Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-194
Type 2 Spontaneous Coronary Artery Dissection Involving the Whole Left Coronary Artery Causing Non-ST-Elevation Myocardial Infarction
By Haw-Ting Tai, Feng-Yu Kuo, En-Shao Liu
Presenter
Haw-Ting Tai
Authors
Haw-Ting Tai1, Feng-Yu Kuo1, En-Shao Liu1
Affiliation
Kaohsiung Veterans General Hospital, Taiwan1,
View Study Report
TCTAP C-194
Coronary - Imaging & Physiology - Invasive Imaging (IVUS, OCT, NIRS, VH, etc)
Type 2 Spontaneous Coronary Artery Dissection Involving the Whole Left Coronary Artery Causing Non-ST-Elevation Myocardial Infarction
Haw-Ting Tai1, Feng-Yu Kuo1, En-Shao Liu1
Kaohsiung Veterans General Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
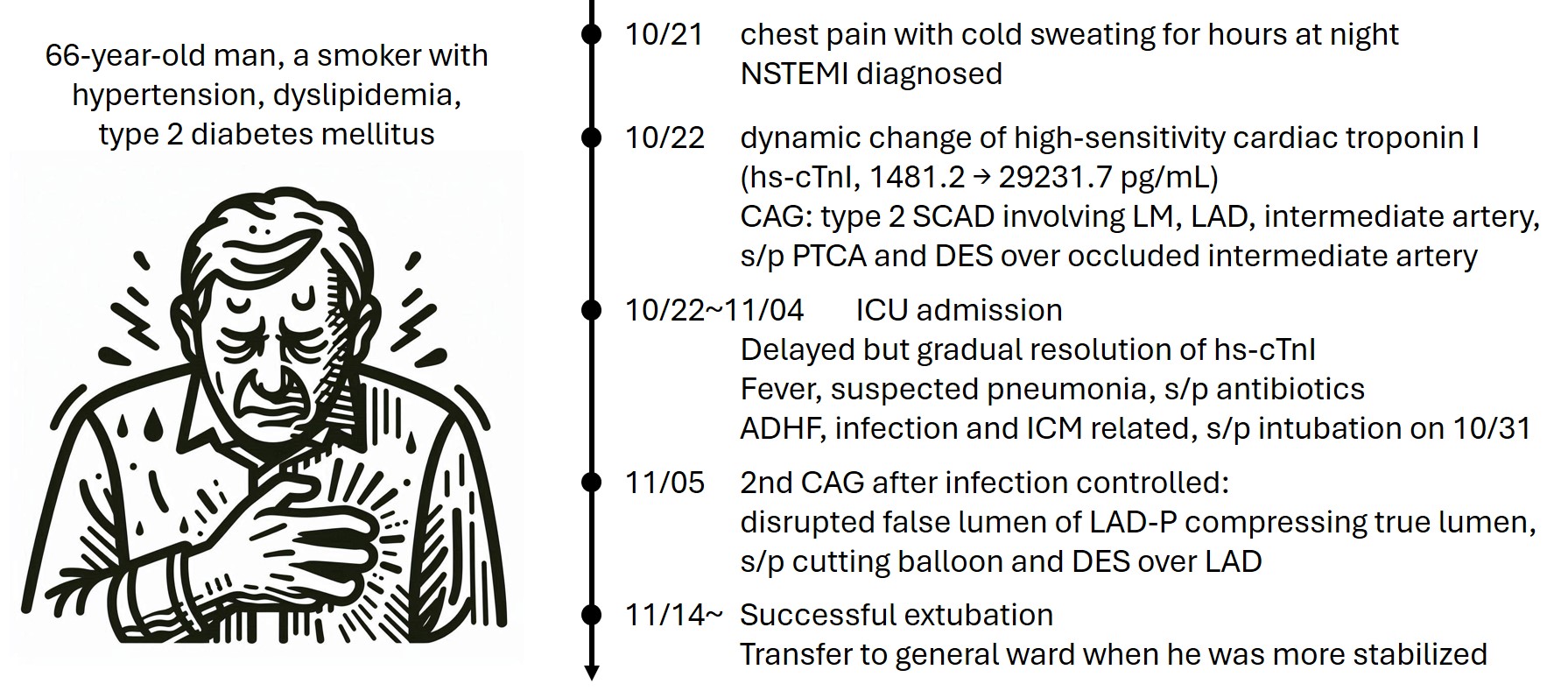
A 66-year-old man was a smoker with underlying hypertension, dyslipidemia and type 2 diabetes mellitus. He suffered from sudden onset of chest tightness with cold sweating for hours prior to his visit to emergency department (ED). At triage, he was conscious with hypertension to 177/109 mmHg. Physical examination showed clear breathing sounds and regular heart beats without significant murmur. Non-ST-elevation myocardial infarction was diagnosed, and coronary angiography (CAG) was performed.
