Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-147
A Challenging Case of Distal Coronary Artery Guidewire Perforation
By Sivayos Deetes
Presenter
Sivayos Deetes
Authors
Sivayos Deetes1
Affiliation
Maharat Nakhon Ratchasima Hospital, Thailand1,
View Study Report
TCTAP C-147
Coronary - Complication Management
A Challenging Case of Distal Coronary Artery Guidewire Perforation
Sivayos Deetes1
Maharat Nakhon Ratchasima Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
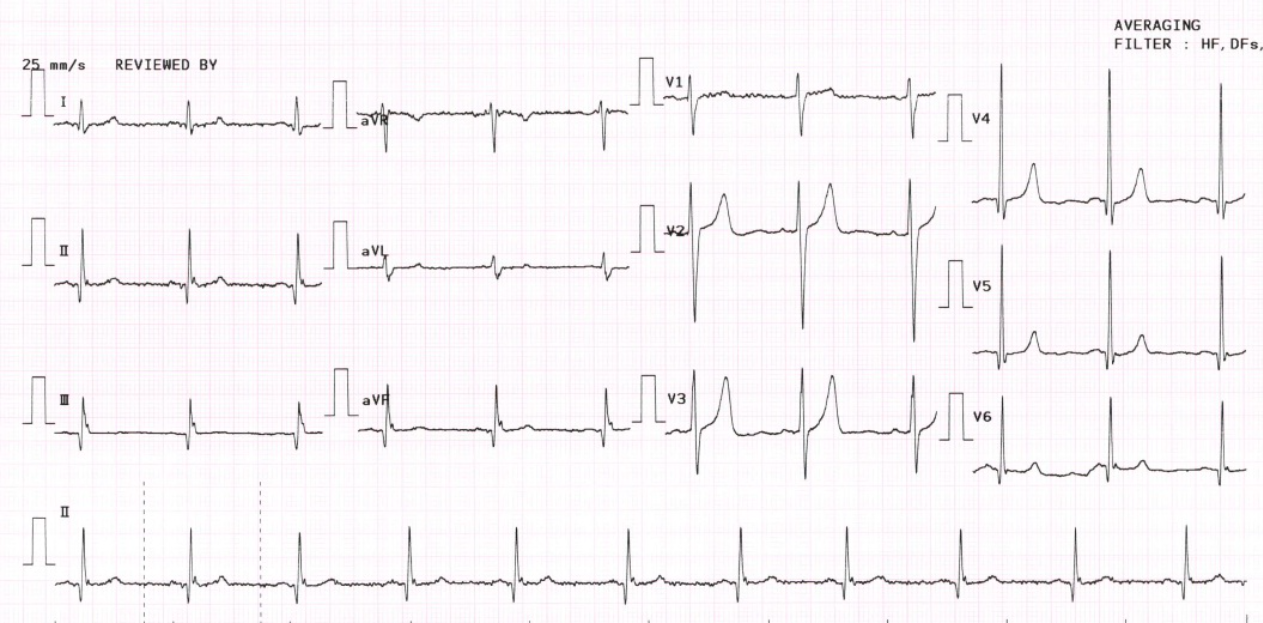
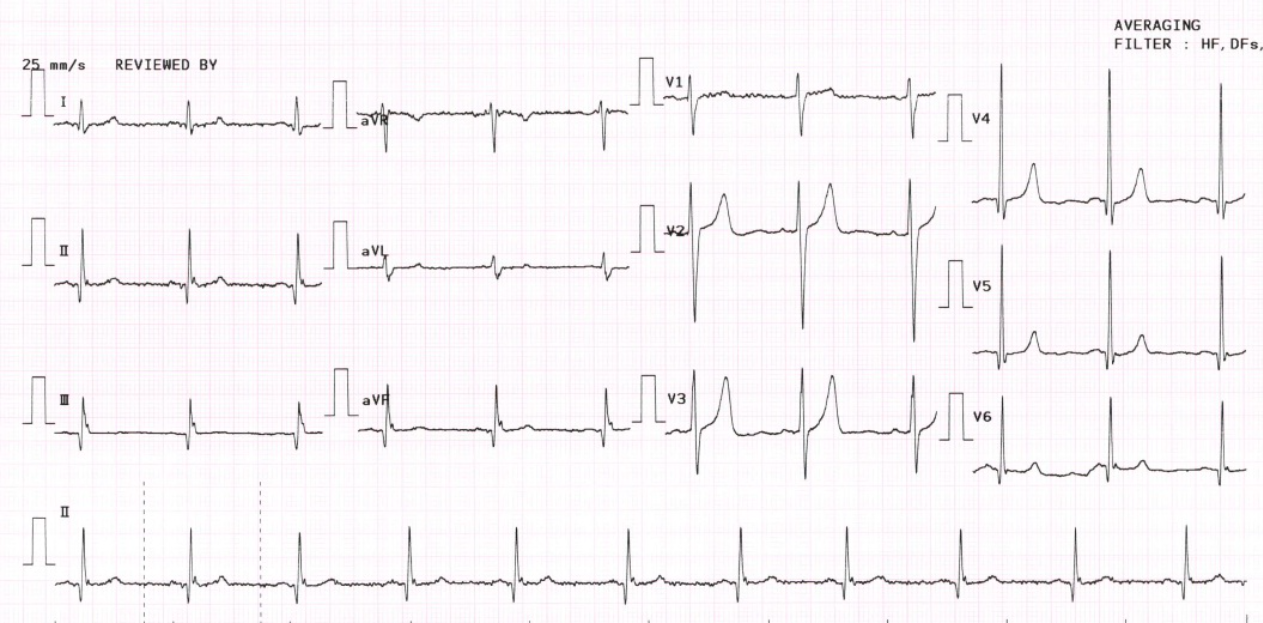
A 67-year-old man with a history of type 2 diabetes, hypertension, and ischemic stroke was sent from an ophthalmologist due to abnormal electrocardiogram (ECG) which showed normal sinus rhythm with Q wave in lead II, III, and AVF. He denied having any symptoms such as chest pain, shortness of breath, or clinical features of heart failure. Physical examination was unremarkable.
