
Jung-Min Ahn
Asan Medical Center, Korea (Republic of)
The management of antiplatelet therapy in patients who need non-cardiac surgery after percutaneous coronary intervention (PCI) with drug-eluting stents (DES) requires consideration, including the risk of stent thrombosis with cessation and bleeding with continuation. Despite current guidelines recommending the continuation of aspirin perioperatively if the bleeding risk allows, there is limited data on the continuation of aspirin in patients with prior PCI with DES who are undergoing non-cardiac surgery. In subgroup analysis of the POISE-2 trial, continuation of aspirin in patients with prior PCI reduced the risk of death or non-fatal myocardial infarction (MI) (hazard ratio [HR] 0.50; 95% confidence interval [CI] 0.26-0.95).
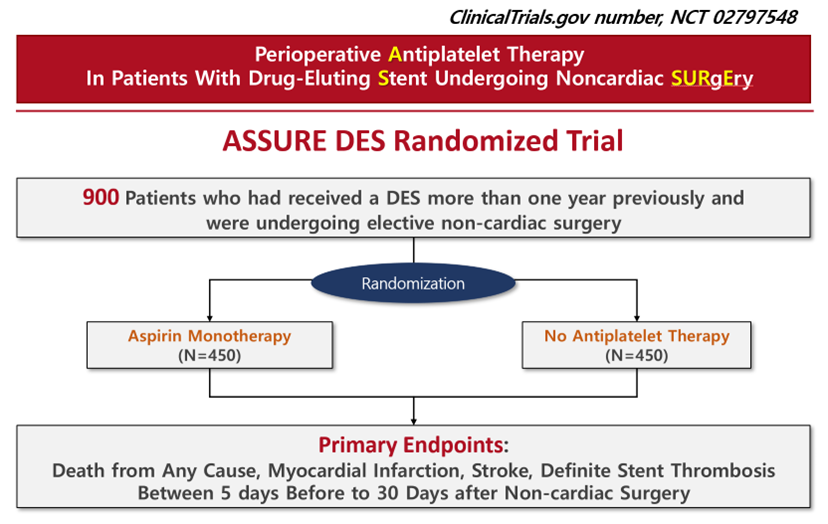
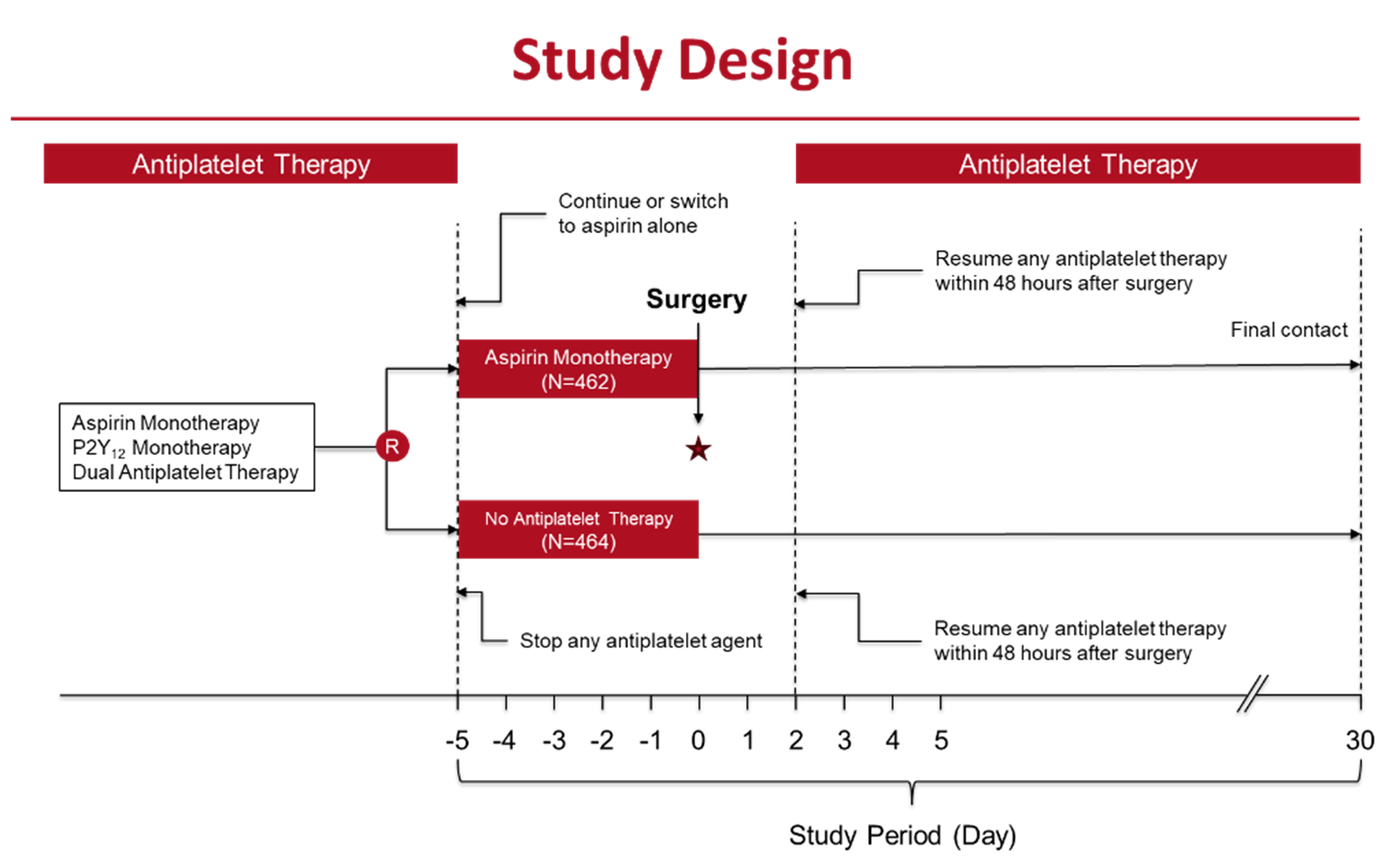
Perioperative Antiplatelet Therapy in Patients With Drug-Eluting Stent Undergoing Non-cardiac SURgEry (ASSURE-DES) trial is an investigator-initiated, prospective, multicenter, randomized controlled trial comparing the safety and efficacy of aspirin cessation or continuation in the perioperative period of non-cardiac surgery in patients who have undergone PCI with DES for more than 12 months (Figure 1,2). Key exclusion criteria include recent acute coronary syndrome (ACS) (within 1 month), severe left ventricular dysfunction (EF Ī┬ 30%), severe valvular heart disease, emergent operation, or high bleeding risk operation (e.g., intracranial, intraspinal, or retinal surgery). The primary endpoint was a composite of all-cause death, stent thrombosis, MI, and stroke from 5 days before to 30 days after surgery.
A total of 1,010 patients were randomized. Among 926 patients in the modified intention-to-treat population, the primary composite outcome occurred in 3 patients (0.6%) in the aspirin monotherapy group and 4 patients (0.9%) in the no antiplatelet group (difference, -0.2 percentage points; 95% CI: -1.3 to 0.9; p > 0.99) (Figure 3). There was no stent thrombosis in either group. The incidence of major bleeding did not differ significantly between groups (6.5% vs. 5.2%; p = 0.39), whereas minor bleeding was significantly more frequent in the aspirin group (14.9% vs. 10.1%; p = 0.027) (Figure 4).
