Coronary - Complex PCI - Bifurcation
A Case of Assessing the Risk of Side Branch Occlusion and Lesion Modification by Debulking Were Useful in the PCI of Bifurcation Lesion With an Eccentric, Highly Calcified Lesion
Takeru Kasama1, Kazuki Hasegawa1, Takayuki Senba1, Keisuke Nakashima1, Kei Kawai1, Takayuki Shinmura1, Kazuhiro Ashida1
Seirei Yokohama Hospital, Japan1,
A 70-year-old man with a history of hypertension, diabetes, and dyslipidemia was admitted for coronary angiography and revascularization due to severe stenosis of the Left Anterior Descending artery(LAD) identified on pre-procedural CTA for catheter ablation of atrial fibrilation. No significant abnormalities were noted in the preoperative physical examination and the ECG, and had no renal impairment.
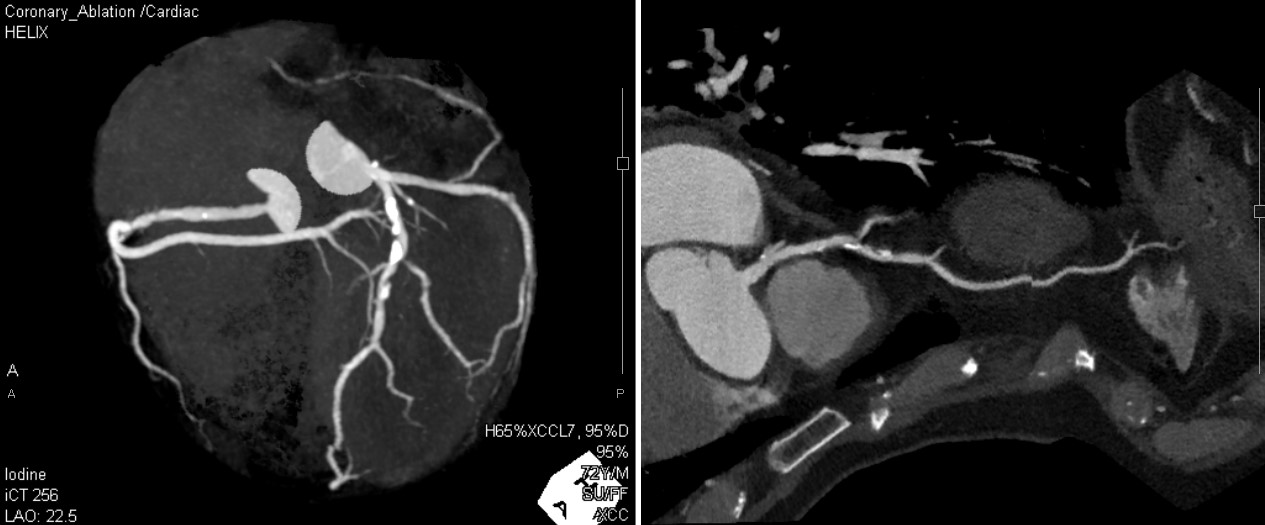
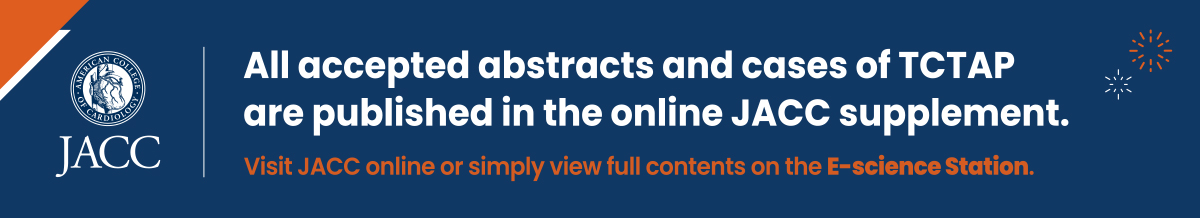
Coronary CTA suggested severe stenosis in the LAD branch with a diagonal branch that has a wide perfusion area, and there was a calcified lesion on the opposite side of the diagonal branch.
