Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-171
RSVG Angioplasty for Distal De-Novo Lesion Using Drug Eluting Stent and Proximal ISR Using Drug Coated Balloon in an Elderly Patient With NSTEMI, Post CABG Status With Mild LV Dysfunction and CKD
By Basabendra Choudhury, Jayanta Saha
Presenter
Basabendra Choudhury
Authors
Basabendra Choudhury1, Jayanta Saha2
Affiliation
Fortis Hospital, India1, Medical College Kolkata, India2,
View Study Report
TCTAP C-171
Coronary - DES/BRS/DCB
RSVG Angioplasty for Distal De-Novo Lesion Using Drug Eluting Stent and Proximal ISR Using Drug Coated Balloon in an Elderly Patient With NSTEMI, Post CABG Status With Mild LV Dysfunction and CKD
Basabendra Choudhury1, Jayanta Saha2
Fortis Hospital, India1, Medical College Kolkata, India2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 72 year old male patient, diabetic, CKD ( eGFR45 ml/min) was referred with waxing wanning chest pain for last 6-7 days suggestive of unstable angina.
Hemodynamically stable, no clinical evidence of heart failure.
History of CABG (LIMA to LAD, RSVG to PDA) 14 years back; PTCA and stenting to RSVG to PDA graft following ACS 6 years back.
