laptop to browse E-posters.
ABS20191007_0002
| Acute Coronary Syndromes (STEMI, NSTE-ACS) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Long-Term Outcomes of Single-Vessel Percutaneous Coronary Intervention on Culprit Vessel Versus Multivessel Percutaneous Coronary Intervention in Non-ST-Segment Elevation Acute Coronary Syndrome Patients with Multivessel Coronary Artery Disease | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Tianyu Li1, Sida Jia1, Yue Liu1, Yi Yao1, Ying Song1, Xiaofang Tang1, Xueyan Zhao1, Runlin Gao1, Yuejin Yang1, Bo Xu1, Zhan Gao1, Jinqing Yuan1 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Fuwai Hospital, China1 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Background:
A lack of clarity exists regarding the optimal percutaneous coronary intervention (PCI) strategy in non-ST-segment elevation acute coronary syndrome (NSTE-ACS) patients with multivessel coronary artery disease (MV-CAD). We aimed to compare long-term prognosis between multivessel PCI (MV-PCI) and single-vessel PCI on culprit vessel (SV-PCI) in patients with MV-CAD presenting with NSTE-ACS.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Methods:
Patients with MV-CAD presenting with NSTE-ACS undergoing PCI in Fuwai Hospital in 2013 were prospectively enrolled. SV-PCI was defined as targeting only the culprit vessel, while MV-PCI was defined as treating ¡Ã 1 coronary artery(s) in addition to the culprit vessel at the index procedure. The primary endpoint was the incidence of major adverse cardiovascular and cerebrovascular events (MACCE), consisting of all-cause death, cardiac death, myocardial infarction, unplanned revascularization, or stroke at 2 years.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Results:
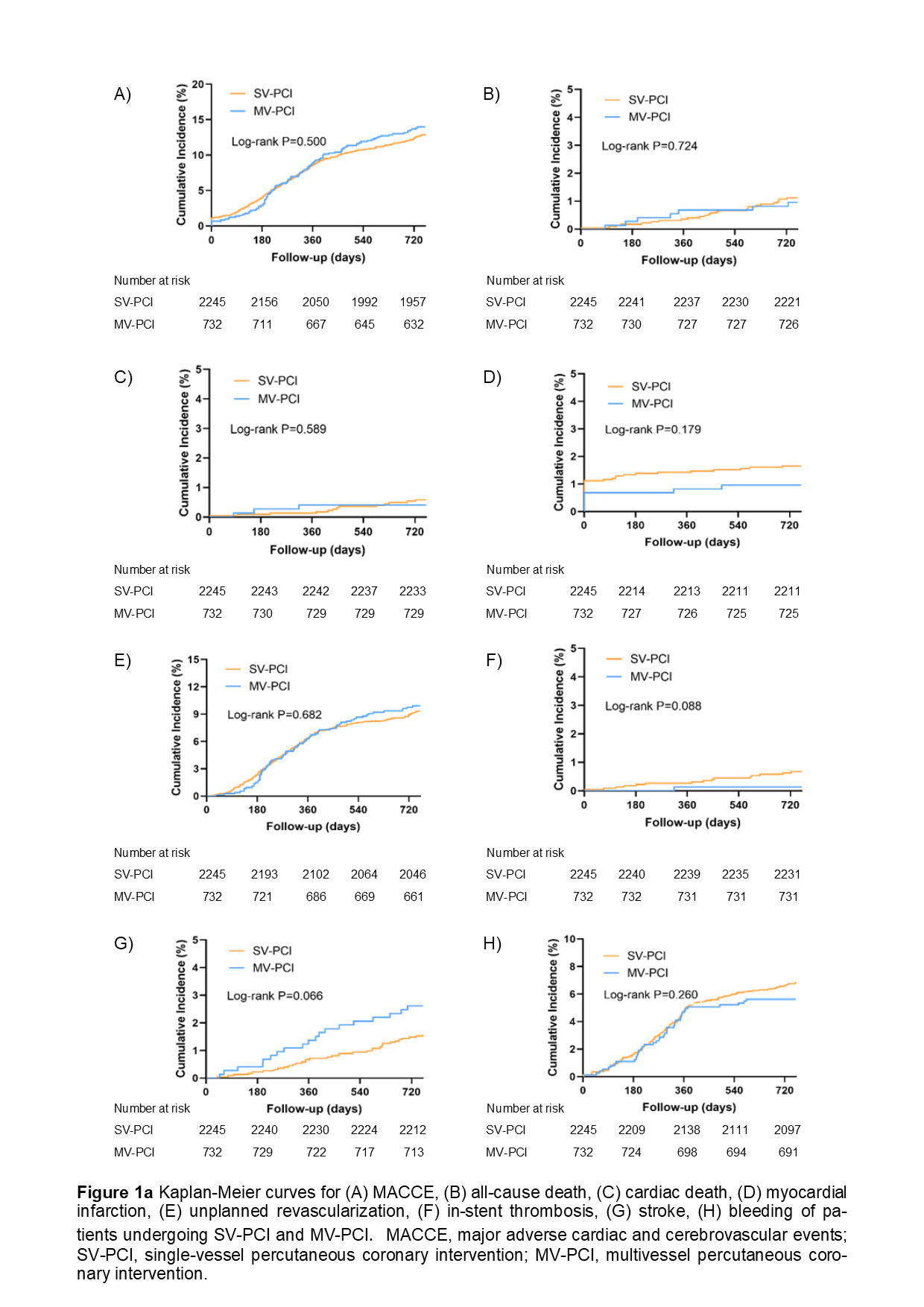
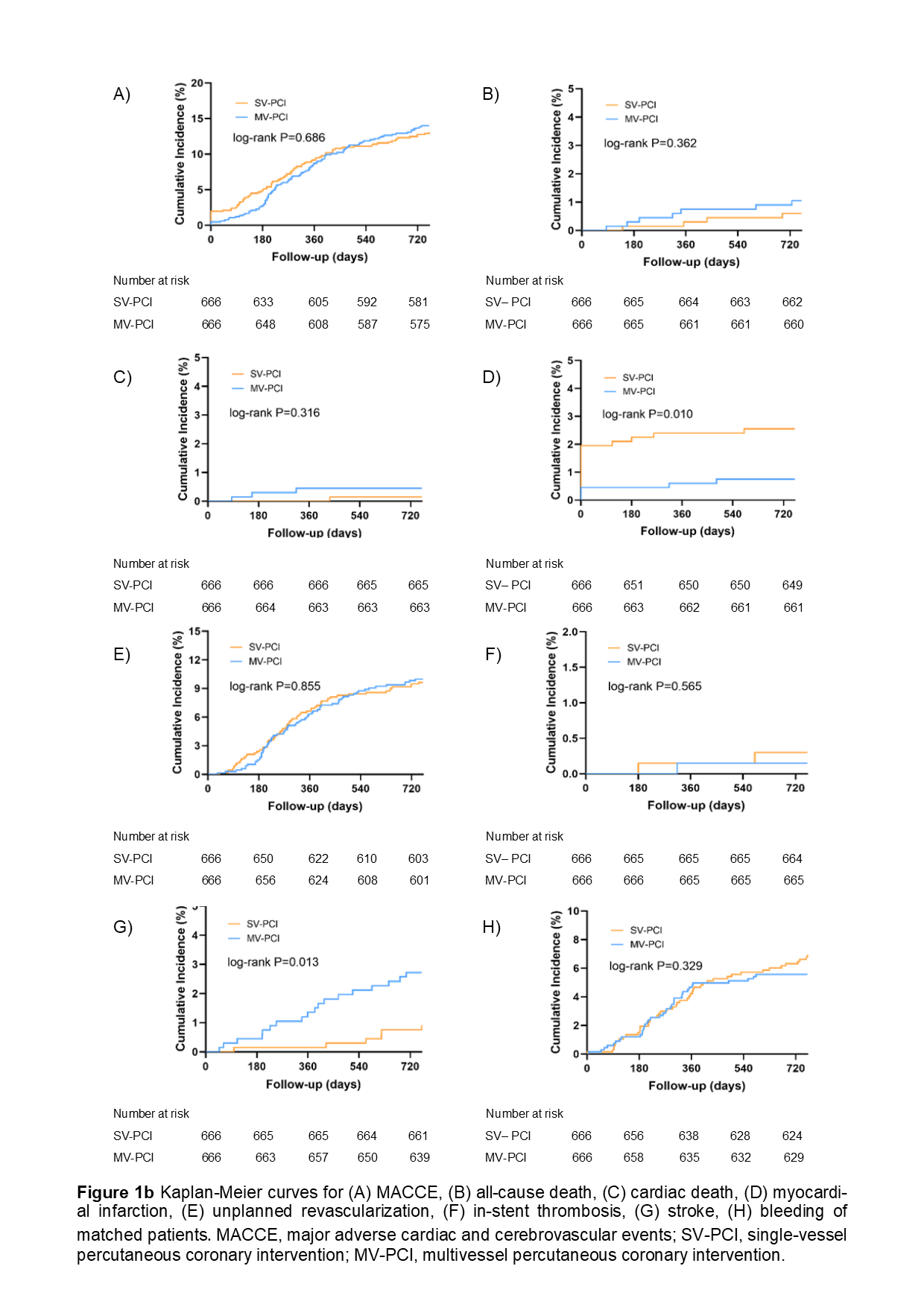
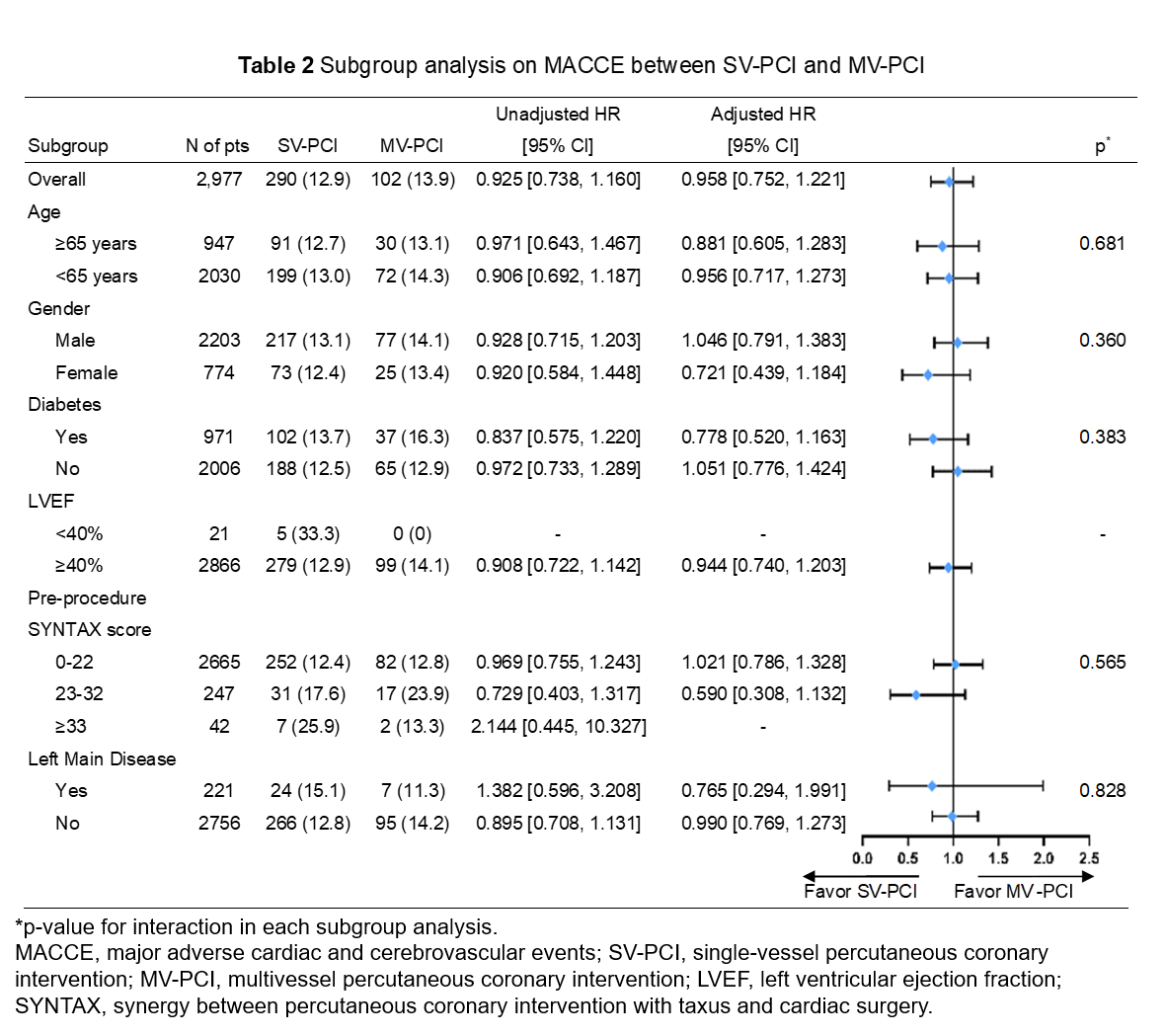
A total of 2,977 patients were included in our study. SV-PCI and MV-PCI were performed in 2,245 patients (75.4%) and 732 patients (24.6%), respectively. During a median follow-up of 2.1 years, the MACCE rates and adjusted risk were not significantly different between the SV-PCI and MV-PCI group (12.9% vs. 13.9%, p = 0.480; adjusted HR = 0.958, 95% CI: 0.752 - 1.221) . Similar results were observed in propensity-matched patients (13.1% vs. 14.0%, p = 0.631; adjusted HR = 0.945; 95% CI: 0.689 - 1.298). Subgroup analysis revealed a consistent effect on 2-year MACCE across different subgroups.
Table 1 Cox Regression analysis of SV-PCI/MV-PCI on 2-year clinical outcomes
   |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Conclusion:
In NSTE-ACS patients with MV-CAD, MV-PCI is not superior to SV-PCI in terms of long-term MACCE. Further randomized control trials are required to guide practice.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||