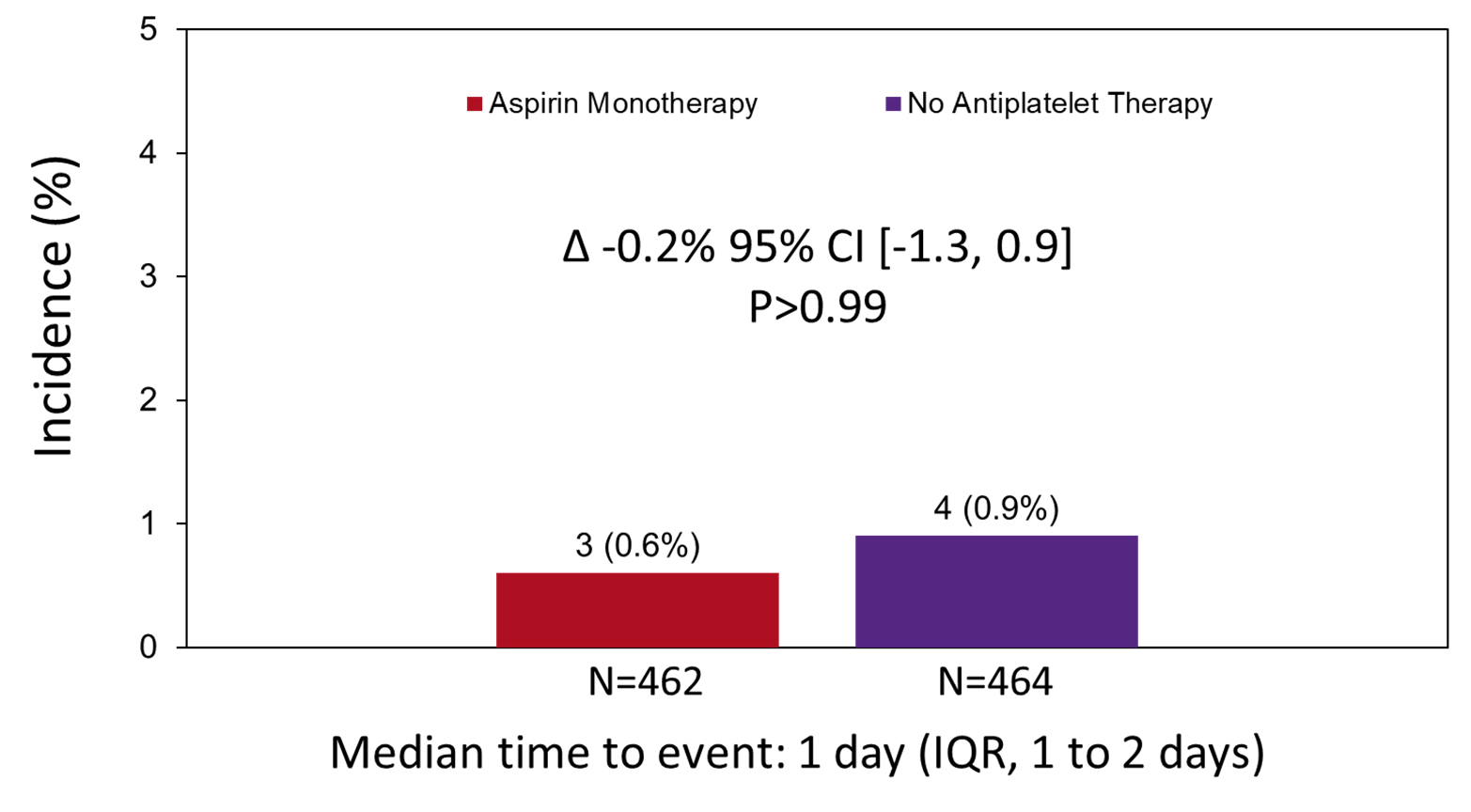
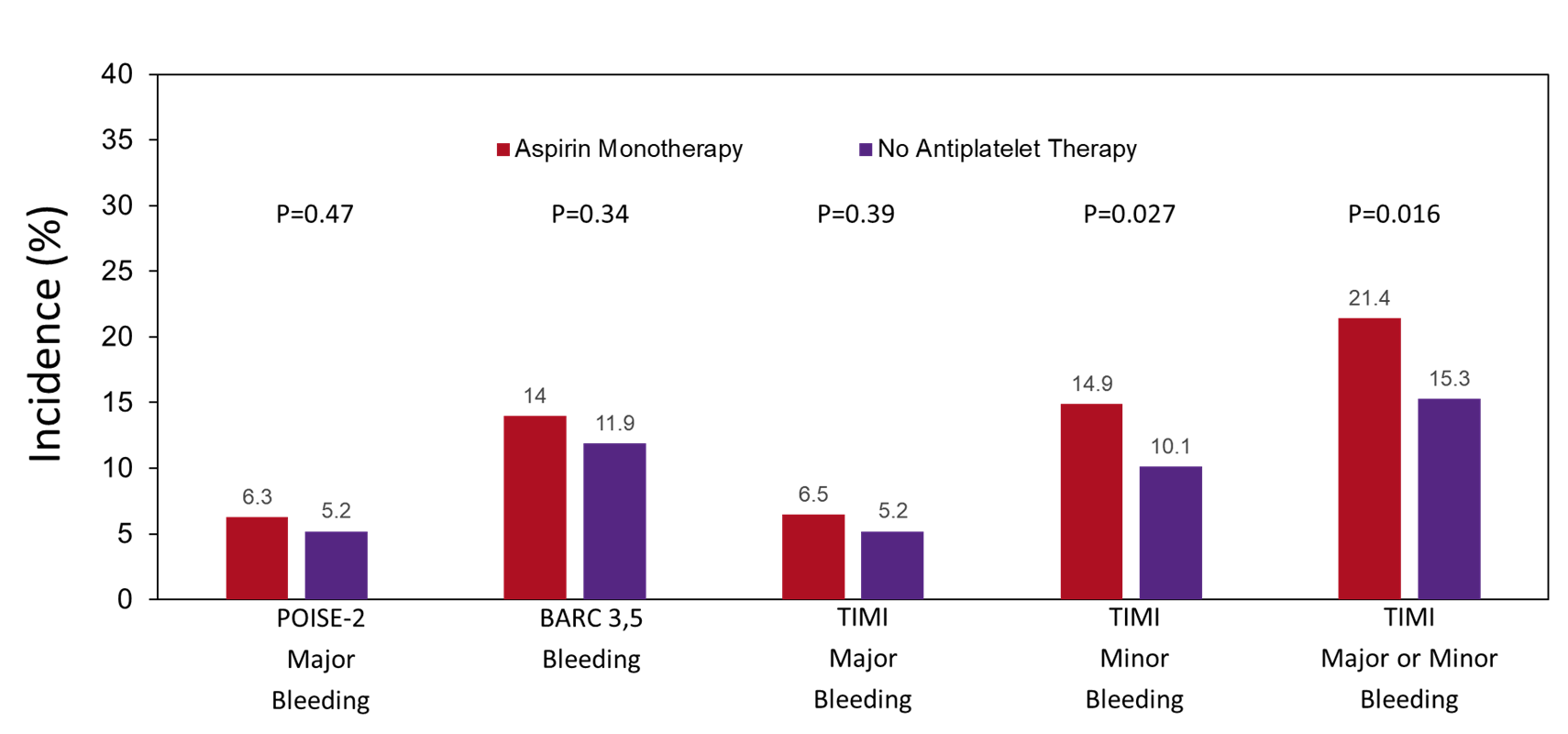
In conclusion, withholding antiplatelet therapy for 5 days before surgery may be a safe alternative to continuing aspirin in this patient population, especially when undergoing lower-risk procedures. While the event rates were low, and the study was underpowered to detect slight differences, these results could inform more flexible perioperative management strategies in future clinical practice.
Best and Novel Medical Therapy in Interventional Cardiology: What Are New in 2025?
Thursday, April 24, 3:30 PM - 5:00 PM
Presentation Room 2, Level 1
Edited by

Hansu Park, MD
Asan Medical Center, Korea (Republic of)