Serial ECGs showed evidence of inferior MI of uncertain duration, no dynamic changes compared to old ECG.
Rising trop I levels confirmed NSTEMI.
LVEF 48%

Relevant Test Results Prior to Catheterization
Rising troponin I levels over last 12 hours confirmed ACS. Echocardiography suggested LVEF 48-50% with small areas of LV apical and basal inferior, inferoseptal hypokinesiaHb 9.8g%, LDL 76 mg/dl, HbA1c 7.6, eGFR 45ml/minImpression: NSTEMI, old IWMI, mild LV dysfunction, CKD
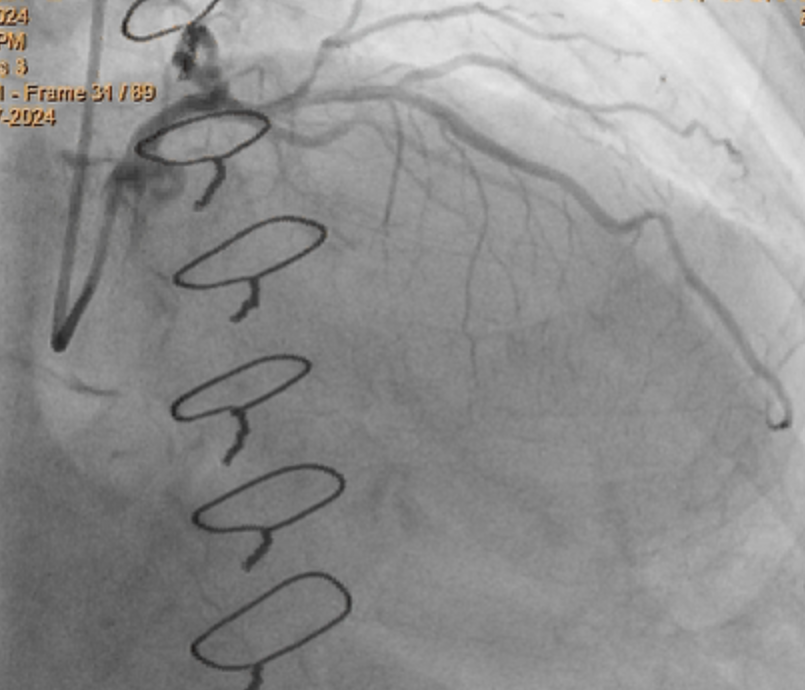
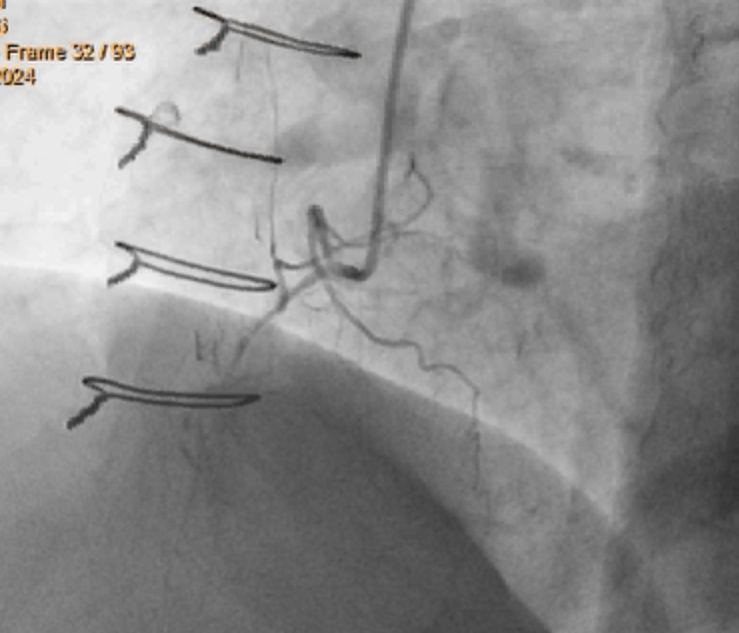
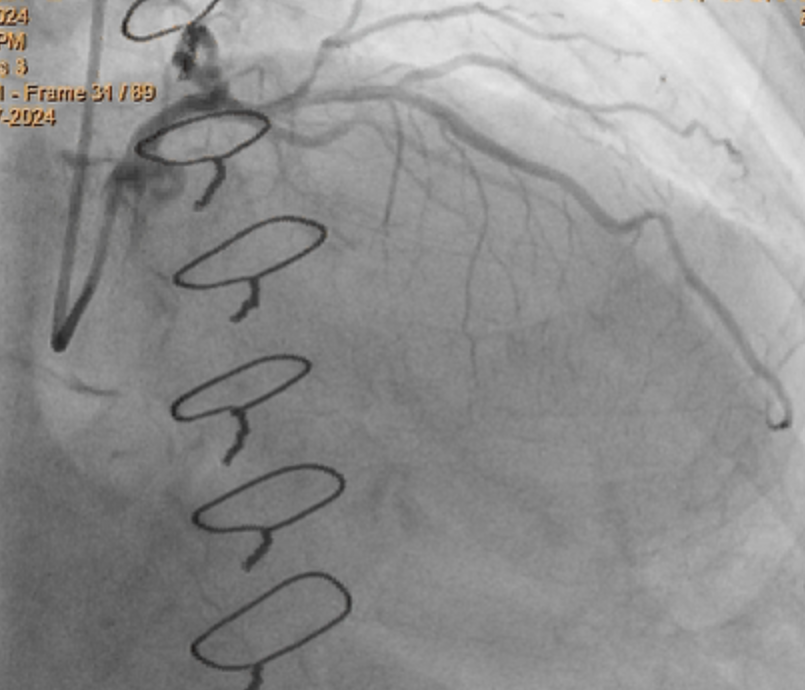
Relevant Catheterization Findings
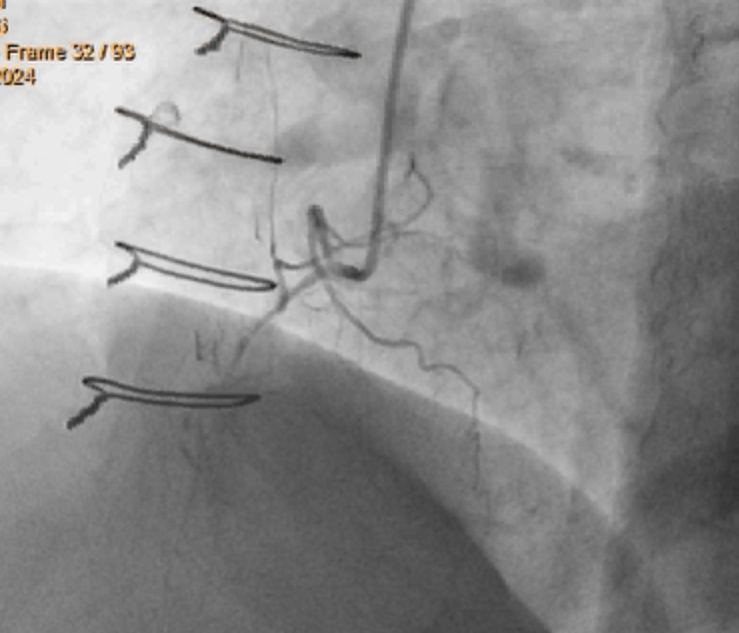
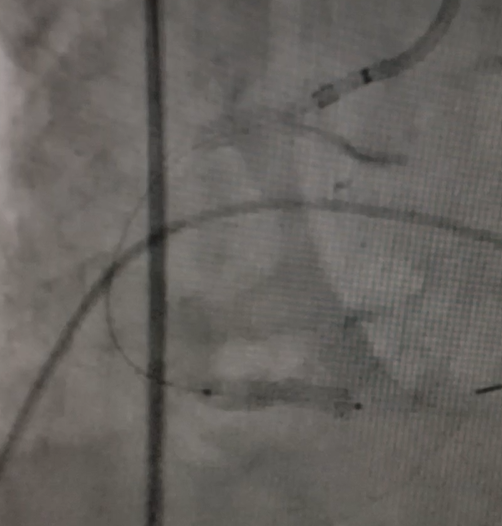
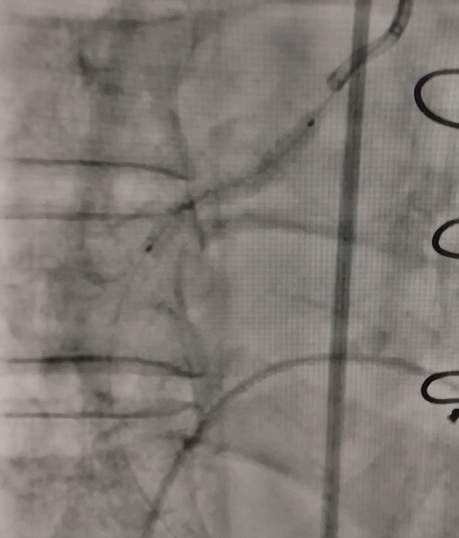
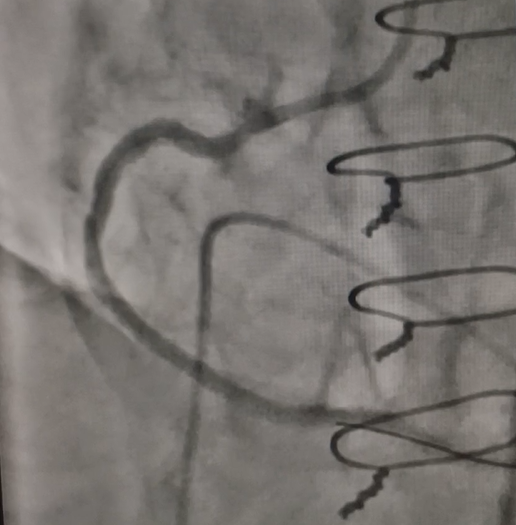
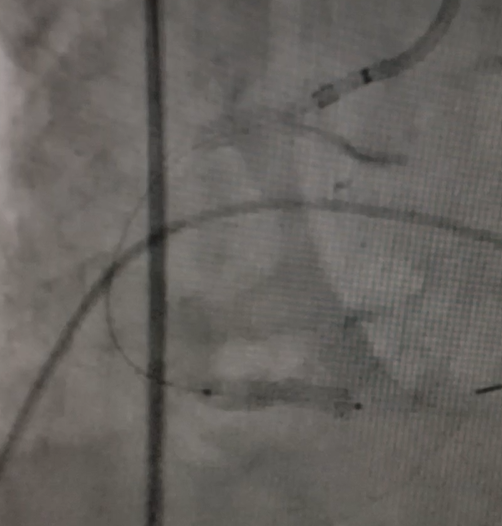
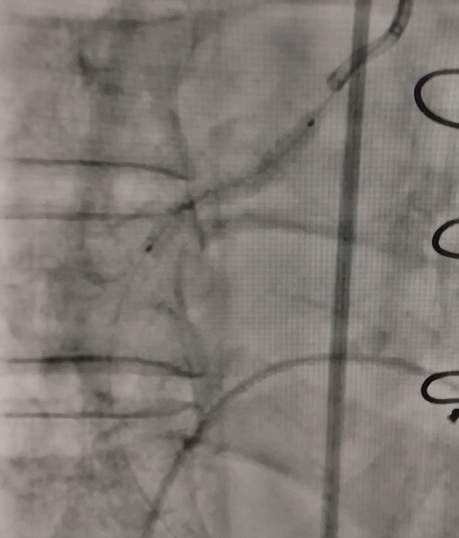
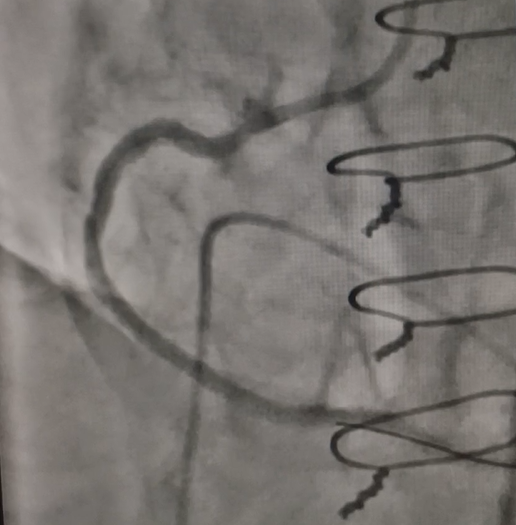
CORONARY AND GRAFT ANGIOGRAPHY (right femoral 7 Fr sheath, 6 Fr JL 3, JR 3.5 and AL1 diagnostic catheters) findings:LMCA minor disease, LAD proximal to mid 50-60-% disease, fair distal flowLCx non-dominant, narrow calibre, proximal 60-70% diseaseRCA dominant, CTO from proximal part, faint retrograde filling from left systemLIMA to LAD graft hypoplasticRSVG to PDA graft showed 80% ISR in proximal part, distal two tandem lesions each 80-90%, compromised distal flow


