Jung-Kyu Han
Seoul National University Hospital, Korea (Republic of)
Chronic total occlusion percutaneous coronary intervention (CTO PCI) remains one of interventional cardiology's most technically challenging procedures. Despite advancements in crossing devices, microcatheters, and guidewires, initial procedural failure rates range from 10-40%, depending on operator experience and lesion complexity. However, evidence suggests that a carefully planned second attempt can achieve successful revascularization in approximately 50-70% of previously failed cases when appropriate patient selection, optimal timing, and technical modifications are implemented.
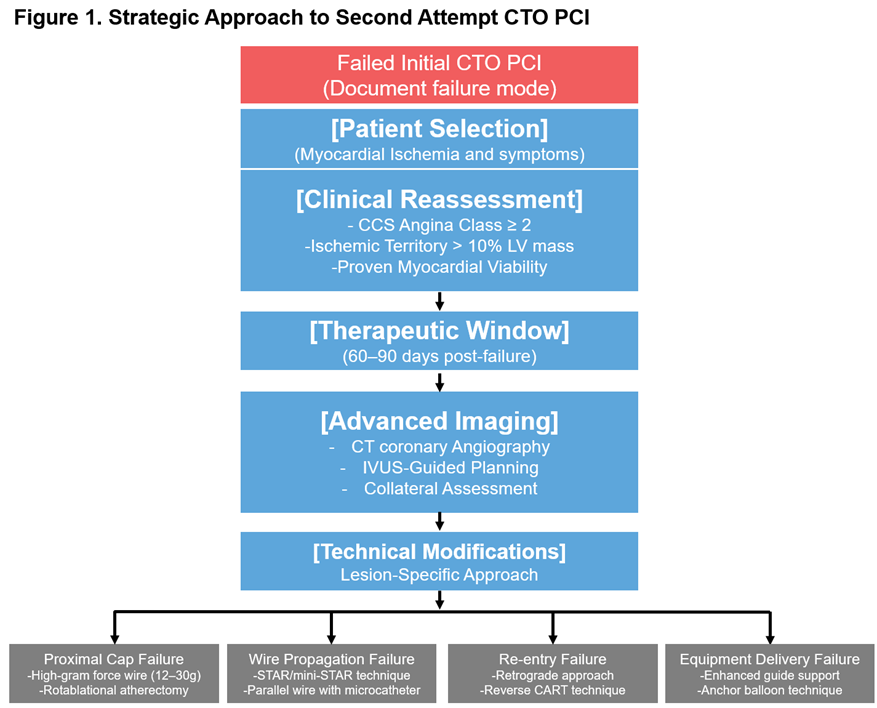
Patient Selection: Evidence-Based Clinical Criteria
Selecting patients for reattempted CTO PCI requires objective measures of myocardial ischemia and symptoms. Optimal candidates include those with Canadian Cardiovascular Society (CCS) angina class Ī├2 despite optimal medical therapy. On stress imaging, patients should also have objective evidence of myocardial ischemia (>10% of left ventricular mass). In addition, myocardial viability should be confirmed by cardiac MRI, PET, or dobutamine echocardiography. The best candidates have occlusions in prognostically significant territories, such as the proximal LAD, large dominant RCA, or last remaining patent vessel.
Retrospective analyses have shown that successful CTO revascularization in these patients significantly improved angina symptoms (Seattle Angina Questionnaire scores) and reduced major adverse cardiac events (MACE) at 12-24 months.
Therapeutic Window: Pathophysiological Considerations
The optimal timing for a second attempt is within 60-90 days after the initial failure. This interval allows for the resolution of procedure-induced vascular inflammation (7-14 days), remodeling of dissection planes from initial wiring attempts (30-45 days), and stabilization of plaque architecture before excessive fibrotic reorganization (>90 days).
A study by Zhong et al. (JACC Intv. 2022) demonstrated that reattempted procedures performed within the optimal therapeutic window of 60-90 days achieved a significantly higher success rate with an odds ratio of 0.85 per 90 day increment (95% CI: 0.73-0.98).
Advanced Imaging
CT coronary angiography with dedicated CTO protocols can provide critical information on the three-dimensional course of the occluded segment, calcium burden quantification, side branch anatomy at the proximal and distal caps, and the size and quality of potential collateral channels.
Intravascular ultrasound (IVUS) guidance significantly enhances procedural success during reattempts. This includes precise identification of proximal cap microanatomy (e.g., calcium arc thickness), confirmation of true lumen versus subintimal wire position, guided re-entry from subintimal space to true lumen, and optimization of stent sizing and expansion.
Technical Modifications: Lesion-Specific Approach
The procedural strategy for a second attempt should be tailored based on the failure mode encountered during the initial attempt. For proximal cap penetration failures, advancement to higher gram-force wires (12-30 g), rotational atherectomy for calcified caps, and "scratch-and-go" techniques with stiff guidewires or dedicated CTO devices are recommended.
In cases of wire propagation failures, implementation of advanced algorithms such as STAR, mini-STAR, or LAST technique, along with parallel wire technique using microcatheters to optimize wire position, can be beneficial.
For distal cap re-entry failures, retrograde approaches via septal or epicardial collaterals for complex lesions (J-CTO score Ī├3), reverse CART technique with appropriately sized balloons, and use of dedicated re-entry devices like the StingrayóŌ system for challenging anatomies are appropriate strategies.
When equipment delivery failure occurs, enhanced guide catheter support techniques and anchor balloon techniques can improve device delivery.
Complication Avoidance Strategies
Second-attempt CTO PCI must incorporate enhanced safety protocols to minimize complications. These include radiation dose minimization techniques (15 frames/second fluoroscopy, collimation), stage-wise contrast volume limitations (<3.7Ī┐ creatinine clearance in mL), dual access with contralateral injections for maintained visualization during retrograde approaches, and hemodynamic support consideration (e.g., Impellaóń or IABP) for high-risk anatomy.
Comprehensive Outlook
Reattempting a previously failed CTO PCI calls for comprehensive lesion-specific planning, optimal timing within the validated 60–90-day therapeutic window and integrating advanced imaging modalities. Multiple registries indicate that technical modifications guided by initial failure analyses can result in successful revascularization for previously failed cases, with reported reattempt success rates ranging from 71.2% to 86.7% across various studies.
This substantial improvement over initial attempt failure rates justifies the additional resource utilization when patients are selected appropriately. Those who derive the greatest benefit include individuals with significant myocardial ischemia (>10%), persistent angina symptoms despite optimal medical therapy, and preserved viability in the target vessel territory.
As dedicated CTO equipment continues to evolve, hybrid algorithms are refined, and operator expertise grows in specialized CTO centers, outcomes for this challenging subset of coronary interventions are expected to improve further. Prospective randomized trials evaluating staged hybrid approaches and novel crossing technologies will be essential to establish definitive, evidence-based protocols for reattempted CTO interventions.
CTO PCI Technical Forum: Learn From Masters
Friday, April 25, 3:10 PM-4:40 PM
Presentation Room 1, Level 1
Edited by
Taeoh Kim, MD
Asan Medical Center, Korea (Republic of)

