Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-180
Primary PCI Nightmare: Using Guide Extension Catheter as Aspiration Device in Rural Area
By Robin Hendra Wibowo
Presenter
Robin Hendra Wibowo
Authors
Robin Hendra Wibowo1
Affiliation
Pasundan University, Indonesia1,
View Study Report
TCTAP C-180
Coronary - High-Risk Intervention (Diabetes, Heart Failure, Renal Failure, Shock, etc)
Primary PCI Nightmare: Using Guide Extension Catheter as Aspiration Device in Rural Area
Robin Hendra Wibowo1
Pasundan University, Indonesia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 74-year-old male, active smoker, presented to the emergency department complaining of chest pain. The pain began suddenly since 3 hour while he was resting at home. He described the pain as burning, 9 out of 10 in intensity, substernal, and associated with nausea, diaphoresis, and dyspnea. Vital signs at admission was systolic blood pressure of 60 mmHg with palpation, heart rate at 60 bpm, respiratory rate 26 times perminute and physical examination were unremarkable.
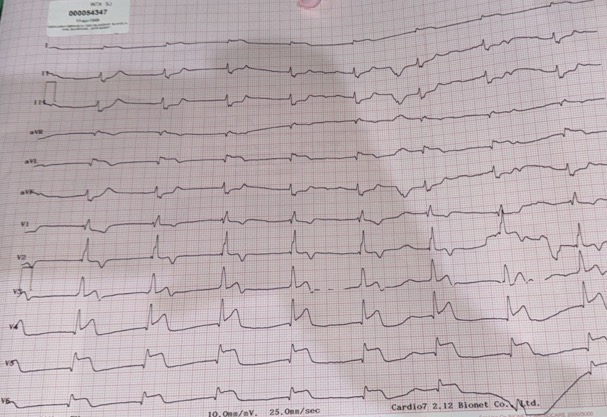
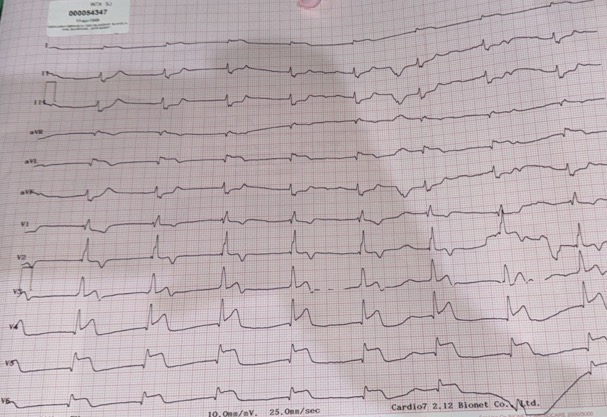
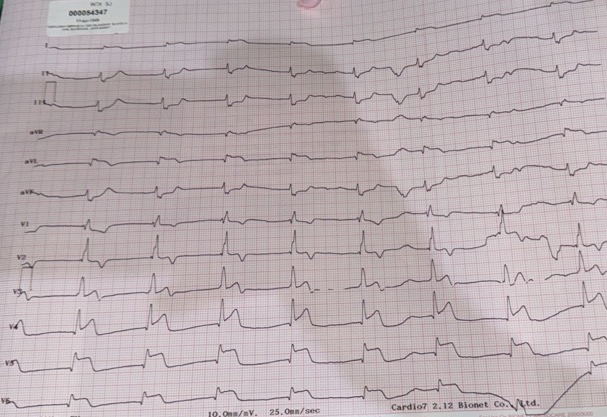
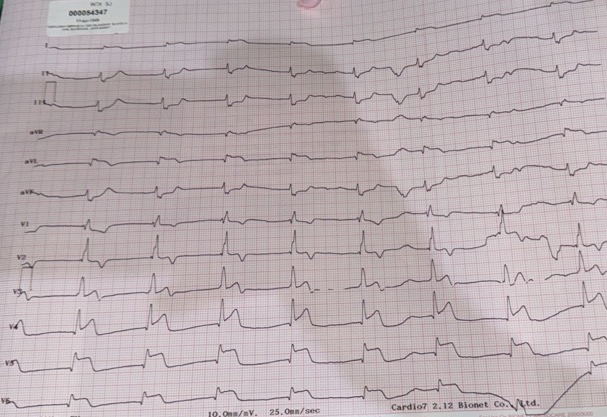
Relevant Test Results Prior to Catheterization
His Electrocardiogram (ECG) showed junctional Rhythm, ST segment elevation of anterior, anterolateral and high lateral wall. Laboratory evaluation showed High Sensitive troponin I level was elevated 1600.0 ng/ml; normal <19 ng/ml, blood sugar level 137 mg/dL, Creatinine 1,72 mg/dL, egfr 41ml/min, Natrium 134 mmlo/L, Calcium 7,8 mg/dL.
