Structural - Aortic Valve Intervention - Coronary Artery Protection / Access
In Doubt of High-Risk Noncardiac Surgery Following Percutaneous Coronary Intervention (PCI) and Transcatheter Aortic Valve Replacement (TAVR): When Is the Best Time?
Apichat Jansillapakorn1, Kittipong Youpaniad1, Anuruck Jeamanukoolkit1, Wasant Soonfuang1, Sukhum Tachasakunjaroen1, Sakolwat Montrivade1
Police General Hospital, Thailand1,
A Thai 85-year-old woman with history of prior myocardial infarction, AF, type 2 DM, HTN and DLP, presented with a 5-month history of exertional dyspnea. Physical examination revealed fine crepitations in both lower lung fields, irregularly irregular with lower volume of carotid pulse and grade 3 systolic ejection murmur at right upper parasternal border with sign of left ventricular hypertrophy.
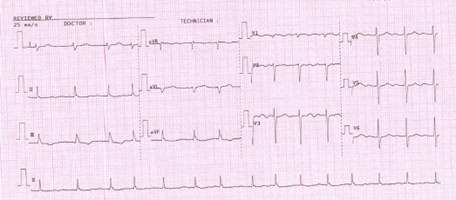

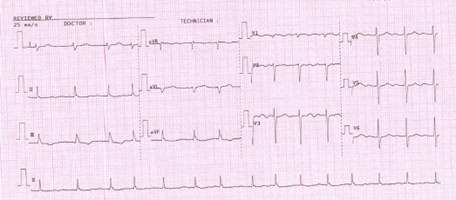
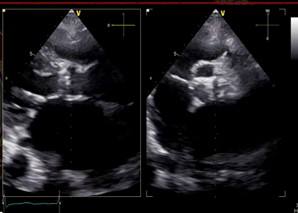
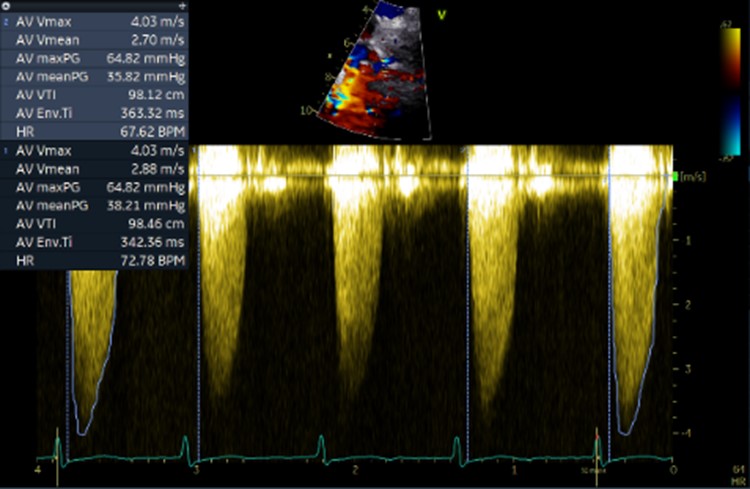
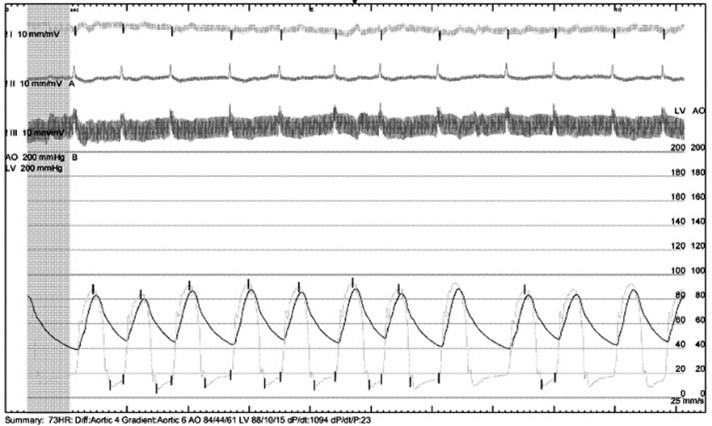
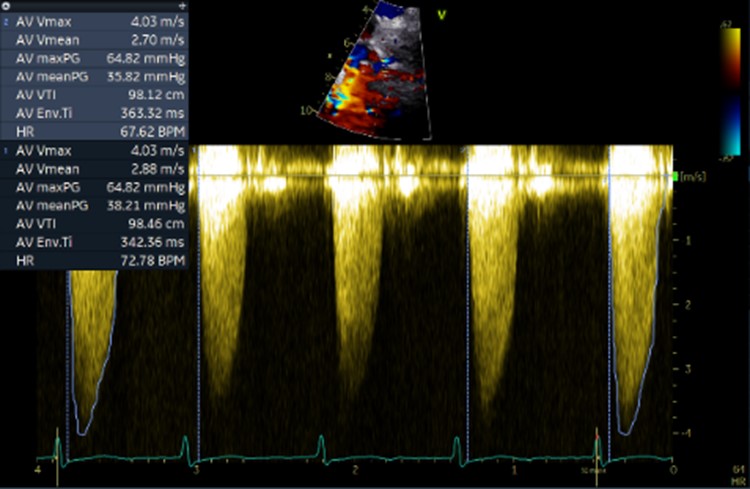
Initial ECG revealed AF. Transthoracic echocardiography revealed concentric LVH with a 70 % of left ventricular systolic function, normal right ventricular systolic function, bi-atrial enlargement and severe calcific aortic stenosis which classified as stage D1 (AVA 0.98 cm
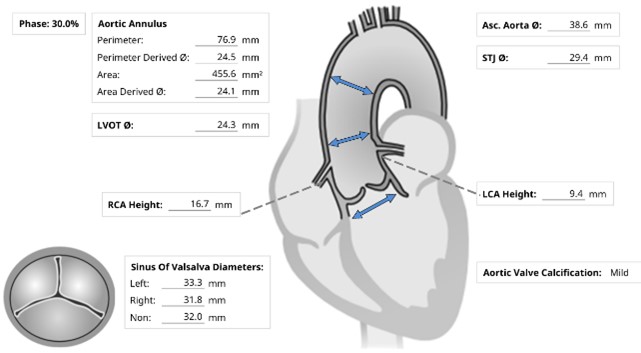
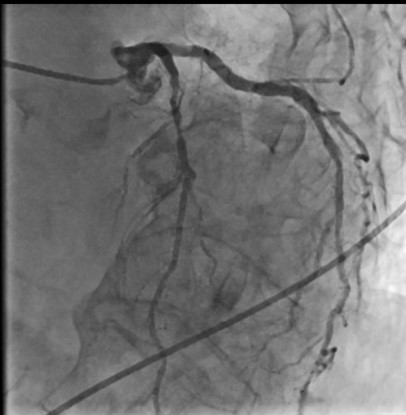
2 by AV VTI, AV Vmax 4.03 m/s, mean AV pressure gradient 38.21 mmHg). Following as the Heart Team discussion, Transcatheter Aortic Replacement (TAVR) following coronary angiography (CAG) was scheduled as the optimal choice.