Relevant Test Results Prior to Catheterization
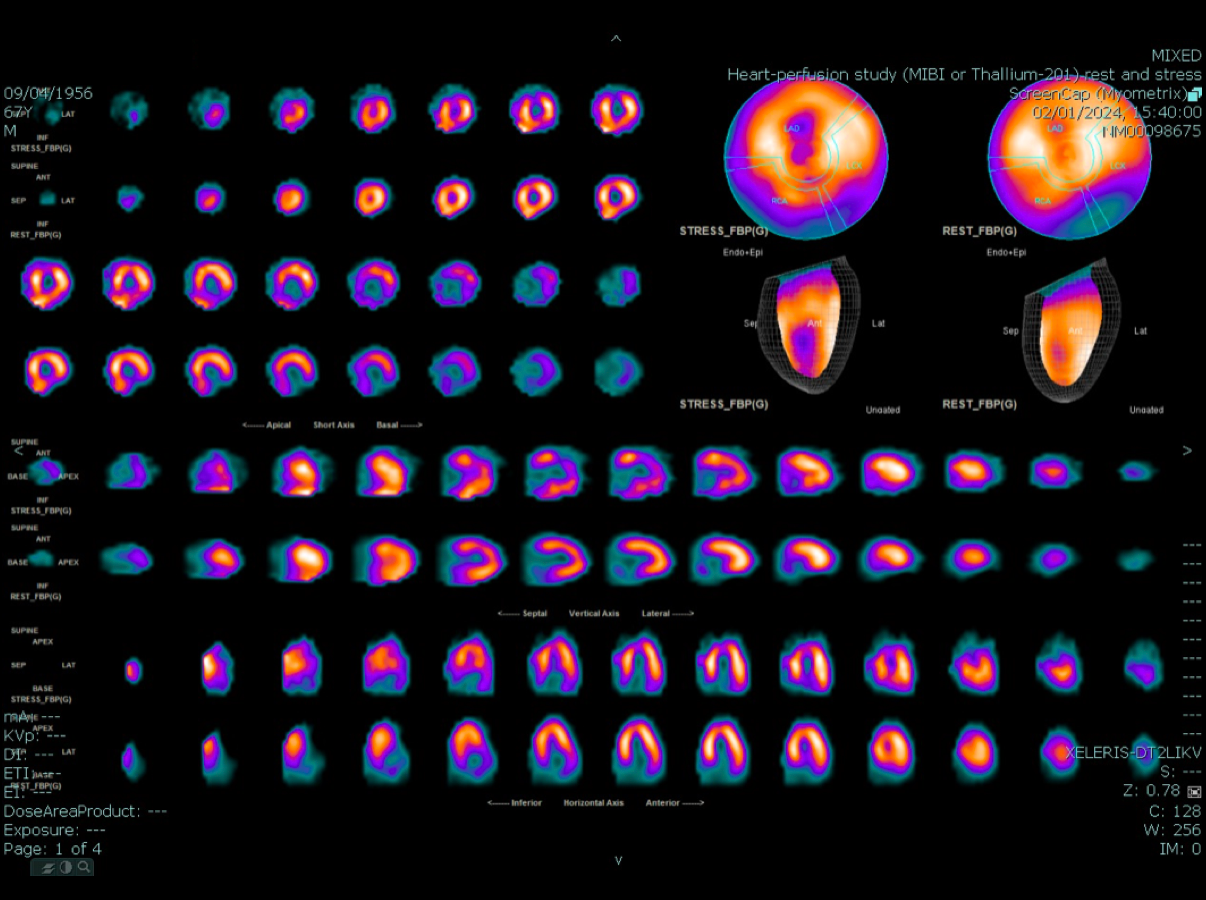
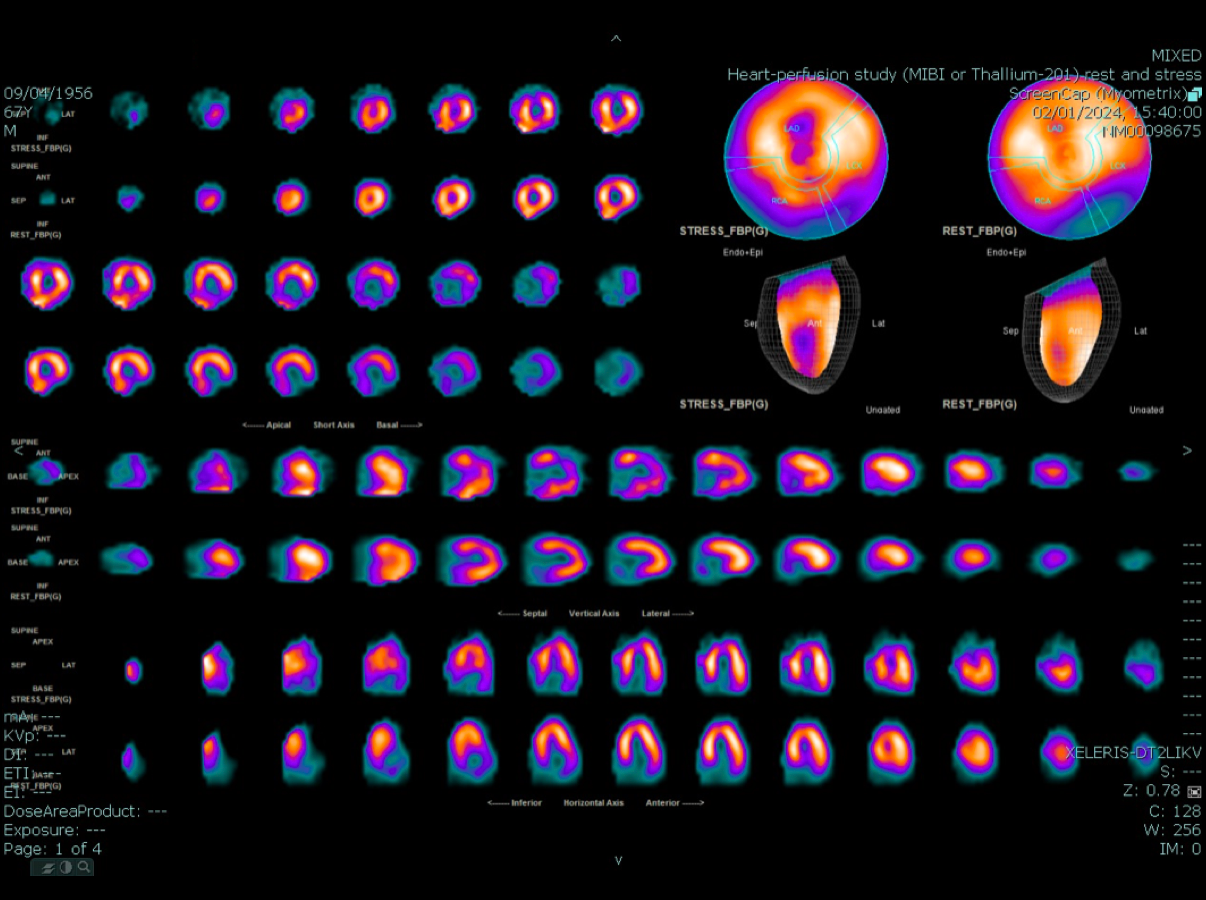
A chest X-ray revealed no cardiomegaly or evidence of pulmonary congestion. Transthoracic echocardiography (TTE) showed moderate LV systolic dysfunction (LVEF estimated 35-40%) with hypokinesia of the inferior and inferoseptal wall, and no sign of valvular heart disease. A Tc-99m MIBI Gated SPECT MPI was performed to evaluate coronary artery disease and showed suggestive evidence of myocardial ischemia at the apex, apical anterior segments and stress-induced hypokinesia at inferior, inferoseptal wall.


