
Tullio Palmerini
University of Bologna, Italy
At TCTAP 2025, during the Ī░TAVR: Current Status and Future PerspectiveĪ▒ session held on April 26 in the Coronary Theater, Dr. Tullio Palmerini (University of Bologna, Italy) delivered a comprehensive overview of the current landscape and persistent challenges in valve-in-valve (ViV) transcatheter aortic valve replacement (TAVR). As the use of bioprosthetic surgical valves continues to rise, so does the clinical relevance of ViV procedures for structural valve deterioration. However, multiple procedural and anatomical hurdles remain, limiting its universal applicability and long-term outcomes.
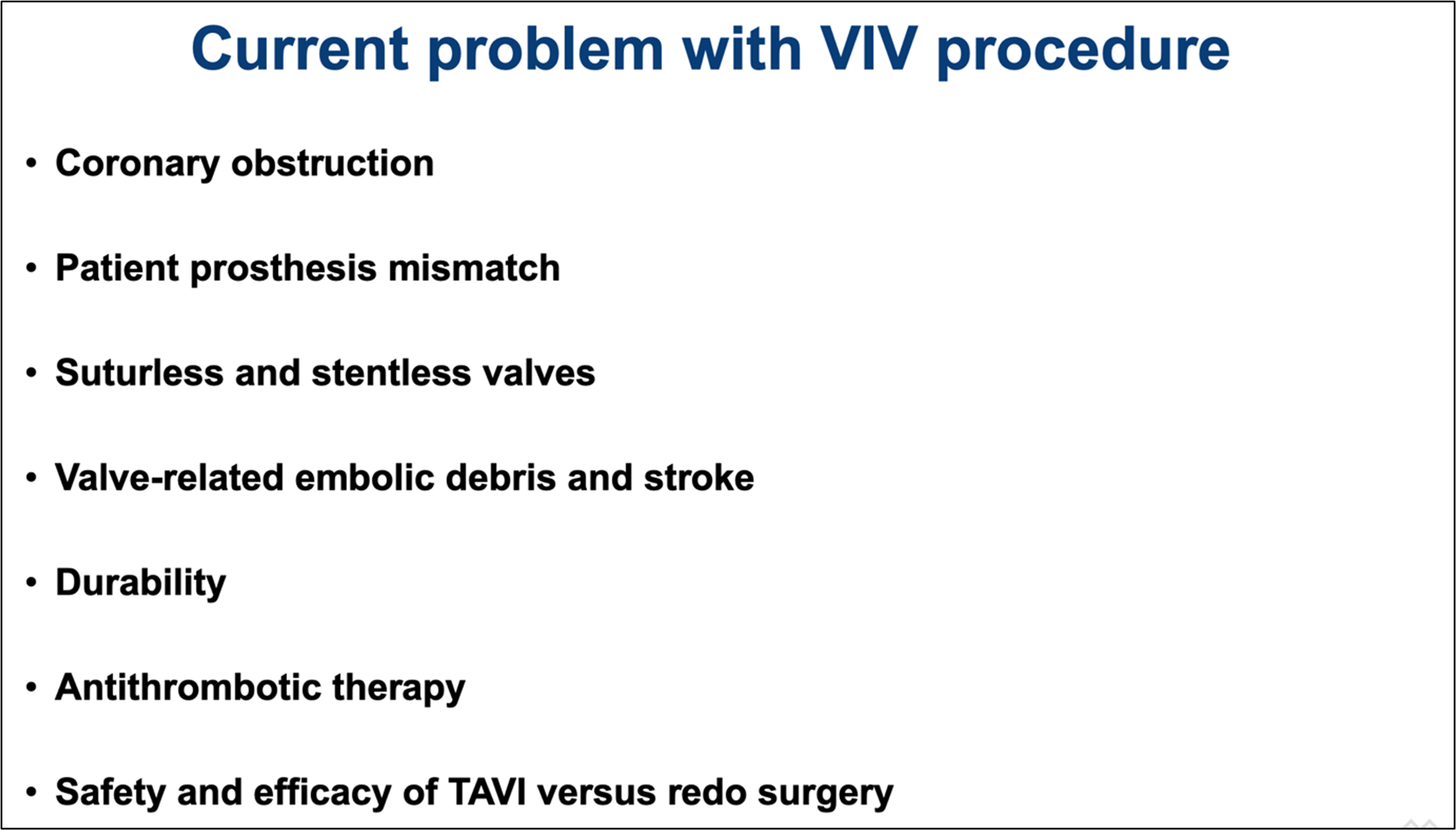
Dr. Palmerini began by outlining the major complications associated with ViV, including coronary obstruction, patient–prosthesis mismatch (PPM), and anatomical difficulties associated with sutureless or stentless valves. He also highlighted concerns regarding valve-related embolic debris, durability, optimal antithrombotic therapy, and the comparative safety and efficacy of TAVR versus redo surgery (Figure 1).
Among these, coronary obstruction remains one of the most feared complications, particularly due to sinus sequestration or leaflet displacement toward the coronary ostia. Dr. Palmerini detailed protective strategies such as CHIMNEY stenting, BASILICA, and emphasized that newer technologies like the short cut device may offer more reliable protection in the future—personally stating he finds it especially promising.
Another major focus was on patient–prosthesis mismatch, which affects over half of ViV patients according to STS and TVT registry data. Dr. Palmerini stressed the value of bioprosthetic valve fracture (BVF) as a key technique for the successful procedure. He devoted significant time to describing the mechanics, timing, and safety profile of BVF, citing both registry data and multicenter experiences. Importantly, delayed BVF—performed after valve implantation—was associated with lower residual gradients and better hemodynamic outcomes.
Issues surrounding sutureless and stentless valves were also addressed, particularly the anatomical ambiguity they present in identifying landing zones and achieving adequate anchoring. These factors contribute to higher procedural failure rates, as noted in the VIVID registry.
In conclusion, Dr. Palmerini emphasized that while ViV TAVR is generally safe and effective, procedure planning, device selection, and operator technique are crucial to optimizing outcomes. He called for randomized controlled trials, especially in intermediate-risk patients aged 70–80 years, to better define long-term strategies for ViV management.
TAVR: Current Status and Future Perspective
Saturday, April 26, 9:50 AM-11:20 AM
Coronary Theater, Level 1
Edited by

Osung Kwon, MD
The Catholic University of Korea Eunpyeong St. Mary's Hospital, Korea (Republic of)
