Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-239
From Blocked to Clear: Upfront Large-Bore Aspiration Thrombectomy for Intermediate-High Risk Pulmonary Embolism
By Ji Ken Ow, Hafidz Abd Hadi, Ming Yoong Low, Afif Ashari, Ting Yuen Beh, Steven Wong Poh Hock
Presenter
Ji Ken Ow
Authors
Ji Ken Ow1, Hafidz Abd Hadi1, Ming Yoong Low1, Afif Ashari1, Ting Yuen Beh1, Steven Wong Poh Hock1
Affiliation
National Heart Institute, Malaysia1,
View Study Report
TCTAP C-239
Endovascular - Thrombus Removal Devices and Techniques
From Blocked to Clear: Upfront Large-Bore Aspiration Thrombectomy for Intermediate-High Risk Pulmonary Embolism
Ji Ken Ow1, Hafidz Abd Hadi1, Ming Yoong Low1, Afif Ashari1, Ting Yuen Beh1, Steven Wong Poh Hock1
National Heart Institute, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
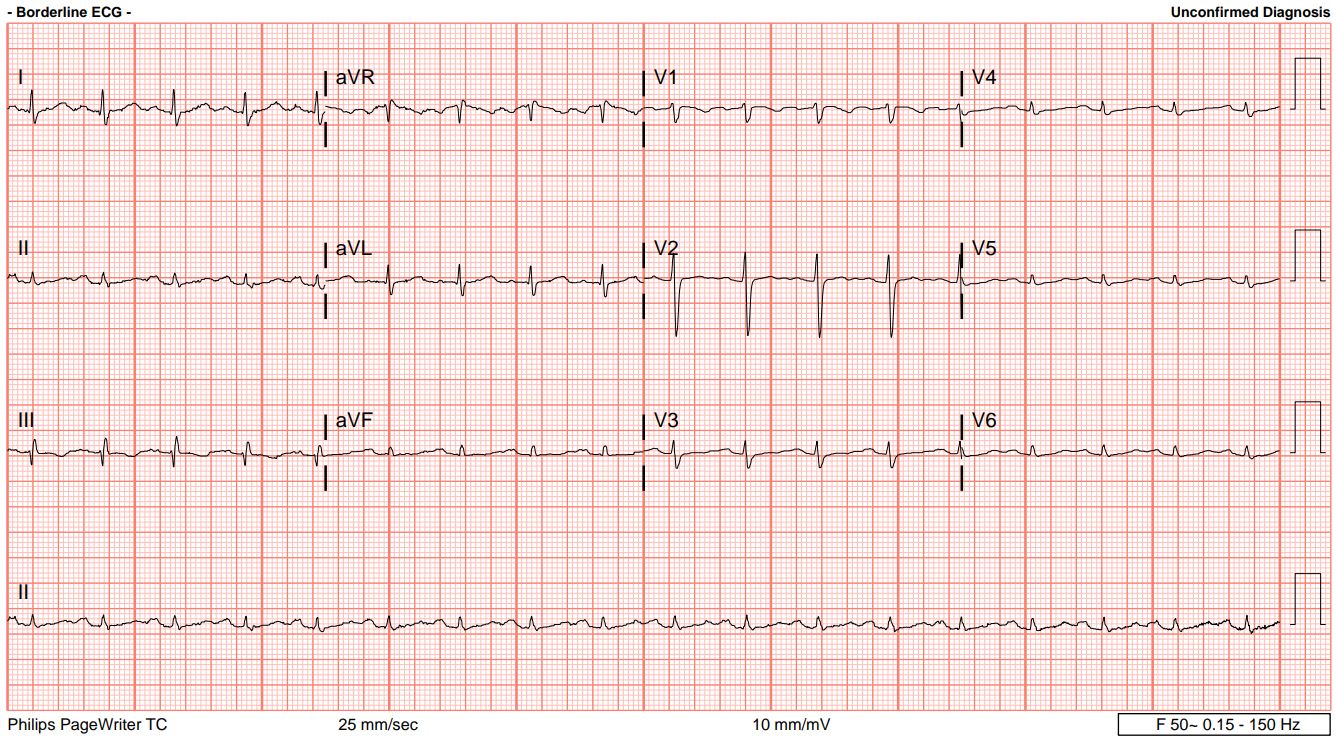
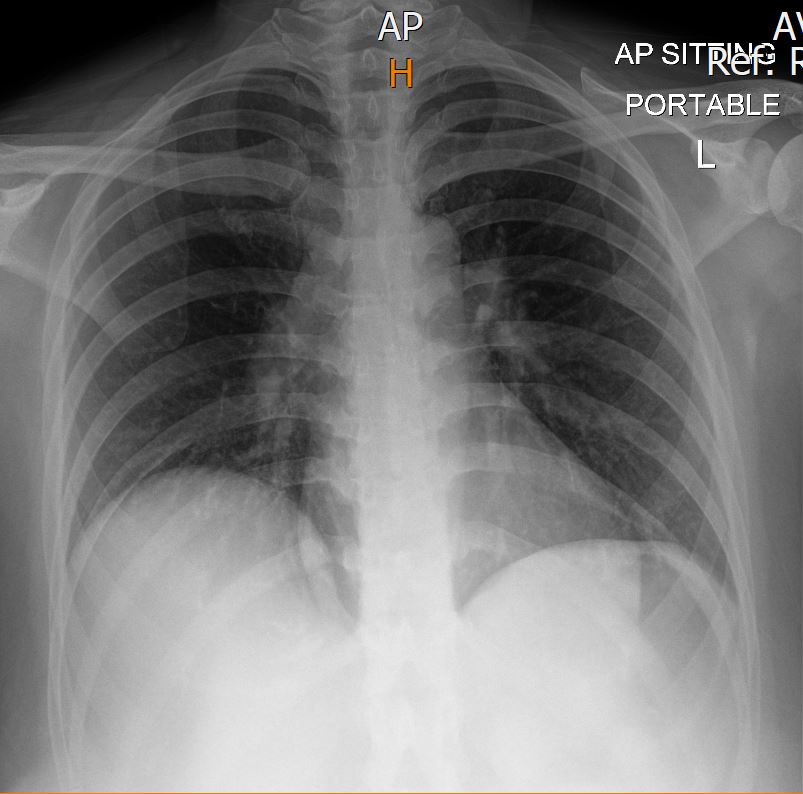
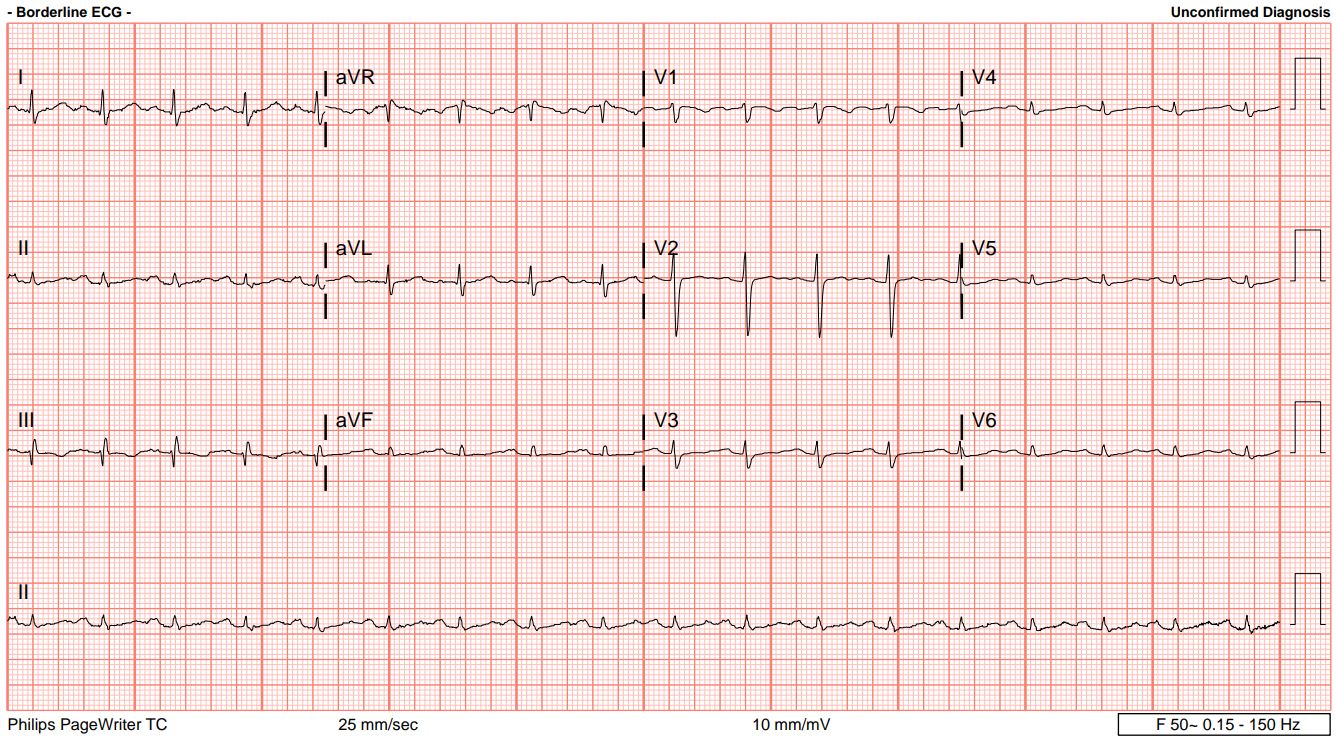
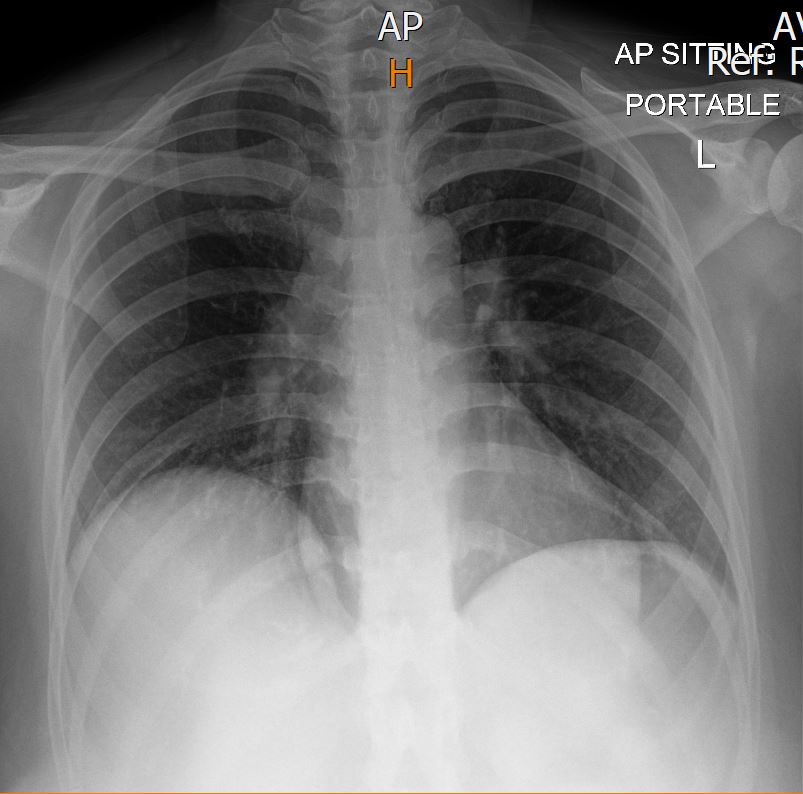
A 42-year-old woman with no known medical illness presented to the ED with shortness of breath for the past 5 days, which acutely worsened a few hours ago. On physical examination, she was tachypneic, lethargic with altered mental status, normotensive but tachycardic, and had an oxygen saturation of 92% on room air. Lung auscultation revealed reduced breath sounds bilaterally, and heart auscultation showed no murmurs. Her chest X-ray was clear, but the ECG showed a typical S1 Q3 T3 pattern.