Relevant Catheterization Findings
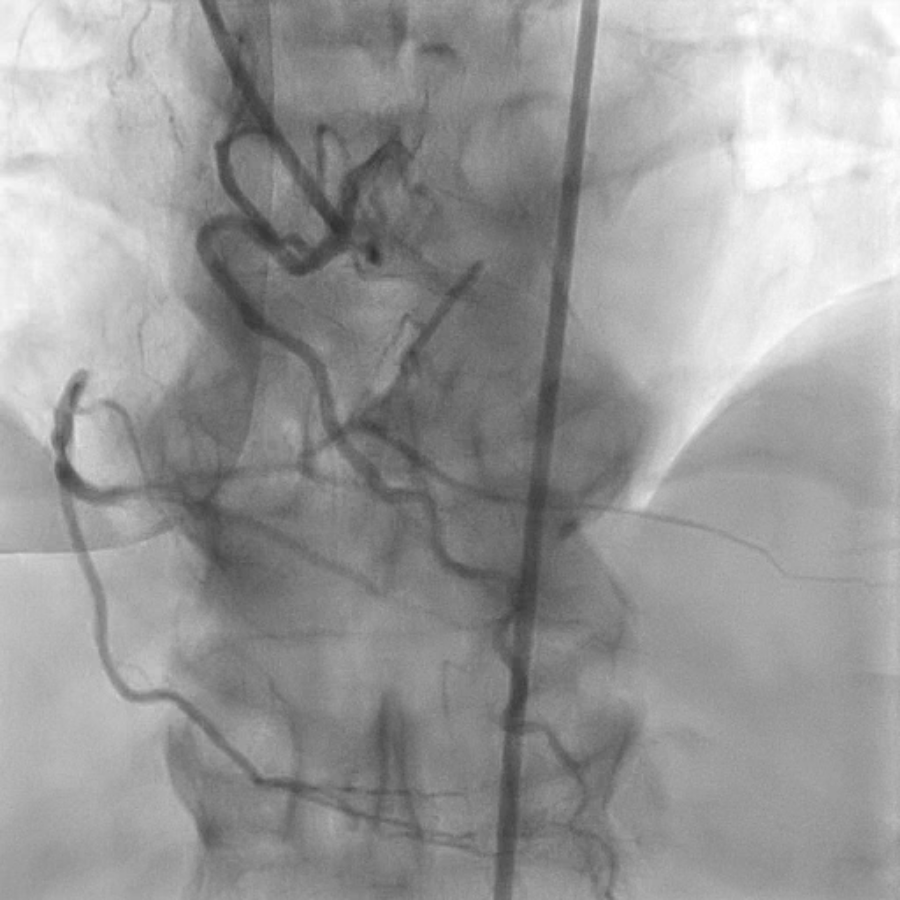
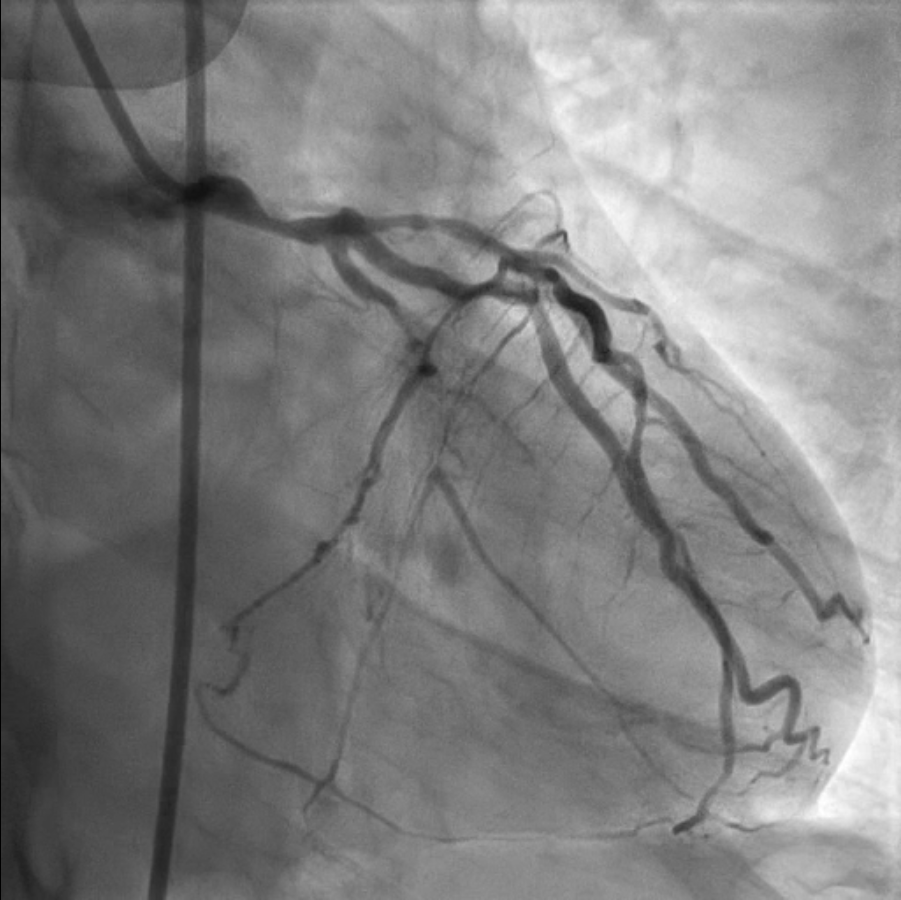
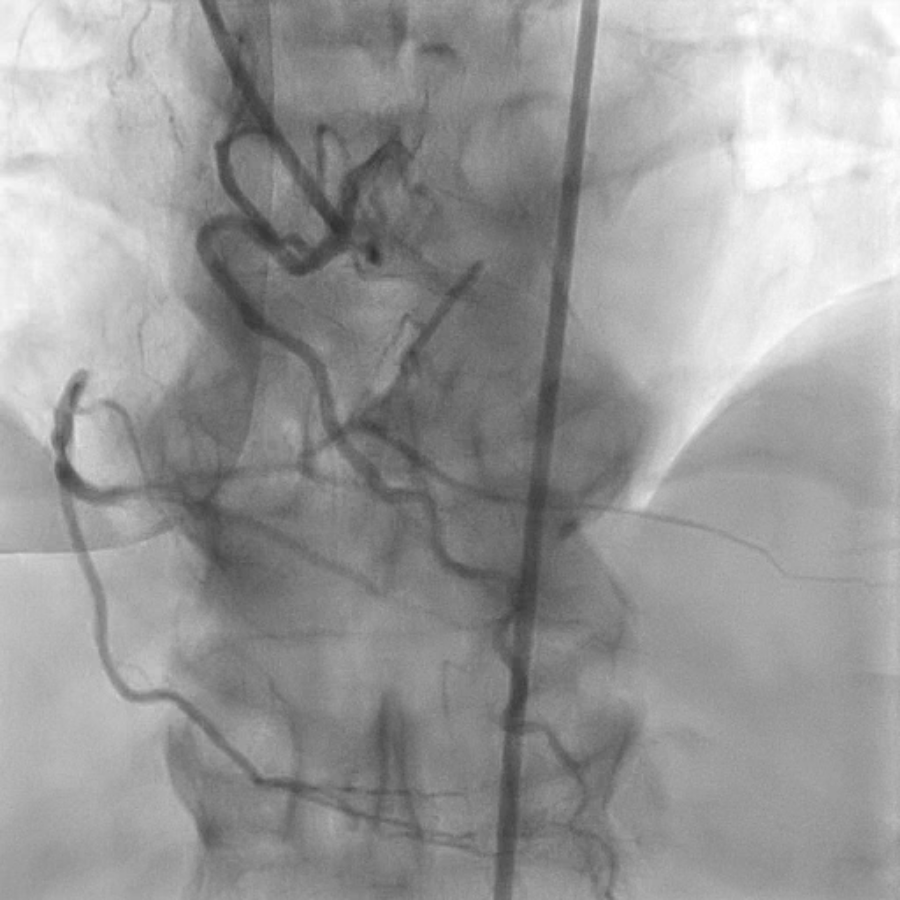
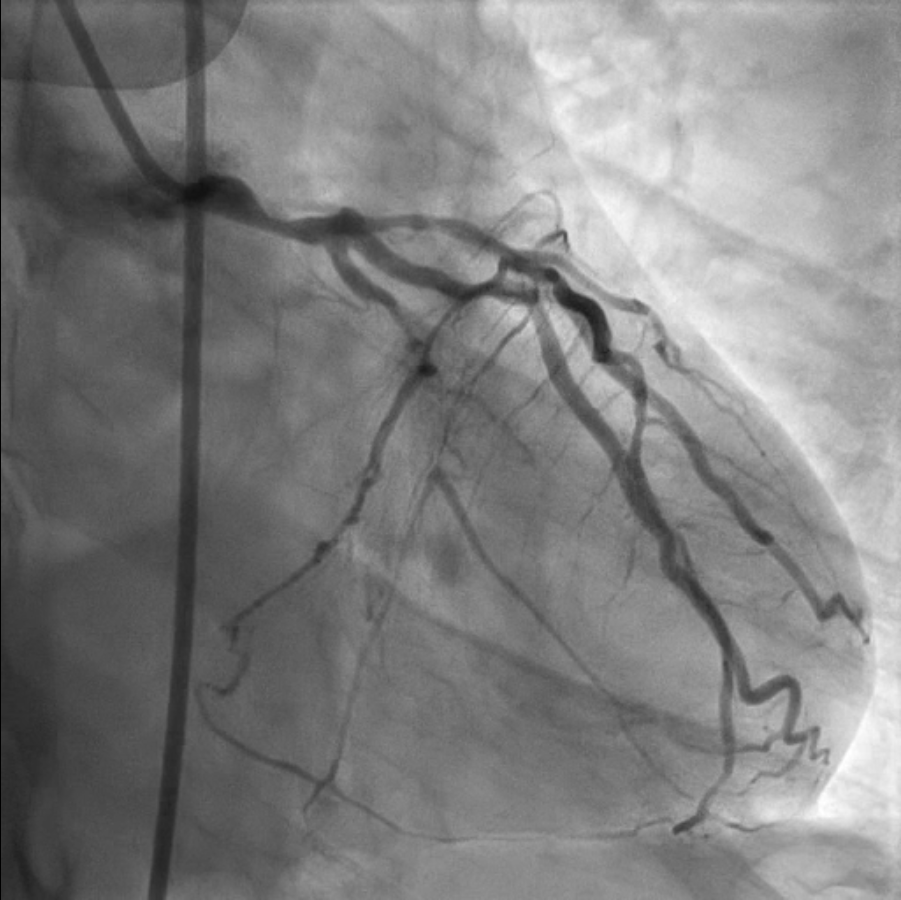
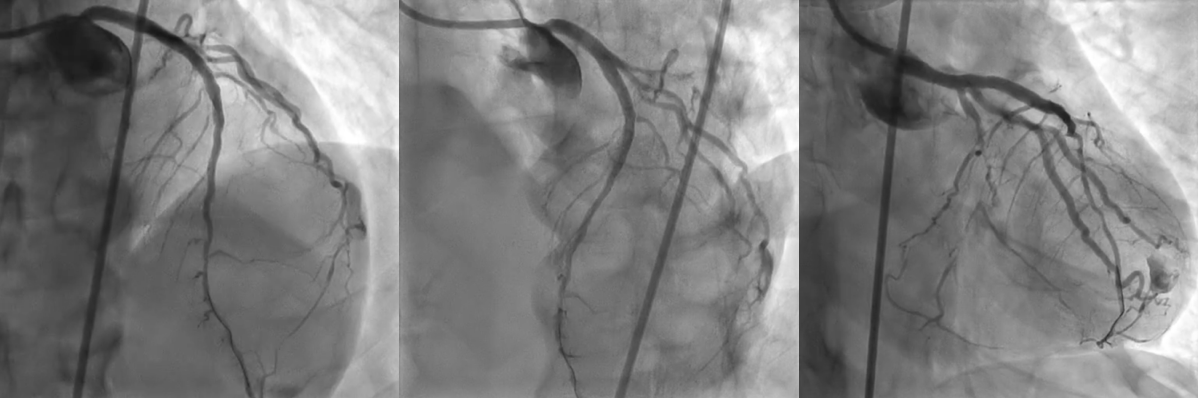
Coronary angiography (CAG) was done and showed right coronary dominance with a heavily calcified vessel of left main (LM) with stenosis 70% of mid LM, a calcified vessel of left anterior descending artery (LAD) with diffuse stenosis 80% of proximal to mid LAD, chronic total occlusion of proximal left circumflex artery (LCx), and heavily calcified vessel of right coronary artery (RCA) with chronic total occlusion of proximal RCA with well collateral blood supply.


Interventional Management
Procedural Step
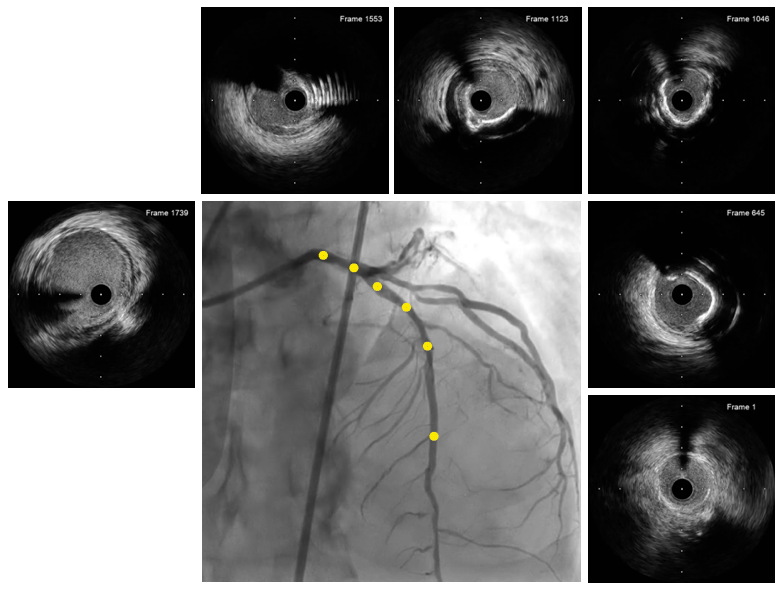
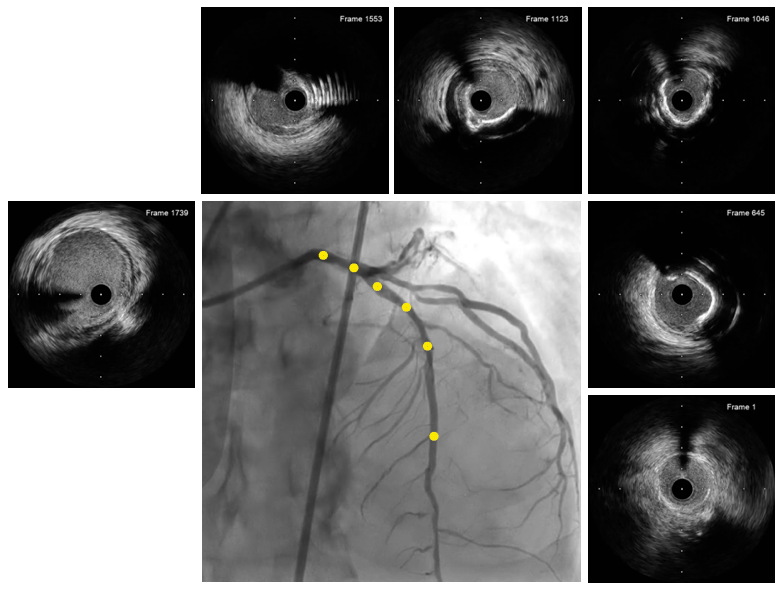
Percutaneous coronary intervention (PCI) was initiated by a right femoral approach using a 7 Fr PB 3.5 guide catheter, which placed a sion black guidewire in the LAD. A rotational atherectomy (Rota burr 1.75 mm) was performed due to calcified vessel of LAD. Intravascular ultrasound (IVUS), used to evaluate the LAD lesion before stenting, showed diffuse fibrocalcific atherosclerotic plaque along LAD. A 3.5 mm x 28 mm everolimus-eluting stent was deployed in proximal to mid LAD and a 4.0 x 33 mm everolimus-eluting stent was implanted in LM ostium to proximal LAD, irrespectively. Post-dilatation with a 3.5 x 12 mm non-compliant balloon and a 4.5 x 15 mm non-compliant balloon was done.
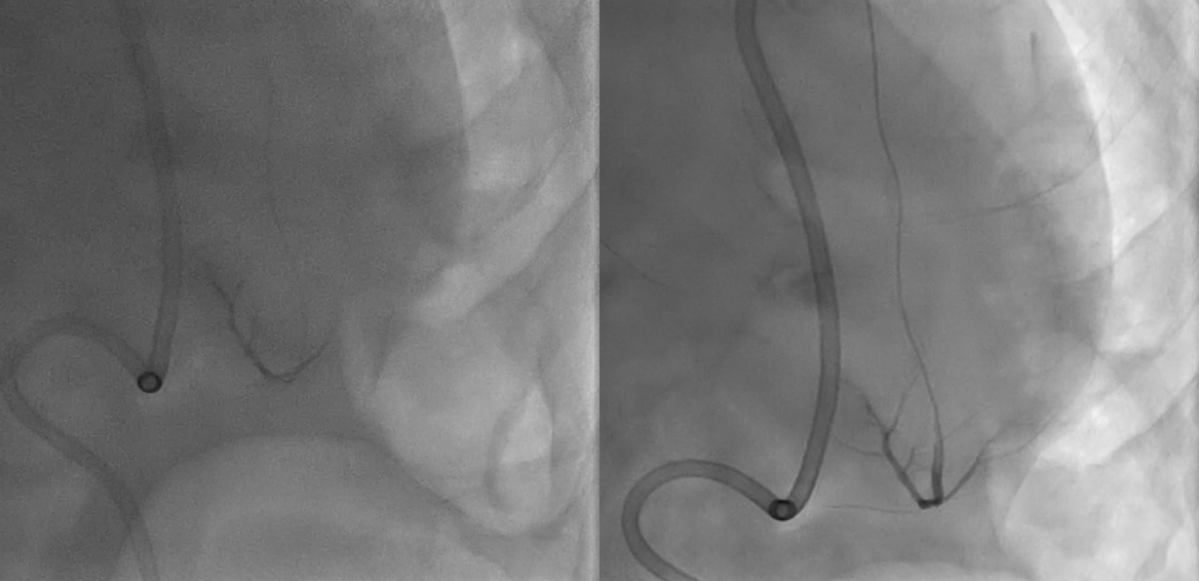
After stent implantation, the patient developed hypotension which an arterial pressure of 89/68 mmHg and CAG revealed evidence of type III coronary artery perforation (Ellis classification) at distal LAD. Bedside TTE was performed and demonstrated pericardial effusion with tamponade physiology. Prompt resuscitation with bolus intravenous fluid, emergent pericardiocentesis with autologous blood reinfusion through the subxiphoid approach using 6F pericardial sheath, and gelfoam embolization via microcatheter to treat distal LAD perforation were performed. Follow-up CAG showed no evidence of coronary artery perforation and the patient's hemodynamics became stable.
