
Gilbert H. L. Tang
Mount Sinai Health System, USA
At TCTAP 2025, Dr. Gilbert H. L. Tang (Mount Sinai Health System) will present a comprehensive framework to streamline Redo-TAVR procedures through simplified planning and standardized technical execution. As the number of patients receiving transcatheter aortic valve replacement (TAVR) increases, the need for effective and reproducible strategies for Redo-TAVR becomes crucial, especially in lifetime valve management. In his talk, titled "Redo-TAVR From Planning to Execution: Tips and Tricks," he will share a practical approach that enables operators to safely navigate various TAV-in-TAV scenarios while maintaining optimal hemodynamic outcomes and ensuring coronary access.
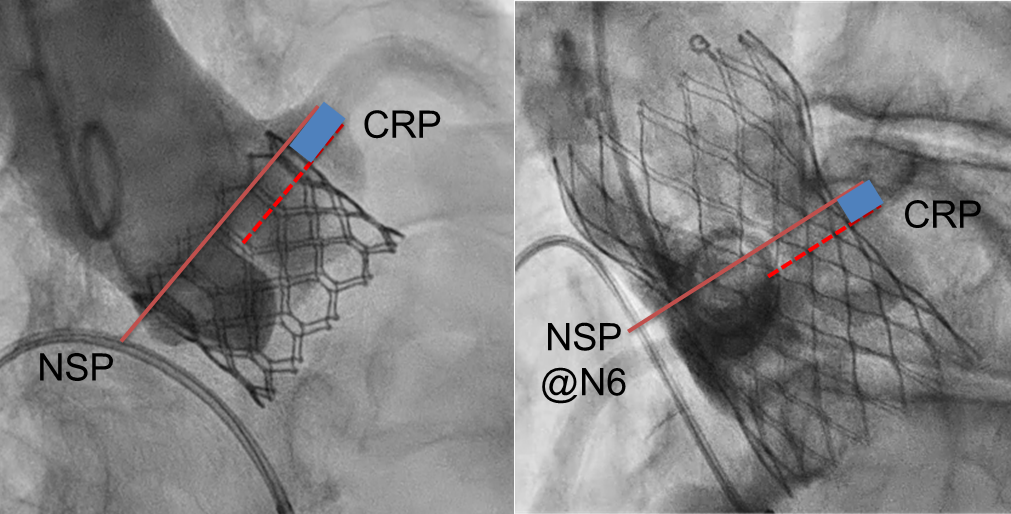
He will begin by categorizing Redo-TAVR procedures based on the interaction between the index and the second transcatheter heart valve (THV). The four possible combinations include: Short-in-Short, Short-in-Tall, Tall-in-Short, and Tall-in-Tall. This classification sets the stage for further procedural planning by determining the anatomical interaction and associated risks. By simplifying these into two scenarios based on the design of the second valve (TAV #2 – short or tall), he will guide the audience through tailored decision-making pathways. Each combination presents unique challenges related to valve positioning, coronary risk, and THV expansion. The planning process will start with a detailed evaluation of four key anatomical and procedural concepts. First, understanding the fluoroscopic markers and structural landmarks of the existing valve is essential for the successful positioning of TAV #2. Second, the neo-skirt plane (NSP), which represents the new functional skirt level after redo, is determined by the commissural post of the index valve (for tall TAV #2) or the outflow level of TAV #2 (for short TAV #2). Third, the coronary risk plane (CRP), the lowest margin of the coronary orifice, sets the lower boundary of the coronary risk zone (CRZ). Lastly, he will emphasize evaluating the CRZ by measuring the virtual to annulus (VTA) distance, which should ideally be greater than 4 mm to minimize obstruction risk. These concepts will be visualized using frame alignment views on fluoroscopy, offering an intuitive method to identify NSP and CRP for optimal TAV #2 implantation.
He will then outline a procedural strategy that translates anatomical insights into actionable techniques, beginning with identifying the index TAV and evaluating the CRZ. Next, he will focus on determining the appropriate implant position for TAV #2, which will depend on its design and the anatomical environment. Pre-dilatation of the index TAV will be highlighted as a critical step, especially in underexpanded or stenotic valves, to optimize the seating of TAV #2 and reduce the risk of HALT. During the implantation of TAV #2, he will recommend slow and controlled deployment to maintain coaxiality and avoid unintended valve movement, particularly in short-in-short or short-in-tall configurations. Post-dilatation will be the final optimization step to ensure adequate expansion of TAV #2, minimize perivalvular leak, and improve overall hemodynamic performance.
Throughout the presentation, he will illustrate real-world case examples involving valve pairs, such as SAPIEN 3 Ultra RESILIA, in Evolut PRO or Navitor Vision. He will highlight the importance of coaxial alignment, stiff wire manipulation, and the role of coronary protection in borderline CRZ measurements, such as those with VTA between 2 and 4 mm. He will stress that post-dilatation alone cannot correct underexpanded index valves, reinforcing the importance of aggressive pre-dilatation to optimize long-term outcomes.
The proposed Redo-TAVR strategy will also emphasize the value of standardization. With pamobile tools such as the "Redo TAV" app (developed by Vinnie Bapat, Miho Fukui, et al.), operators can access procedural checklists and visualize anatomical landmarks in real-time. By demystifying the Redo-TAVR workflow, he aims to provide a reproducible roadmap that reduces variability in outcomes while ensuring safety across complex anatomical subsets.
He will conclude by emphasizing that Redo-TAVR can be simplified through structured planning and meticulous execution. Frame alignment fluoroscopy will be critical to determine NSP and CRP. Pre-dilatation will remain essential for procedural success and long-term valve durability. Positioning of TAV #2 should prioritize coaxiality and depth control, while slow inflation during deployment will reduce the risk of valve migration and coronary obstruction. As Redo-TAVR becomes a more frequent necessity in lifetime valve care, his approach is expected to shape procedural standards and provide clarity for interventional cardiologists navigating this evolving field.
TAVR: Key Issues in 2025
Thursday, April 24, 8:10 AM-9:50 AM
Valve & Endovascular Theater, Level 1
Edited by

Cheol Hyun Lee, MD
Keimyung University Dongsan Medical Center, Korea (Republic of)