Relevant Test Results Prior to Catheterization
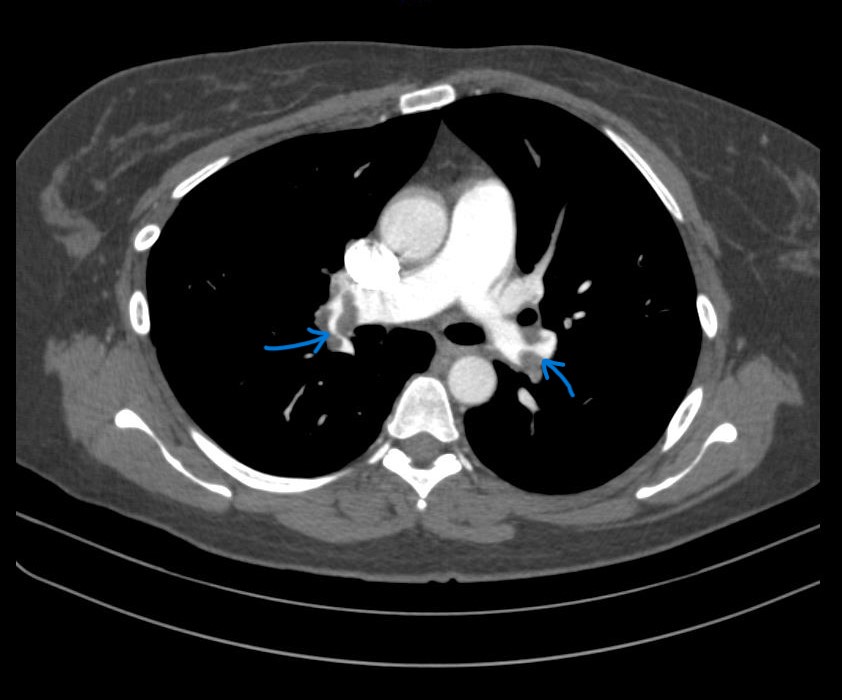
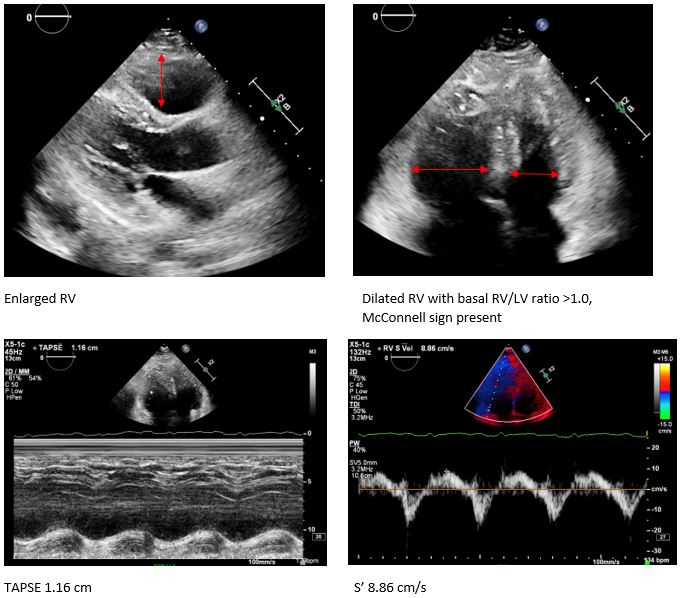
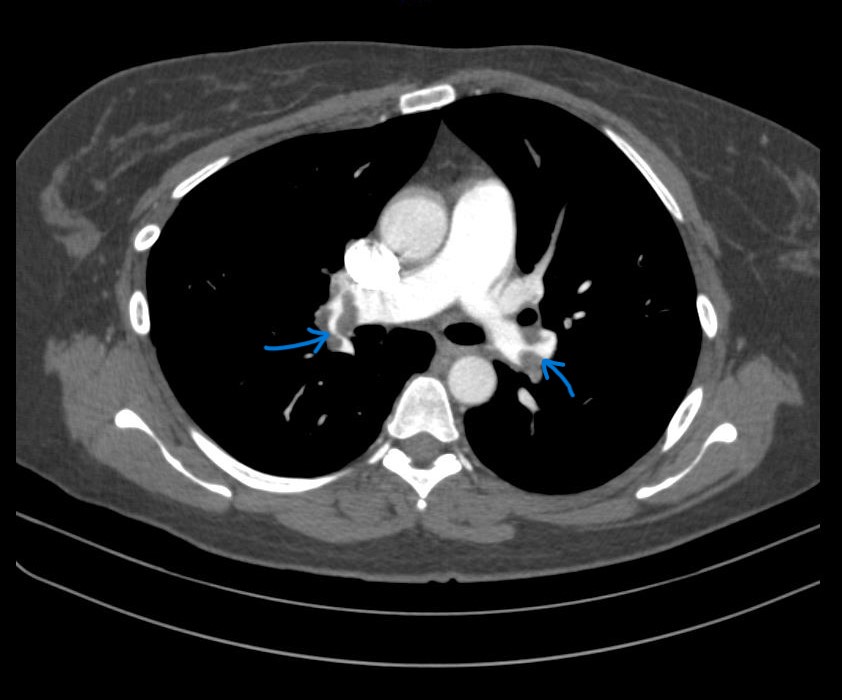
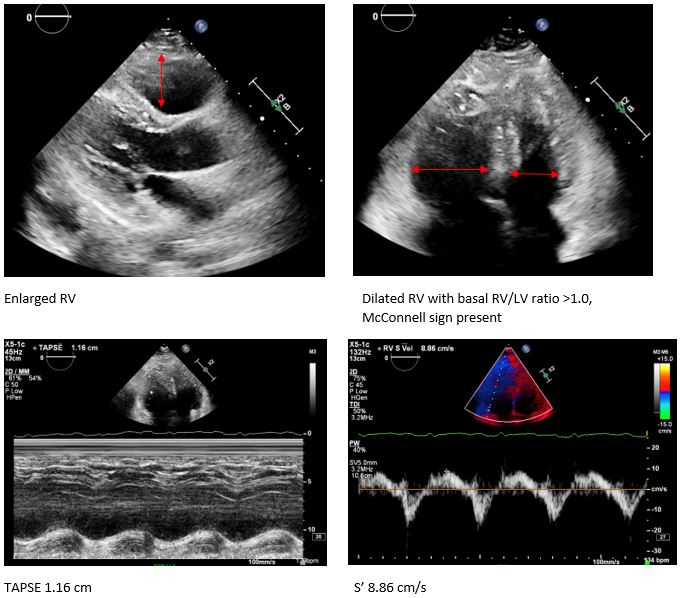
Her troponin T and D-dimer levels were both significantly elevated, at 289 pg/mL (normal < 14) and 3195 ng/mL, respectively. An ECHO revealed signs of right ventricular (RV) overload and dysfunction. Given the high clinical suspicion for pulmonary embolism, she was sent for a CT pulmonary angiogram, which confirmed a massive bilateral pulmonary embolism (PE). She was classified as Class V on the Pulmonary Embolism Severity Index (PESI) and diagnosed with intermediate-high risk PE.
Relevant Catheterization Findings