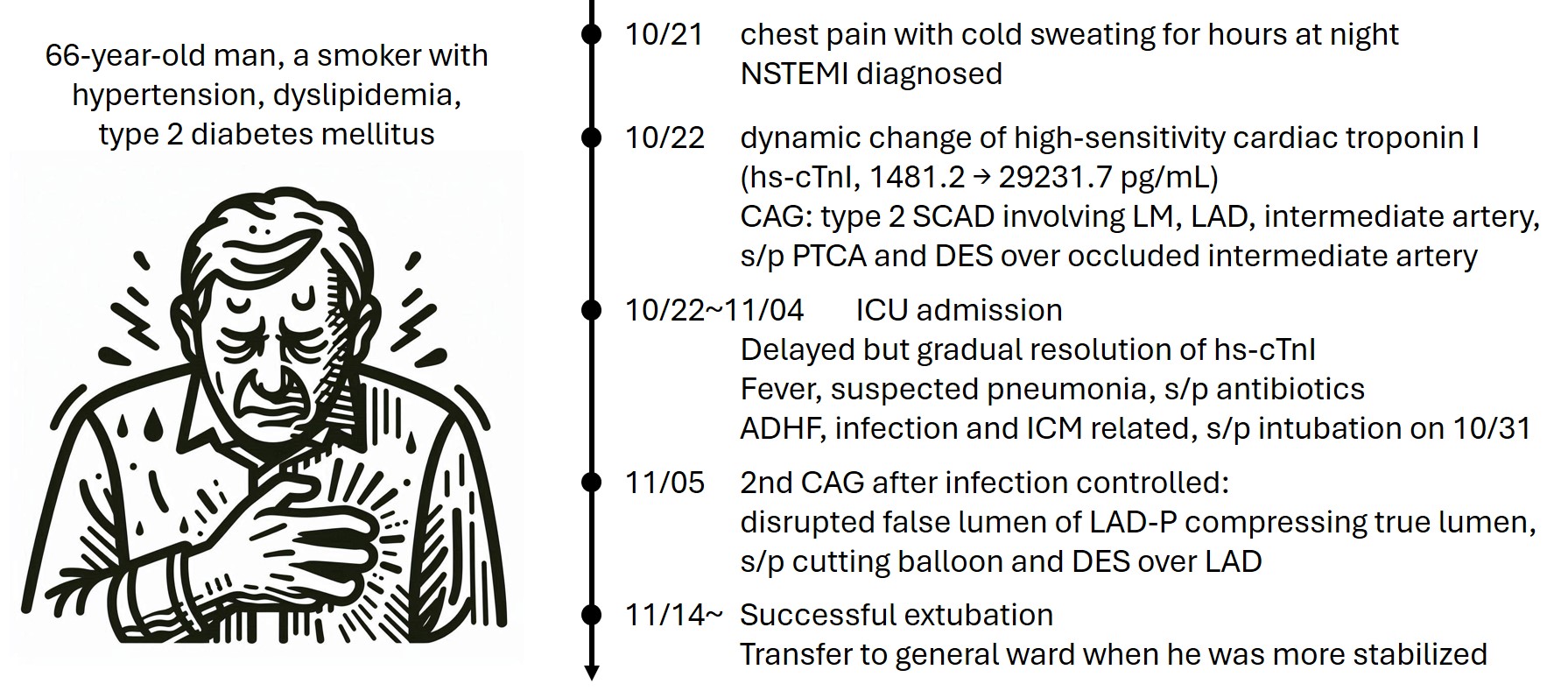
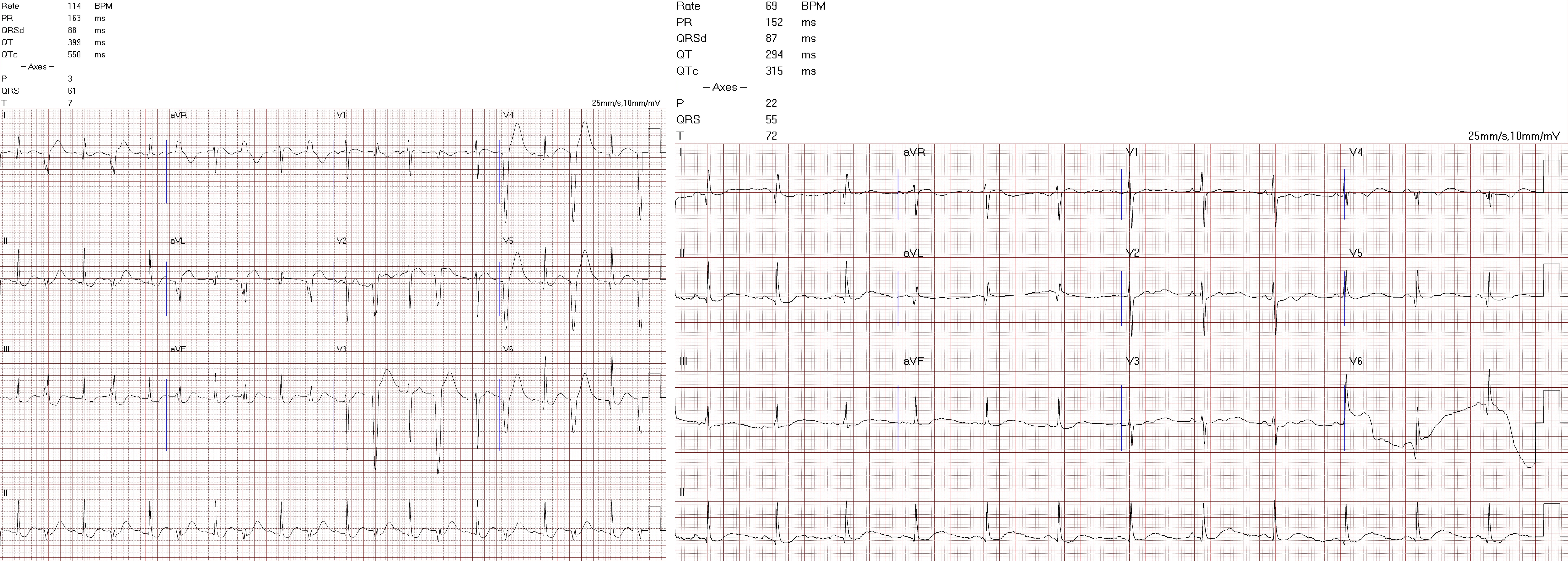
Relevant Test Results Prior to Catheterization
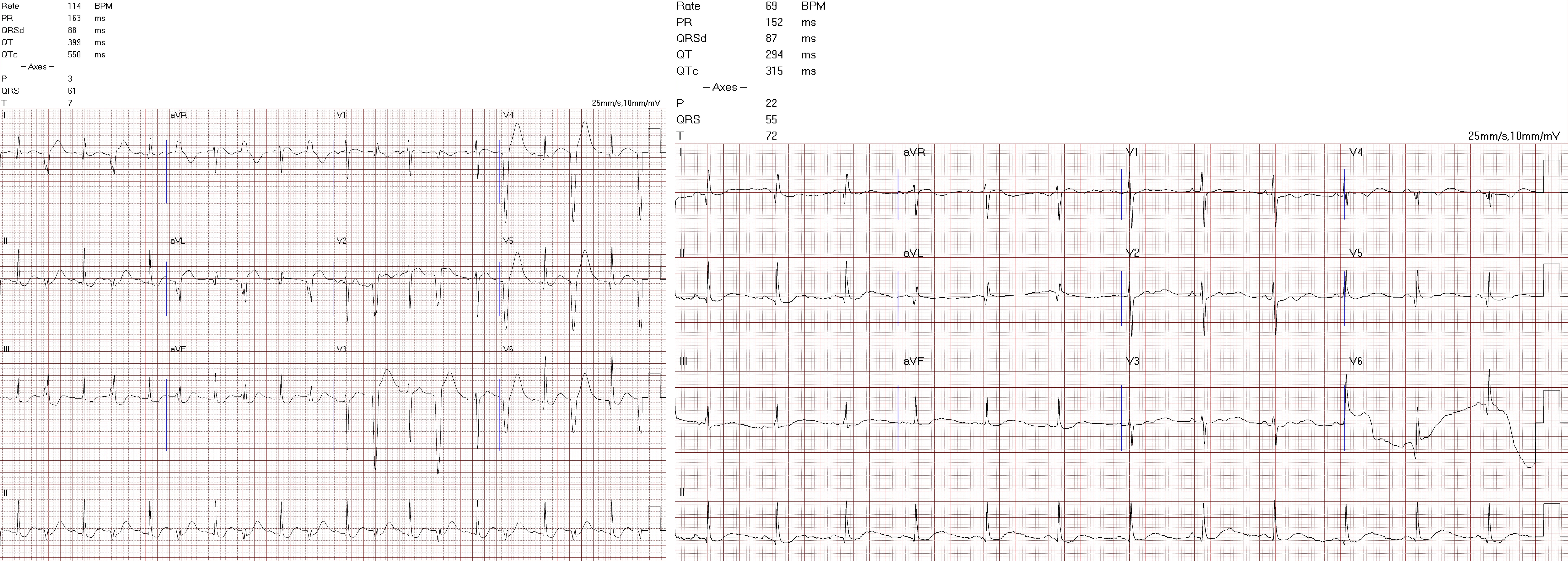
At ED, serial electrocardiographies showed bigeminal premature ventricular contractions at first and recovered to normal sinus rhythm in the followed study, with no significant elevation or depression of ST segment. Chest radiography showed no cardiomegaly or significant lesion. Laboratory tests showed significant elevation of cardiac enzymes, particularly high-sensitivity troponin I (hs-cTnI) from 1481.2 to 29231.7 pg/ml, despite antithrombotic therapy.


