
Roxana Mehran
Icahn School of Medicine at Mount Sinai, USA
As the recipient of the 15th TCTAP Master of the Masters Award, Roxana Mehran, MD (Icahn School of Medicine at Mount Sinai, USA), delivered a message on the transformative future of interventional cardiology—one defined not only by technical excellence in the cath lab but also by long-term, personalized prevention and cross-disciplinary collaboration.
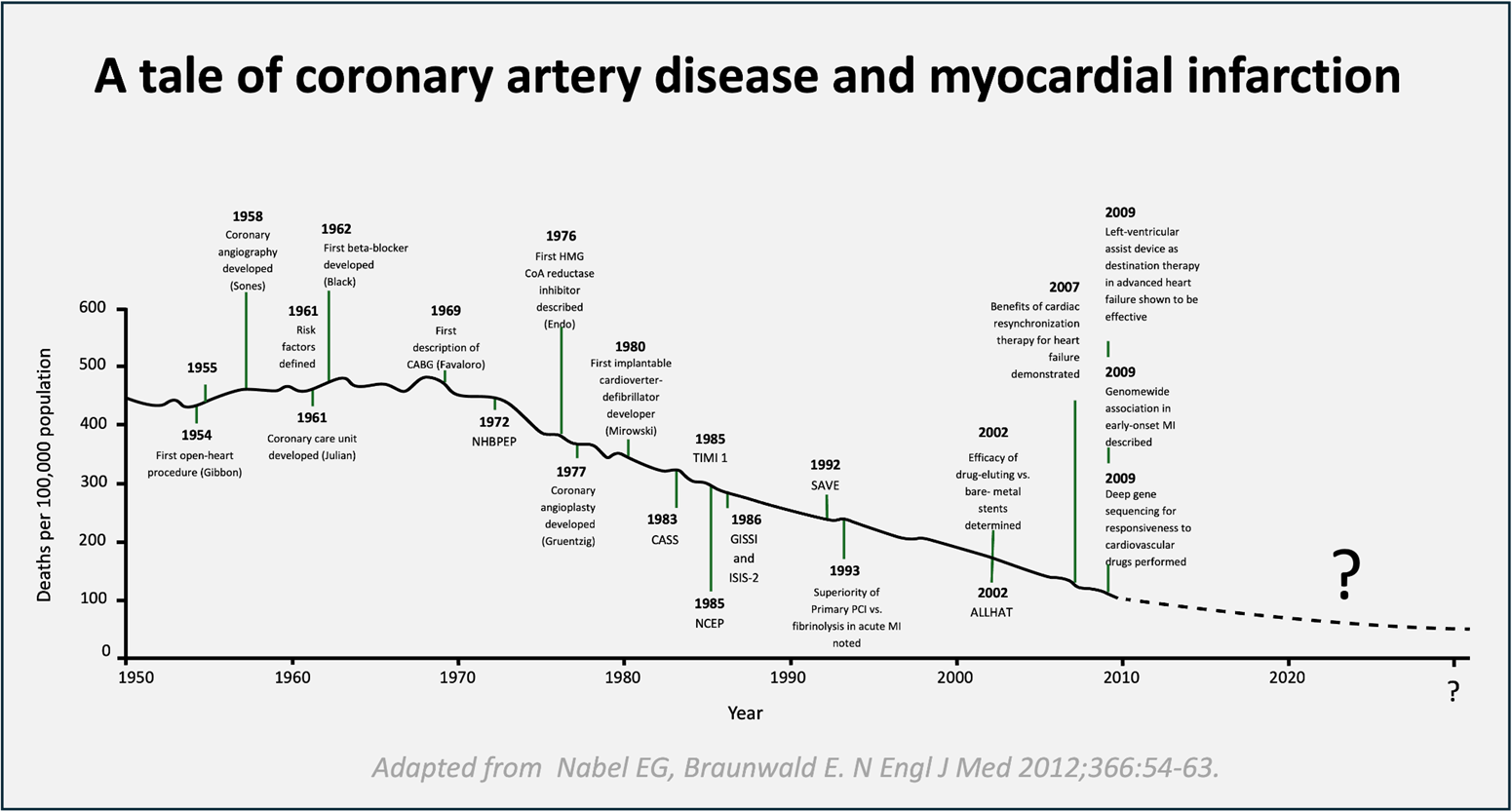
Despite significant declines in coronary artery disease (CAD) and myocardial infarction (MI) mortality over the past two decades (Figure 1), cardiovascular disease remained the leading global cause of death.