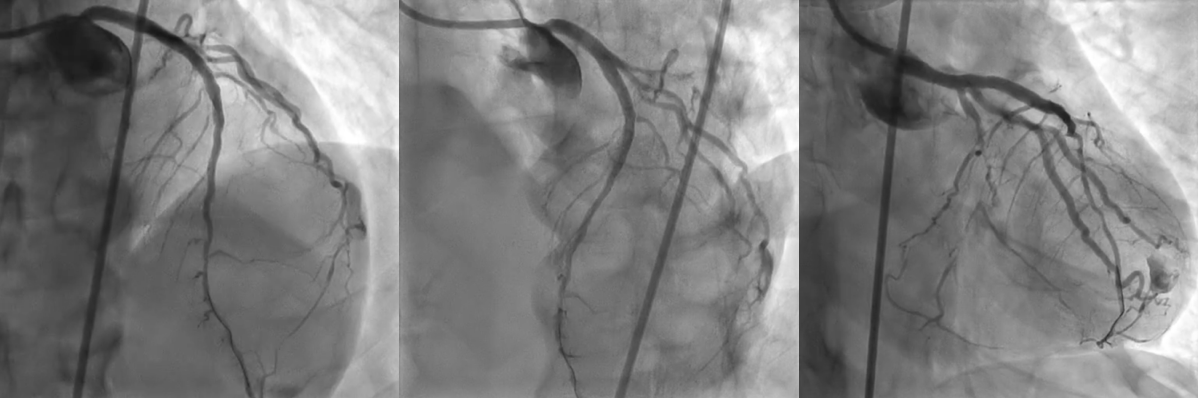
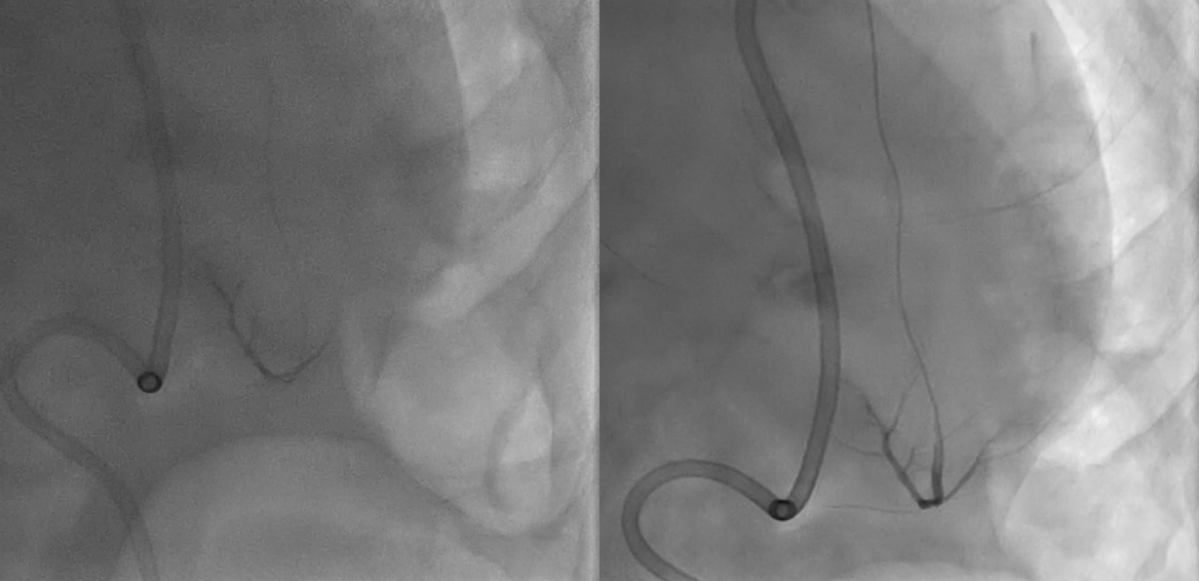
After stent implantation, the patient developed hypotension which an arterial pressure of 89/68 mmHg and CAG revealed evidence of type III coronary artery perforation (Ellis classification) at distal LAD. Bedside TTE was performed and demonstrated pericardial effusion with tamponade physiology. Prompt resuscitation with bolus intravenous fluid, emergent pericardiocentesis with autologous blood reinfusion through the subxiphoid approach using 6F pericardial sheath, and gelfoam embolization via microcatheter to treat distal LAD perforation were performed. Follow-up CAG showed no evidence of coronary artery perforation and the patient's hemodynamics became stable.
Case Summary
Coronary artery perforation is a rare but serious complication of PCI that is associated with significant morbidity and mortality. Prompt recognition and treatment are essential to prevent immediate life-threatening complications. Management of coronary artery perforation depends on its severity and associated hemodynamic compromise. The presence of coronary artery perforation should encourage immediate echocardiography, and when a large pericardial effusion is associated with tamponade physiology, emergent pericardiocentesis is indicated.