Relevant Catheterization Findings
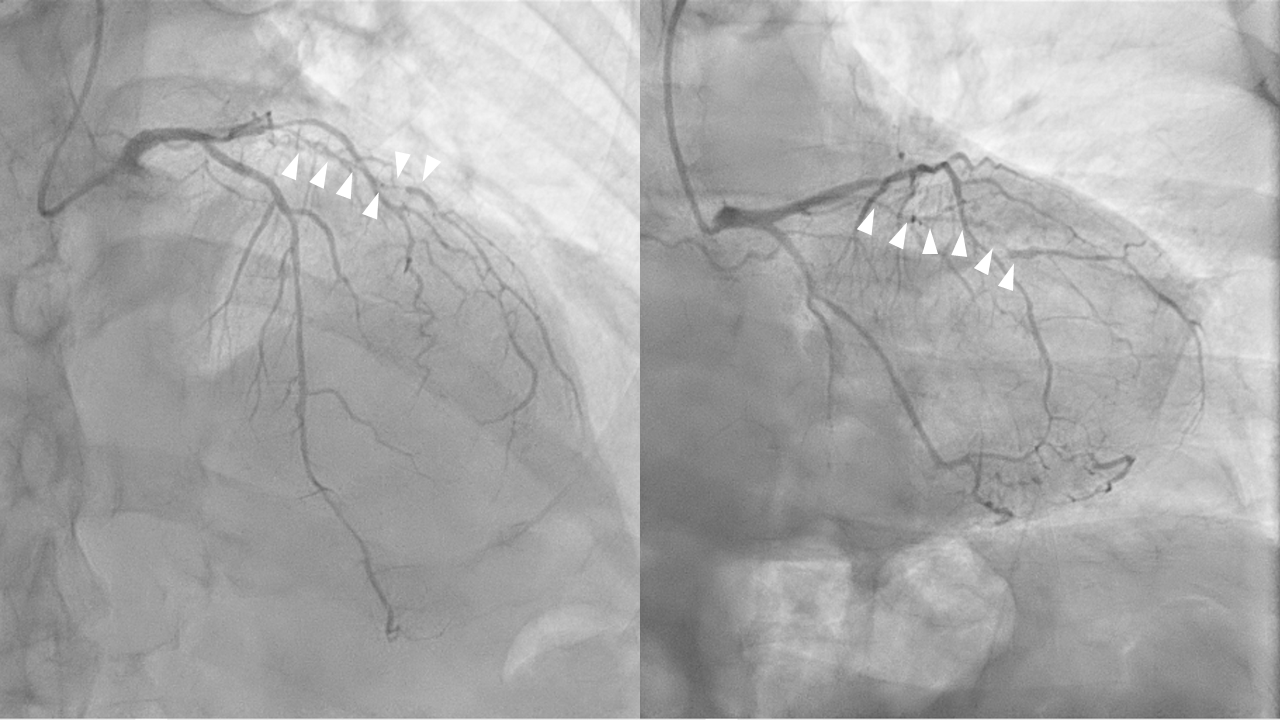
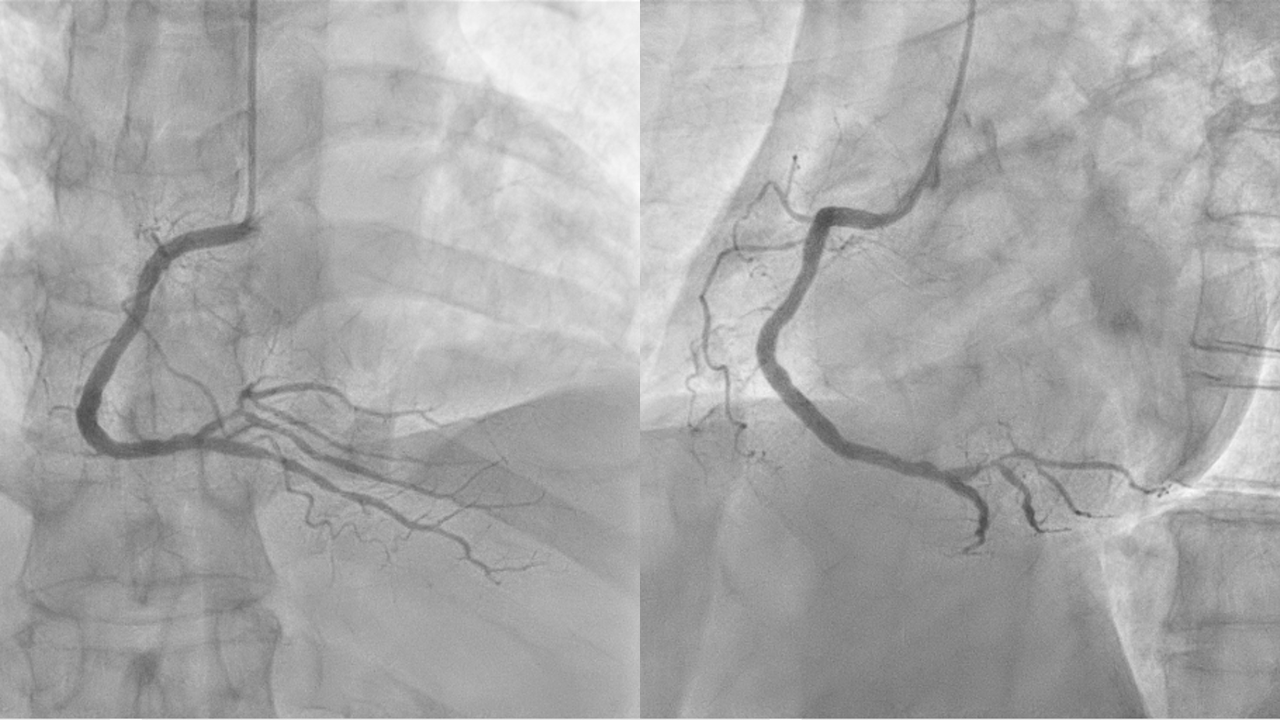
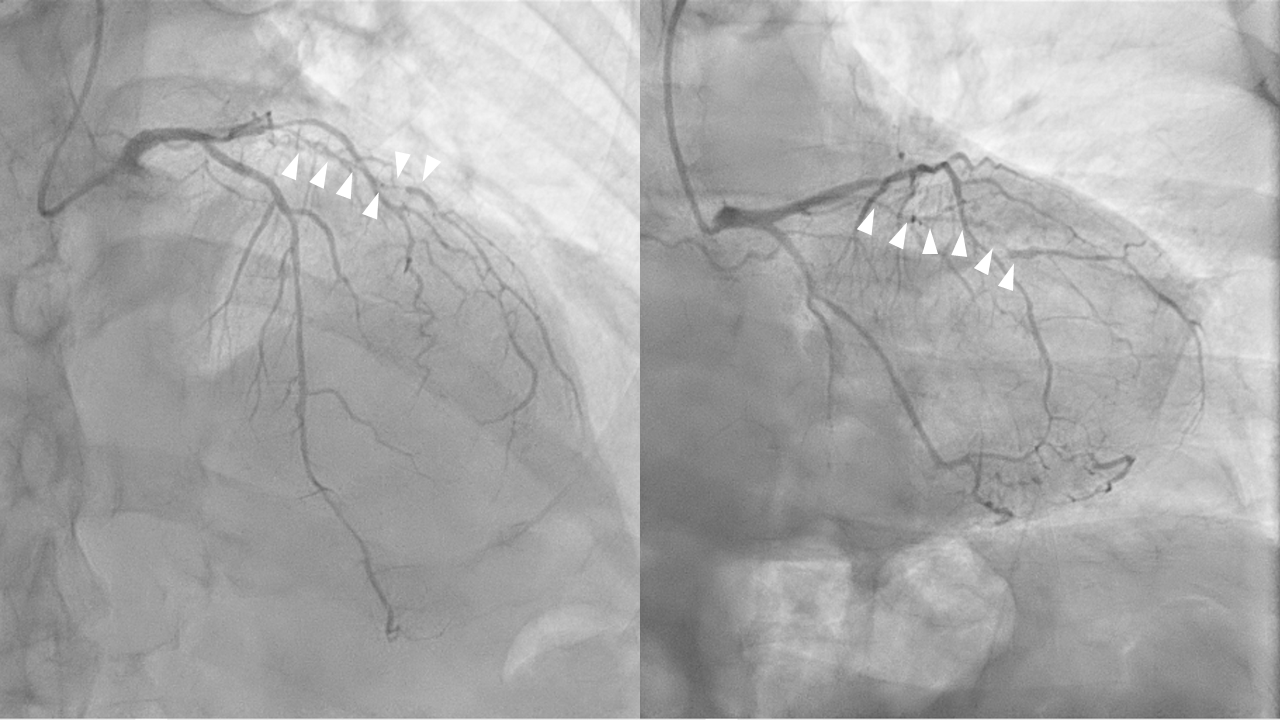
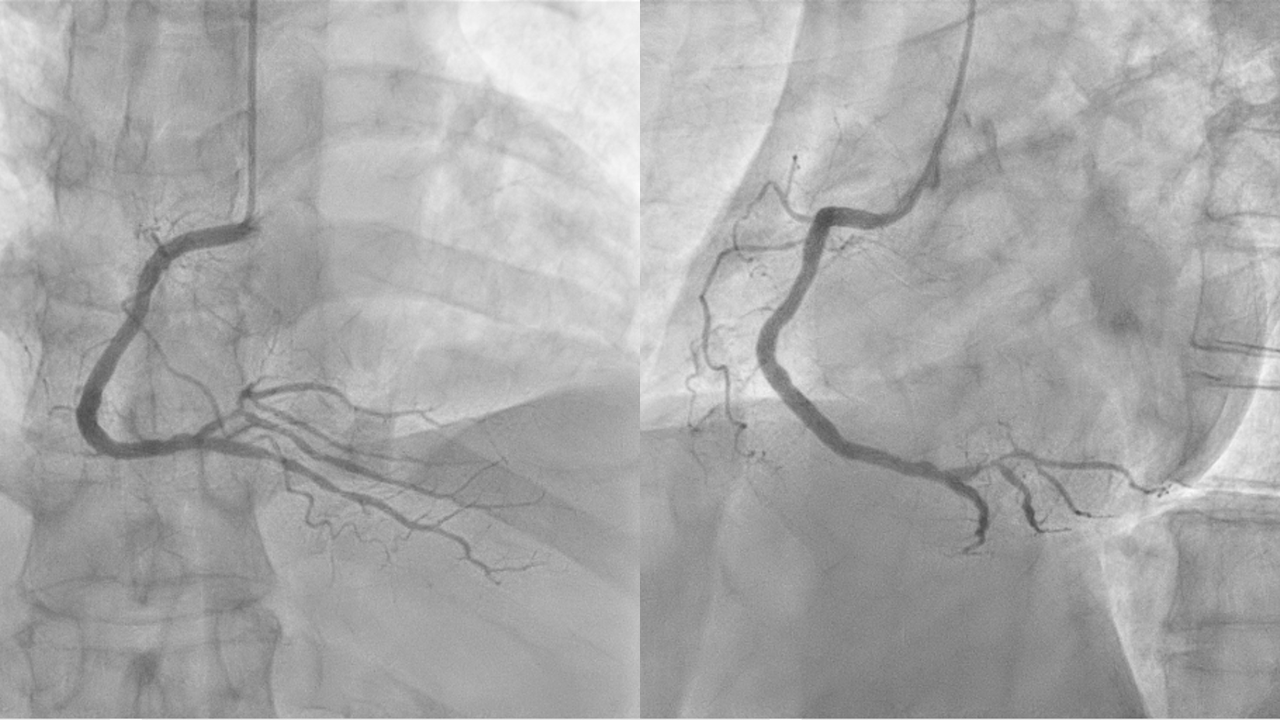