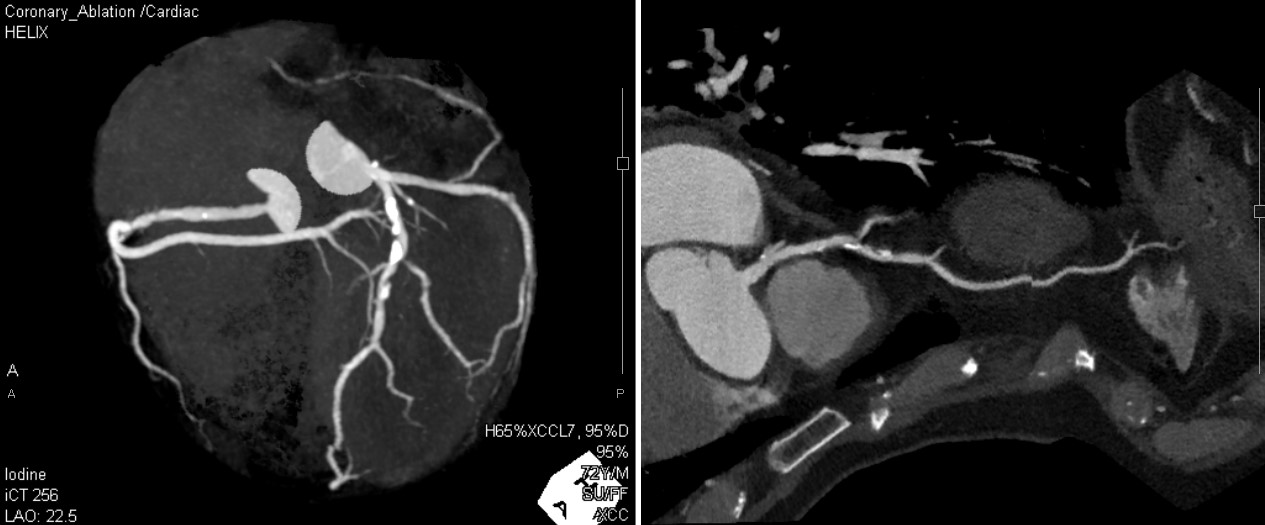
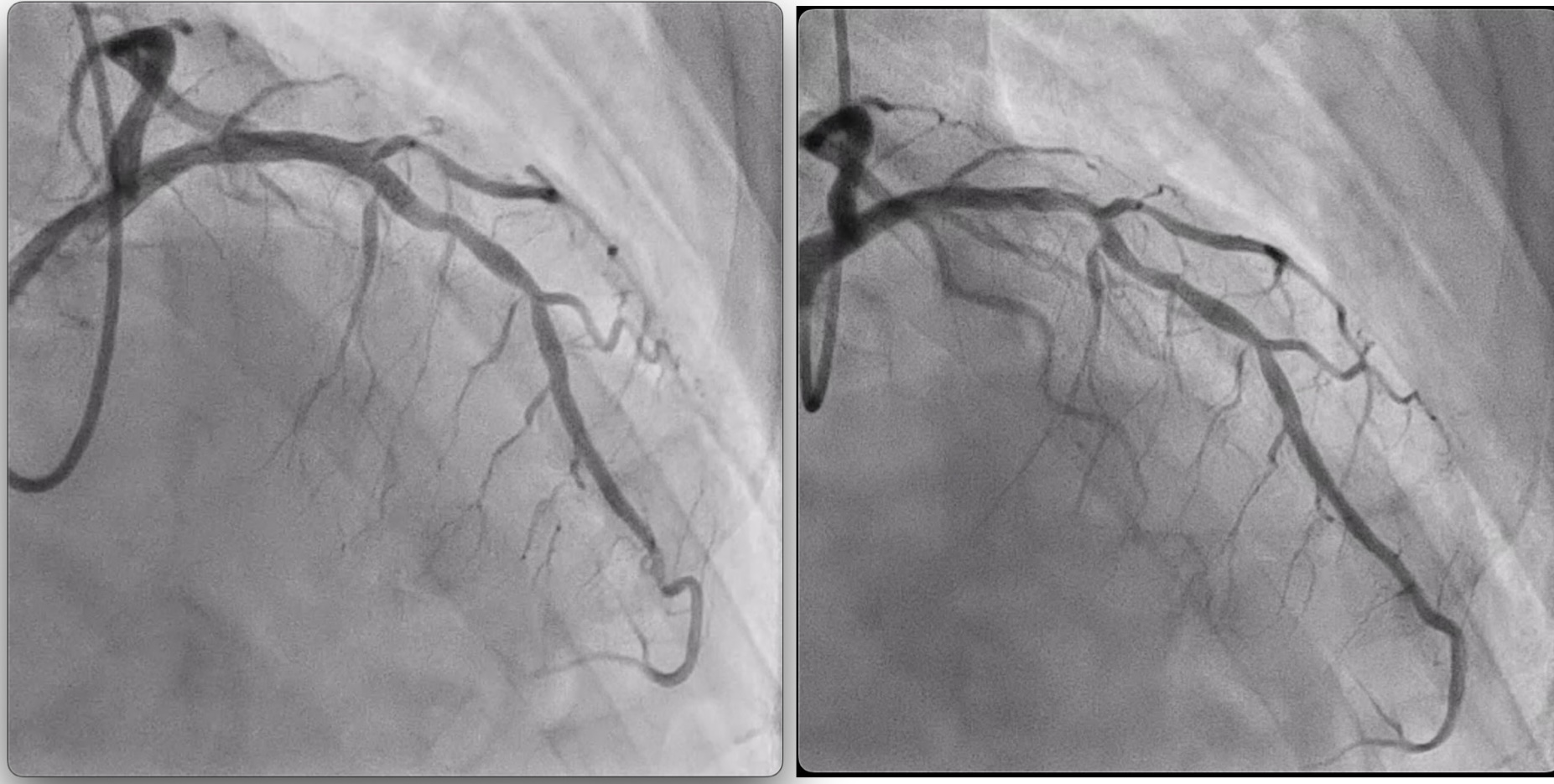
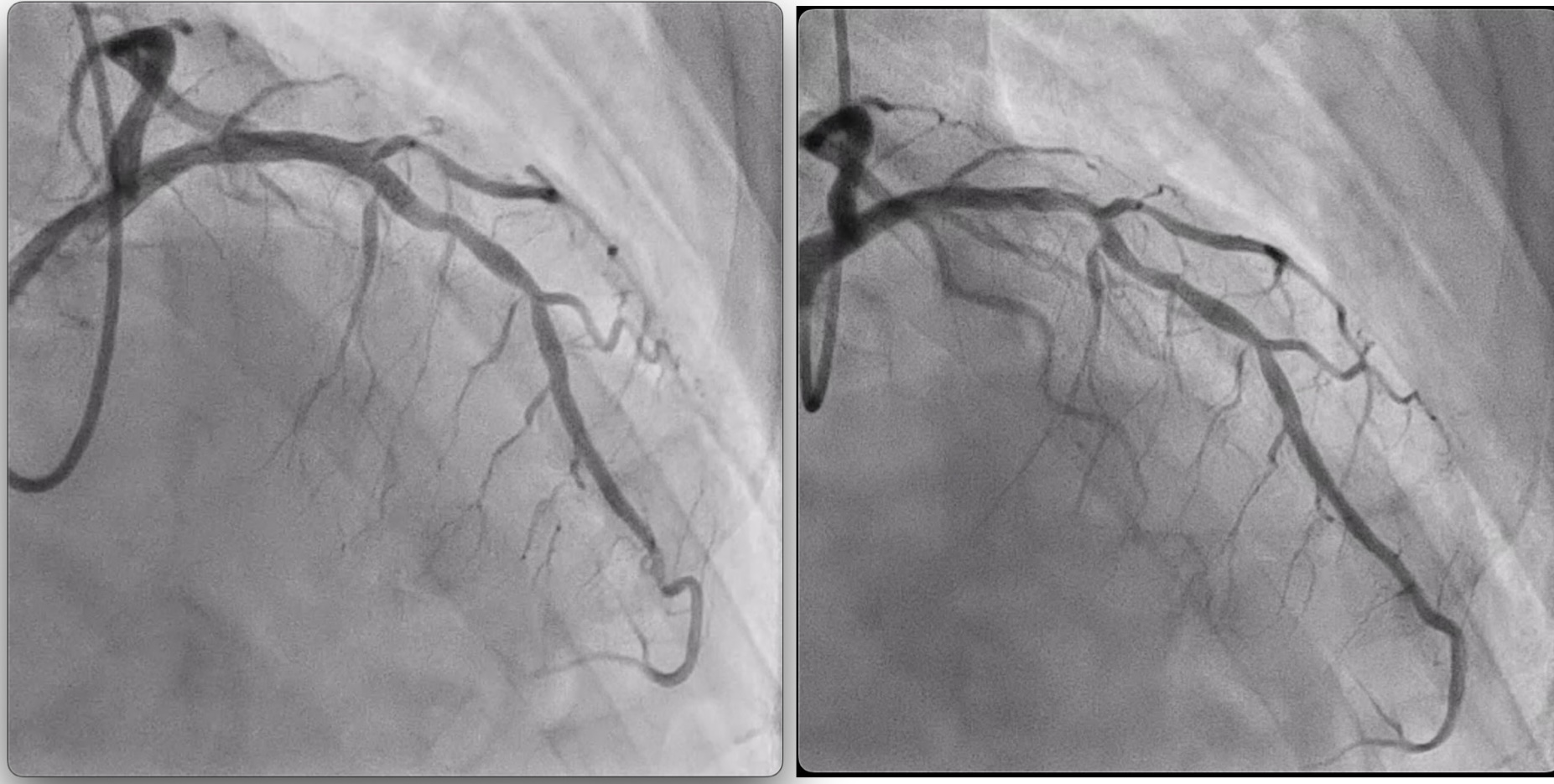
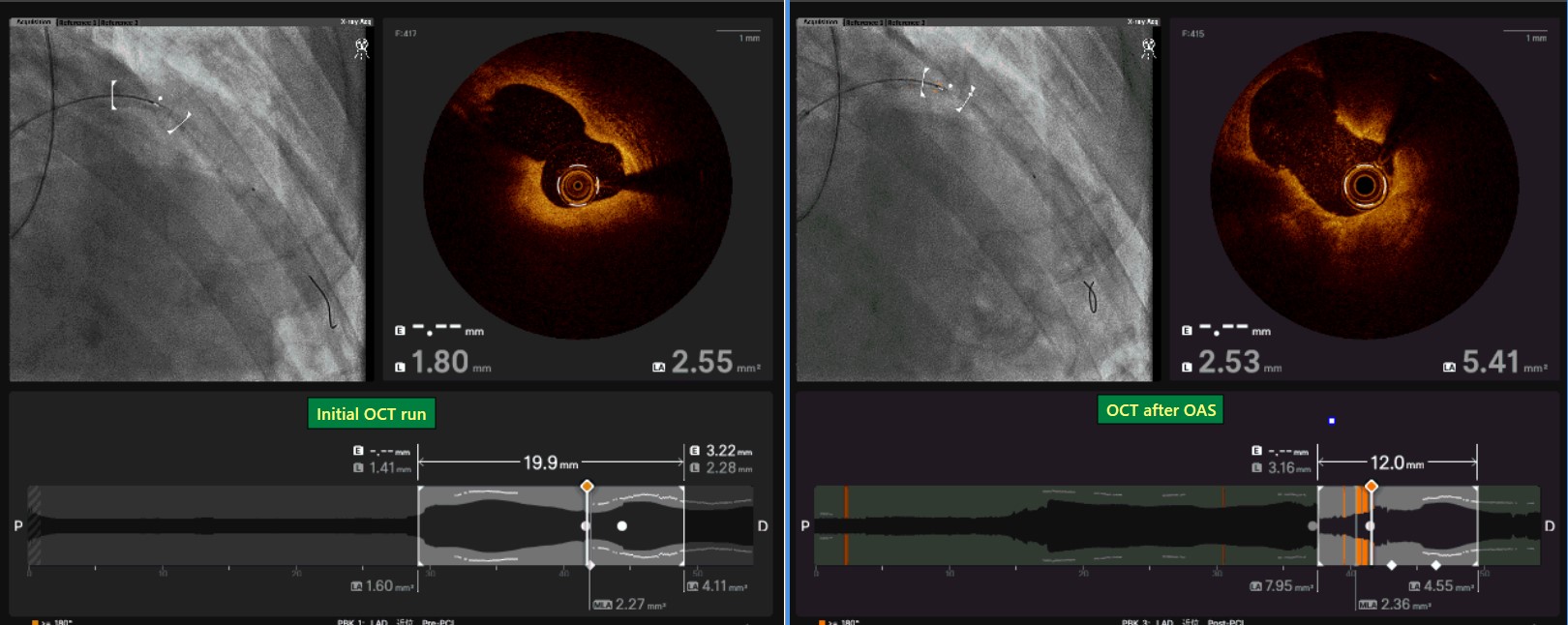
CAG was performed via radial artery, revealing 90% stenosis in the mid-LAD, consistent with pre-procedural CTA findings. IVUS/OCT evaluation showed a prominent calcified lesion in the LAD contralateral to the Diagonal branch, raising the possibility of carina shifting during stent placement.Based on the guidewire bias and lesion length, we decided to perform lesion modification by orbital atherectomy. After executing multiple rounds of sanding cycles at both low speed and high speed, OCT confirmed volume reduction of the calcified lesions.Folowing pre-dilation with a scoring baloon, DCB treatment was applied to the diagonal branch. When Pre-Kissing Baloon Inflation(KBI) was performed on the LAD and D1, the baloon in the LAD was able to expand without causing indentation in the lesser curvature side of the vessel with calcification. Based on this result, we considered that the likelihood of carina shift associated with stent placement was low. So we deployed a DES in the LAD and performed KBI on LAD and D1 again. Final angiography demonstrated good antegrade blood flow in both the Diagonal branch and the main LAD, concluding the procedure.
It is wel known that the presence of a coronary bifurcation lesion in conjunction with side-branch occlusion during PCI can be a prognostic factor for cardiovascular events. In this case, we report on the prevention of side-branch occlusion by lesion modification prior to stenting, since side-branch occlusion was predicted due to calcified lesions on the contralateral side of the side branch.