Given the clinical severity and high risk of progressive hemodynamic deterioration leading to decompensated shock, the invasive catheterization lab was activated for emergency percutaneous catheter-directed mechanical thrombectomy.
Interventional Management
Procedural Step
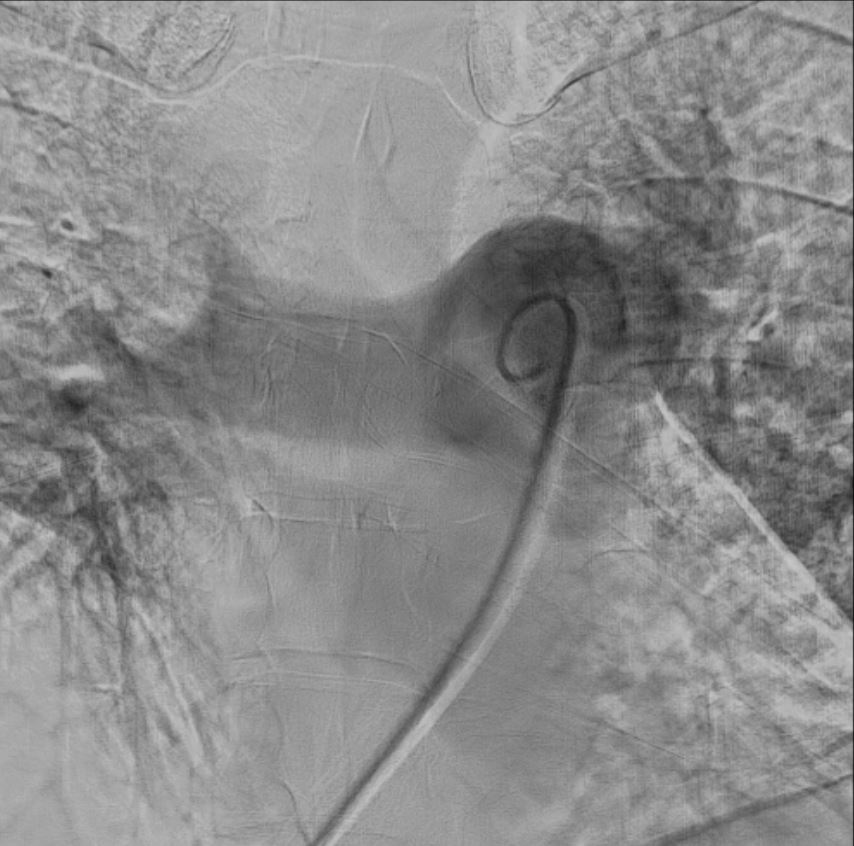
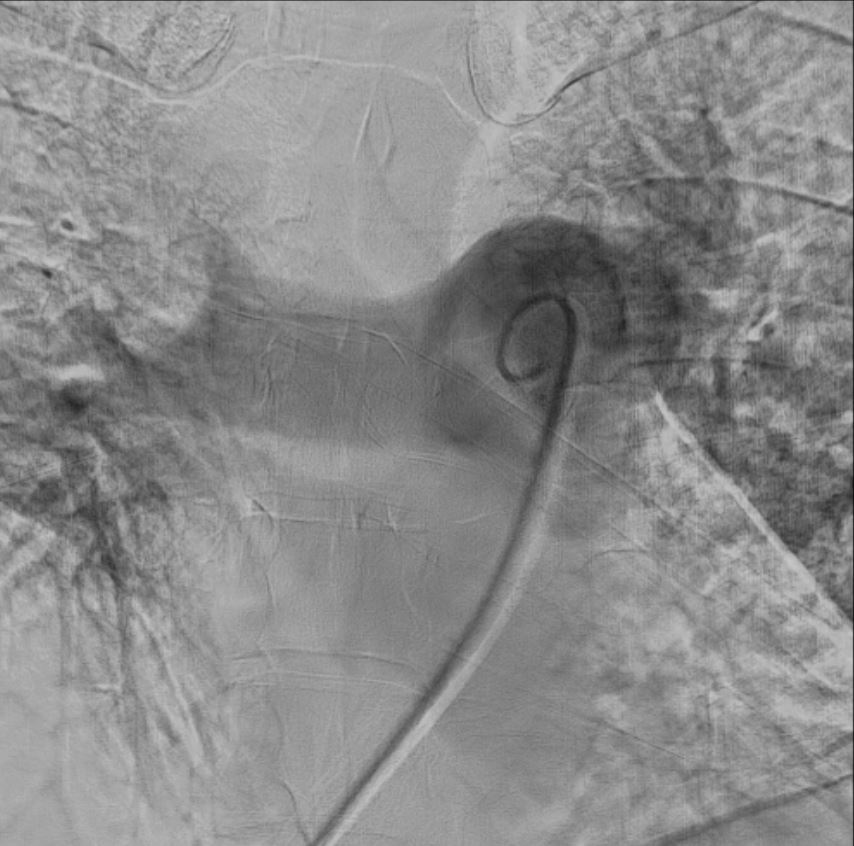
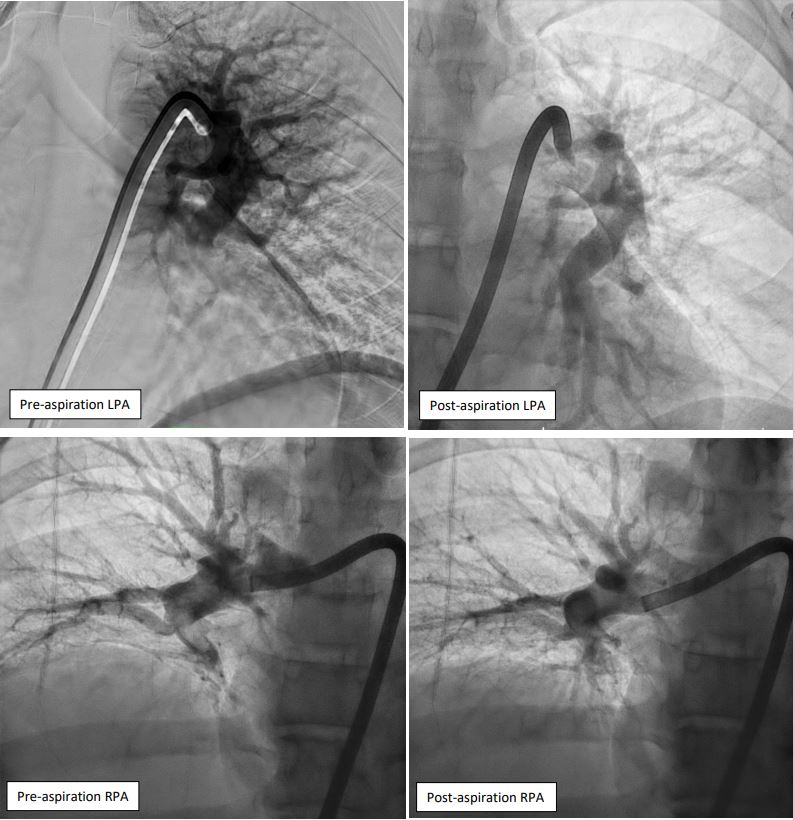
Right femoral vein access was obtained under ultrasound and fluoroscopy guidance. A 6Fr multipurpose (MP) catheter was used to deliver a J-tip guidewire into the main pulmonary artery, which was then exchanged for a pigtail catheter. Digital subtraction angiography revealed filling defects in the truncus anterior