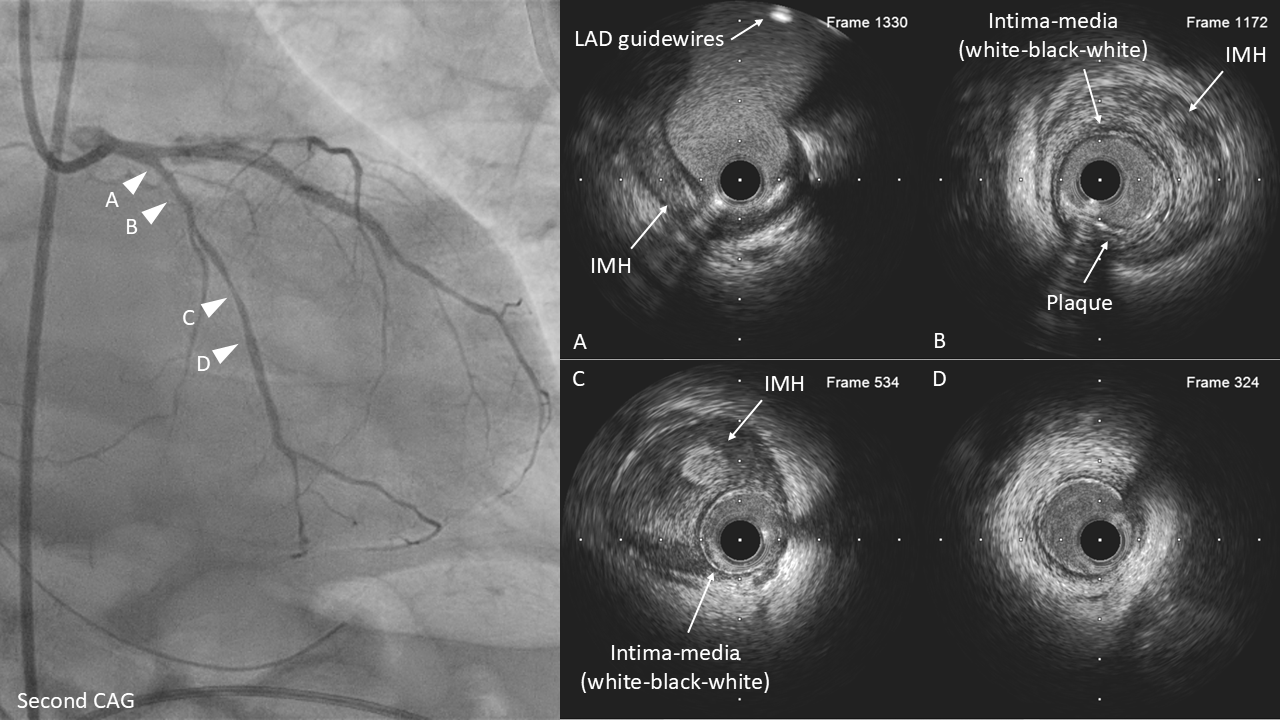
CAG showed diffuse luminal narrowing over left circumflex artery (LCX), left anterior descending artery (LAD), and the first diagonal branch (D1), which was almost occluded and considered as the cultprit lesion. There was also luminal irregularity of right coronary artery (RCA) and focal stenosis over posterior descending artery (PDA) and posterior left ventricular artery (PLV).