Relevant Catheterization Findings
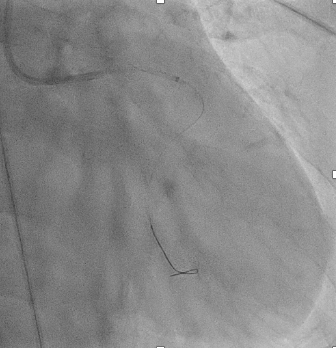
He received a loading dose of aspirin 160 mg, ticagrelor 180 mg, Enoxaparin 0.4 ml iv, and atorvastatin 40mg once daily. The patient was referred to the cathlab for primary percutaneous coronary intervention (PCI). The angiography was performed via Femoral artery access using a 6 fr sheath access. During the procedure the patient received UFH 6000 IU and NTG 200 mcg. Angiography revealed right dominant coronary artery system, total occlusion of left main artery and normal right coronary artery
Interventional Management
Procedural Step
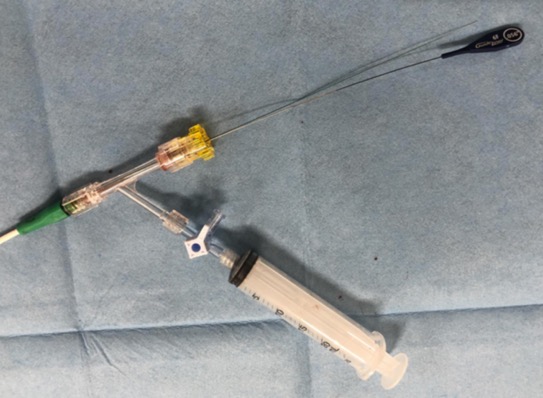
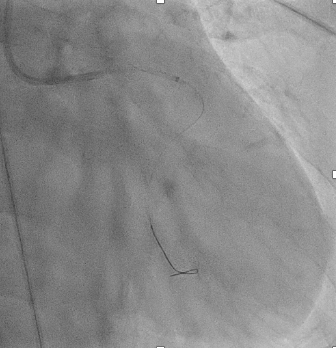
Primary PCI at the LCA was conducted using guiding catheter EBU 3.5/6F, A 0.014inch double floppy guidewire wire successfully across the lesion and is placed distal to the distal LAD and LCX. Multiple thrombus aspiration was done using the standard device. Predilatation was done using semi-compliant 2.5 x 15mm balloon with 16 atm of pressure. There was difficulties with the persistent thrombus burden that impeding the corornary flow. We decided to use 6F guide extension guideliner catheter for aspiration device and successful thombus retrieval was done. Stenting was performed with DES 3.0x29mm in proximal LAD at 14 atm pressure. Contrast injection after intervention showed TIMI Flow III, without dissection or residual stenosis.
Case Summary
We reported a 74-year-old male with STEMI and Primary PCI was done via Femoral access with guide extension catheter support as aspiration device and successfully done without any complications. With the increasing complexity of PCI procedures and the development of new tools in PCI, especially guide extension catheters, this tool helps the success rate of PCI procedures, but also has great potential to cause additional complications, especially coronary dissection. In STEMI patients undergoing primary PCI, the most important goal is the immediate restoration of blood flow.