Interventional Management
Procedural Step
PLAN: PTCA to RSVG to PDA graft in same sitting; Left system to be addressed if symptoms persist/ ischemic burden large in staged procedureLoading with Aspirin 325mg, Ticagrelor 180mgRight femoral, 6 Fr AR1 guide, Runthrough Extrafloppy wire. Serial pre-dilation of distal de-novo and proximal ISR lesions with 2x12 semi-compliant balloon at 12-16 atm prDistal lesion dilated further with 3.25x12 and 3.25x8 non-compliant (NC) balloons at16-22 atm pr. Proximal lesion dilated with 3.25x8 and 3.5x12 NC balloons 20 atm prFair pre-dilation result achieved, small dissection at distal lesion site6Fr guide extension advanced over semi-compliant balloon for safe distal delivery of stent across proximal stent and tortuous graft anatomyUse of DES instead of DCB for distal lesion confirmed due to significant distal dissection3.5X24 DES advanced through old proximal stent and deployed @ 12 atm pr distally and post dilated with 3.5x12 NC balloon at 16-20 atm pr using guide extension support3.5x30 Drug coated balloon (Paclitaxel) inflated over proximal lesion including the ISR region at 8 atm pr for 90 seconds (previous stent 3x24 mm Sirolimus eluting)Good final result. Heparin adjusted to ACT 300 seconds. Contrast: 150 ml VisipaqueImaging missed due to health card issuePatient could be discharged in stable condition after 3 days, LVEF 50%, GFR 43 ml/minClinical follow up after 1 month and 3 months of procedure satisfactory, no angina on daily activities, LVEF 50-52%, LDL 50 mg/dl, HbA1c 7.2
Case Summary
PCI to venous grafts have higher risk of restenosis, CV events compared to native arteriesHigh pressure balloon inflation in venous grafts have higher chances of thrombotic and mechanical complications. Prompt identification and management are essentialRoutine use of filter may not be beneficialTimely use of guide extension for difficult proximal anatomy is helpfulDIVA trial (2018) showed no differences between DES and BMS after 1 year follow-up in treating SVG lesions1 yr follow up by Lin L et al (2023) had similar results between DES and DCB for de-novo SVG lesionsFew case reports (M Rogowski 2024) have used DCB in SVG ISR safely with good short term follow upHigh quality data limited