Interventional Management
Procedural Step
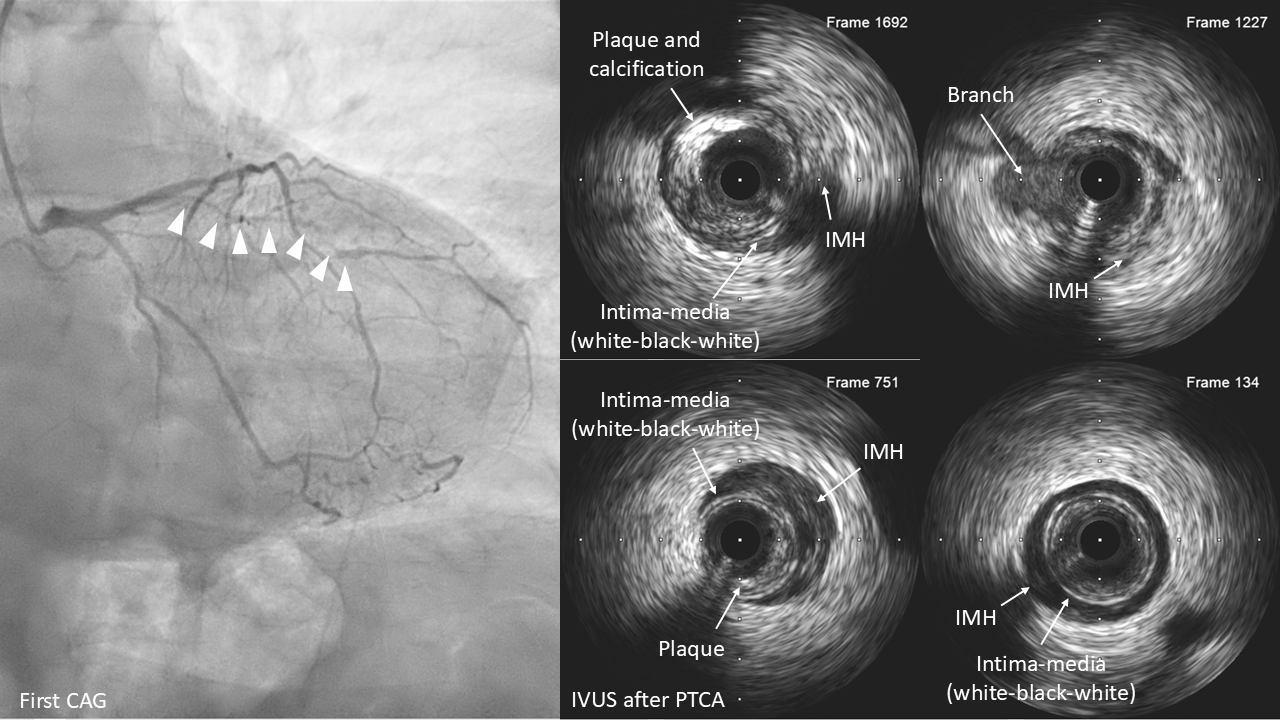
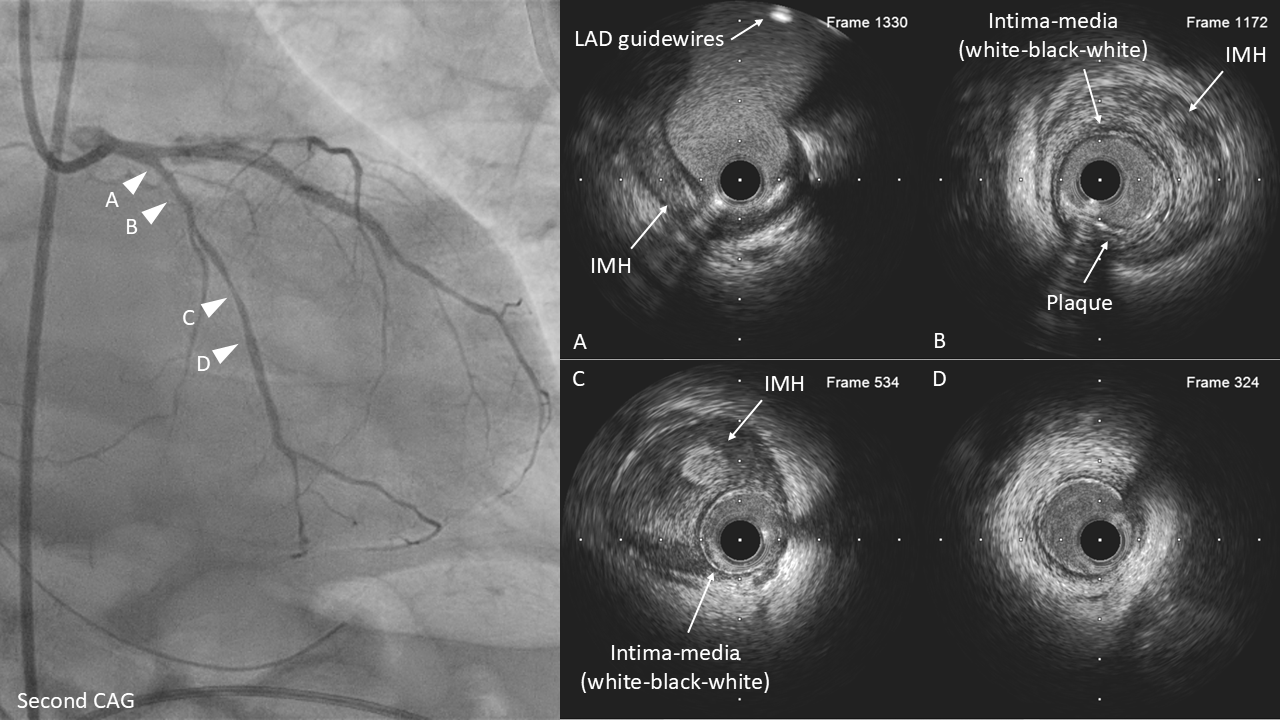
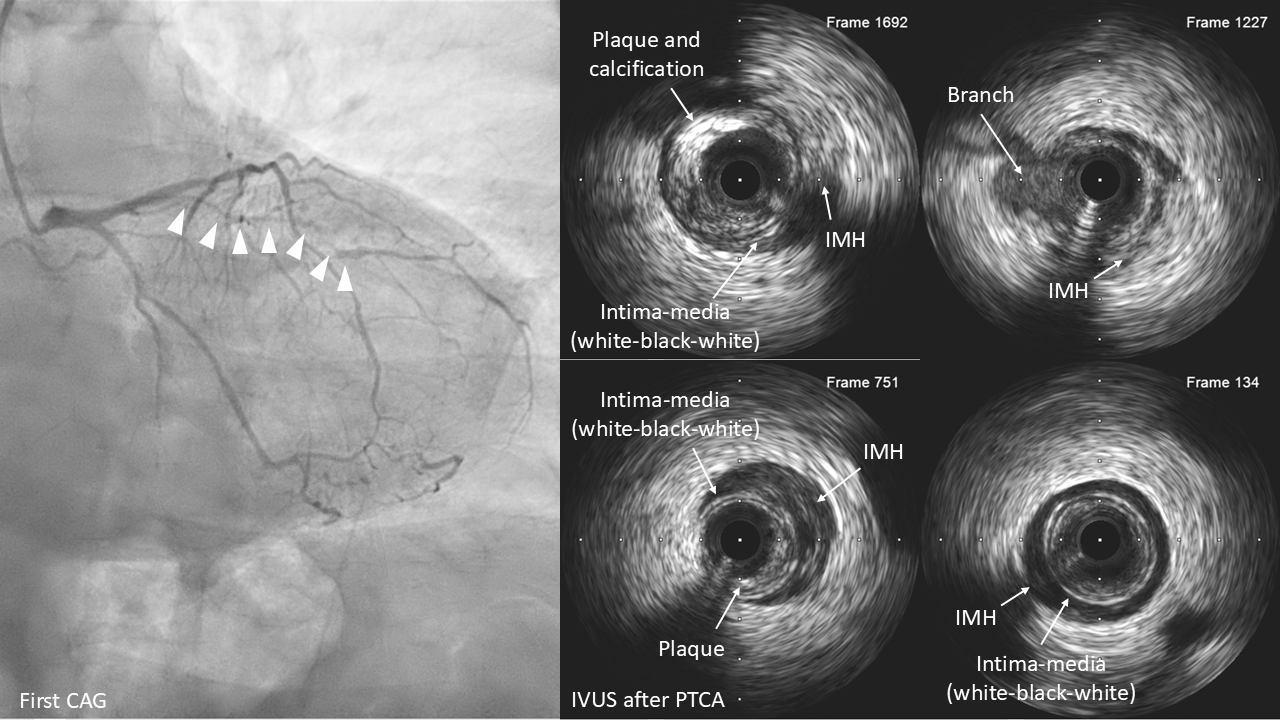
Percutaneous transluminal coronary angioplasty (PTCA) and stenting with drug-eluting stents (DESs) were performed smoothly over PLV.Then, we engaged left coronary artery with 6 French EBU guide catheter and carefully wired through the critical stenosis of D1. Intravascular ultrasound (IVUS) performed after PTCA over D1 with a 2.0mm balloon showed the guidewire all within the true lumen, and diffuse intramural hemotoma (IMH), favored type 2 spontaneous coronary artery dissection (SCAD), were noted from the ostium to distal segment, and DESs were placed. IVUS in LAD also showed diffuse IMH from the ostial to distal LAD, with TIMI grade 3 flow in the angiogram.Delayed resolution of hs-cTnI was noted after the patient admitted to ICU, with relapsed chest pain complained. Therefore, CAG was repeated and showed patent stents in D1 but contrast stasis in the subintimal space of proximal LAD. IVUS then revealed disrupted IMH involving left main coronary artery (LM) revealed, and the true lumen of LAD was compressed by the false lumen with impaired coronary flow. Angioplasty with 3.0mm cutting balloon was performed and successfully created fenestrations over the distal end of the false lumen, and DESs were placed from the ostial to distal LAD. IVUS also showed diffuse IMH, also favored type 2 SCAD, from the ostium to distal LCX without impairing coronary flow.


Case Summary
SCAD is uncommon and often presents as acute coronary syndrome. The diagnosis and classification usually depend on the CAG with intracoronary imaging using IVUS or optical coherence tomography (OCT).The goal of management is to preserve myocardial perfusion, and conservative medical therapy is preferred in stable patients. However, revasularization would be necessary in unstable patients or when SCAD involves the LM and / or proximal LAD, LCX or RCA.PCI for SCAD is relatively difficult with technical challenges and increased rates of complications. Besides using IVUS or OCT, the use of a floppy wire and cutting balloon, and multi-stent approach to prevent hematoma extension should be considered.