and bilateral interlobar arteries. The 6Fr femoral sheath was upsized to a 16Fr sheath. The Penumbra ENGINE and Lightning Flash 2.0 system, with a 16Fr aspiration catheter, was primed. Using the MP catheter, the J-tip guidewire was delivered into the left pulmonary artery and exchanged for the 16Fr aspiration catheter. Multiple aspiration runs were performed using the computer-assisted vacuum thrombectomy system. The same steps were repeated for the right pulmonary artery. The procedure lasted 2 hours, with 1.2L of blood loss and approximately 6-8 cubic centimeters of fresh clots aspirated. The patient received 2 units of packed red blood cells during the procedure. Femoral access was closed with a figure-of-8 suture.
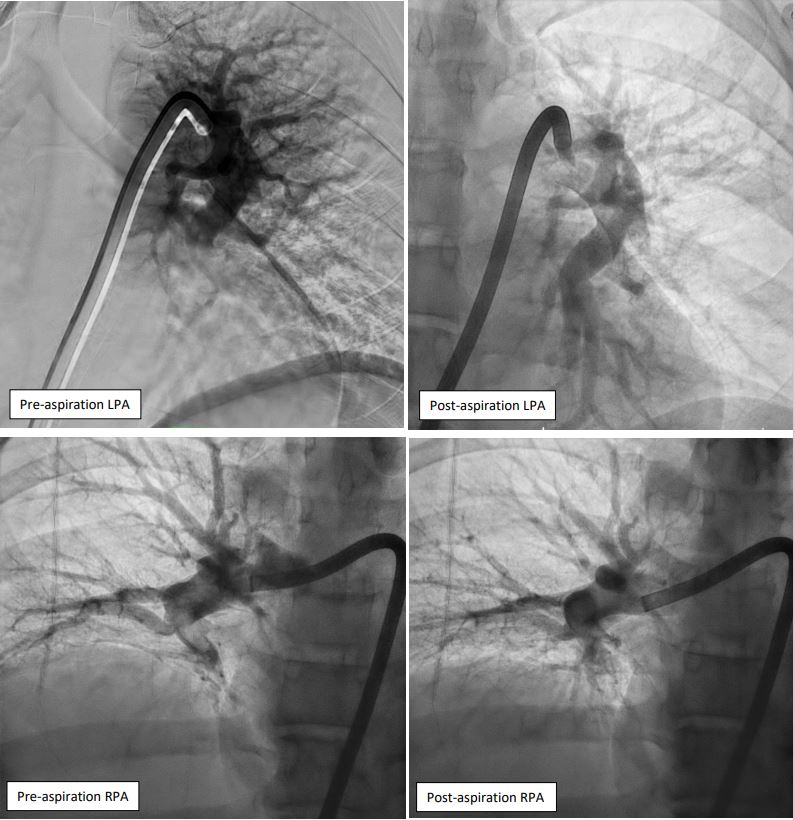


Case Summary
The patient was transferred to the Cardiac Care Unit for close monitoring and continued on parenteral anticoagulation. Less than 12 hours post-procedure, she showed remarkable clinical improvement. Her altered mental status, tachycardia, and tachypnea resolved, and oxygen saturation improved to 99% on room air. A repeat ECHO showed improvement in RV function, with a TAPSE of 1.35 cm and an S' 9.0 cm/s. She was discharged well 5 days later. Intermediate to high risk PE remains a disease with sub-optimal clinical outcomes. Early mechanical thrombectomy should be considered for rapidly deteriorating patients, even in the absence of hemodynamic instability.