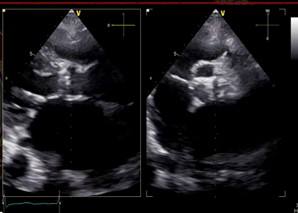
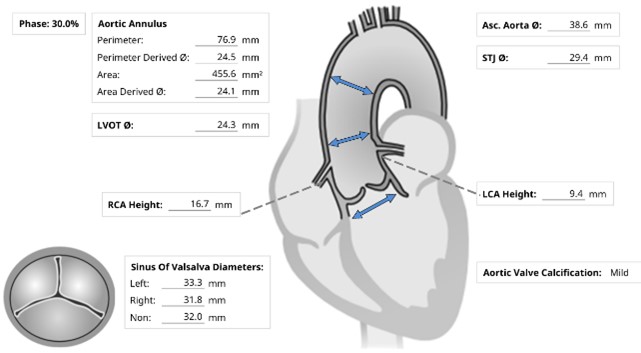
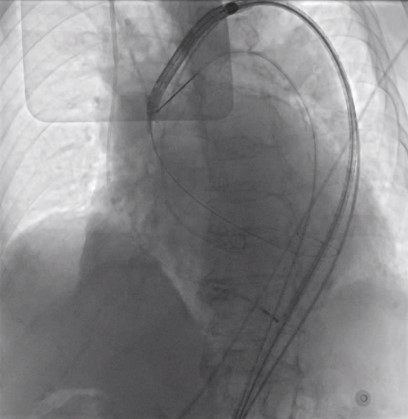
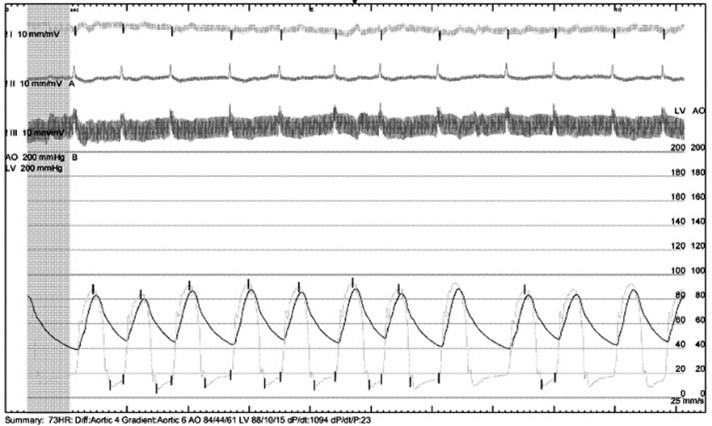
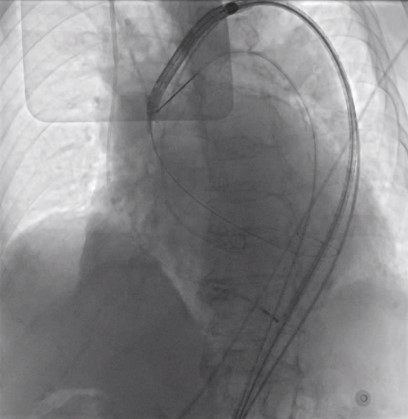
Under local anesthesia and conscious sedation, femoral arteries (FA) were accessed by 8-Fr sheath at right FA and two of 8-Fr sheaths at left FA for pigtail catheter and snare-assisted device. Aortography was conducted by pigtail catheter to locate aortic cusp. An Amplatz left catheter over a 0.035-inchJ-tip wire was placed at aortic cusp via the RFA which was then exchanged with an Amplatz Super Stiff wire to upsized 16-Fr Braidin sheath. The aortic valve was crossed with an Amplatz left catheter over a straight-tip wire under cuspoverlap views (LAO16, CAU 30), peak-to-peak gradient of 19 mmHg. During RV pacing, a Safari Extra Small guidewirewas positioned in LV and the AV was pre-dilated by an 18 × 40 mm Alwide balloon. Subsequently, a 27 mm VitaFlow valve was deployed in an optimal position under snare-assisted. Post-deployment aortography revealed mild AR, LVEDP of20 mmHg, and 4 mmHg of LVOT gradient. Post-dilation was performed by a 24 × 40mm VACC III balloon. The FA was closed by 6-Fr Proglide at the right and 8-Fr AngioSeal at the left. Post-TAVR TEE showed mild PVL without significant transvalvular gradient and preserved LVEF of 64%. One-month after the TAVR, she was diagnosed with early-stage colonic cancer. A laparoscopic hemicolectomy which completed pre-operative evaluation, coronary revascularization, TAVR and appropriated medication was performed as time-sensitive surgery following by CMT with curative intent.