Residual Risk: The Next Frontier
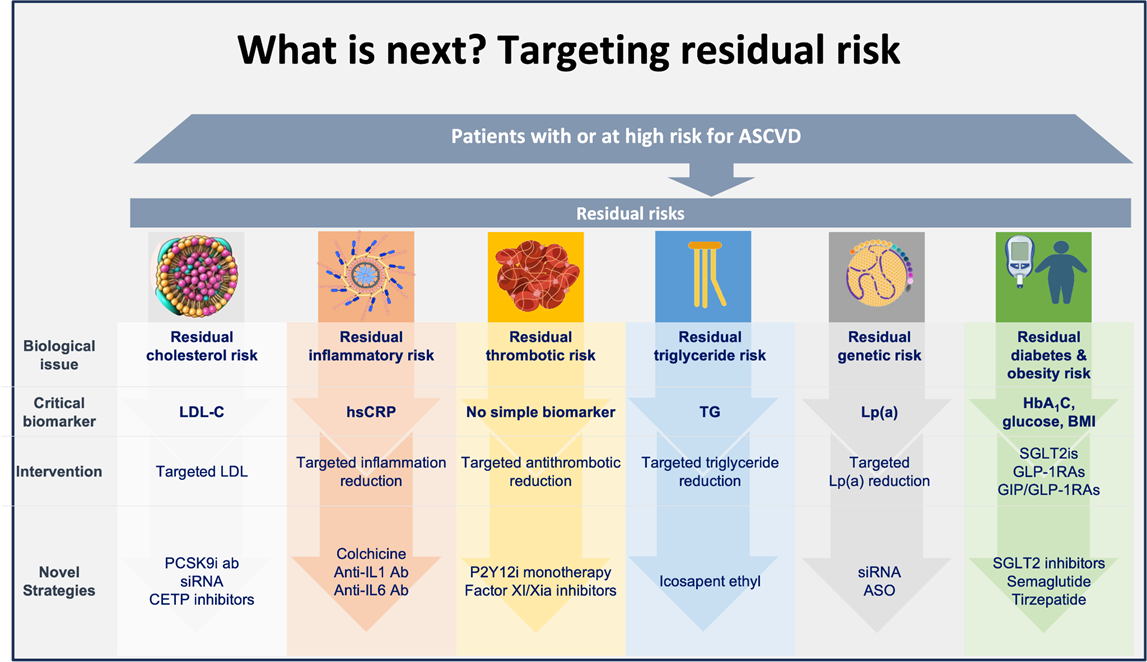
Post-PCI patients often face continued risk despite successful revascularization. These residual risks fall into three main categories—thrombotic, inflammatory, and metabolic.
Thrombotic risk will demand precision beyond standard dual antiplatelet therapy (DAPT). AI-guided tools and individualized strategies will help balance bleeding and ischemic profiles. Novel anticoagulants targeting Factor XI may offer effective protection with lower bleeding risk.
Inflammatory risk will gain prominence as trials such as CANTOS and ARTEMIS reinforce the role of cytokines in atherothrombosis. High-sensitivity CRP will guide risk assessment, and therapies targeting IL-1źŌ and IL-6 will likely be integrated into long-term management of high-risk patients.
Metabolic risk will remain multifaceted. LDL-C will continue as a key target, with inclisiran and PCSK9 inhibitors offering sustained control. A new focus on lipoprotein(a) will emerge with RNA-based therapies under investigation in the HORIZON and OCEAN(a) trials. The role of metabolic agents—such as SGLT2 inhibitors, GLP-1 receptor agonists, and tirzepatide—will expand significantly, demonstrating cardiovascular benefits even in non-diabetic populations.
Imaging-Driven Precision
Future care will rely heavily on advanced imaging for diagnosis and treatment planning. Intravascular ultrasound (IVUS) and optical coherence tomography (OCT) will be standard in PCI for optimizing outcomes. Non-invasive tools will enable comprehensive anatomical and functional evaluation, especially coronary CT angiography (CCTA) combined with CT-derived fractional flow reserve (FFR).
AI-powered plaque characterization and emerging biomarkers like perivascular fat attenuation—validated in the ORPHAN study—will support early identification of vascular inflammation and risk stratification (Figure 2).
Redefining the InterventionalistĪ»s Role
As the field evolves, interventional cardiologists will take on expanded roles—leading in acute care and long-term cardiovascular prevention. Armed with next-generation therapeutics, advanced imaging, and digital tools, they will deliver care that is as much preventive as it is interventional.
This new model defines success by restoring coronary patency, reducing future events, and improving long-term outcomes—ensuring patients leave the hospital with an open artery and a personalized strategy for lifelong cardiovascular health.
15th TCTAP Master of the Masters Award
Thursday, April 24, 11:10 AM-11:35 AM
Main Arena, Level 3
Edited by

Soo Yeon An, MD
Asan Medical Center, Korea (Republic of)

