Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-023
Lifeline Hanging by a Thread
By Md Mohasin Uddin, Mahbubor Rahman, Shiblee Sadik Pathan, Md Asifudduza Asif, Rashiduz Zaman, Rakibul Hassan, Md Noor Nabi Khondaker
Presenter
Md Mohasin Uddin
Authors
Md Mohasin Uddin1, Mahbubor Rahman1, Shiblee Sadik Pathan1, Md Asifudduza Asif1, Rashiduz Zaman1, Rakibul Hassan1, Md Noor Nabi Khondaker2
Affiliation
Labaid Cardiac Hospital, Bangladesh1, Combined Military Hospital, Bangladesh2,
View Study Report
TCTAP C-023
Coronary - ACS/AMI
Lifeline Hanging by a Thread
Md Mohasin Uddin1, Mahbubor Rahman1, Shiblee Sadik Pathan1, Md Asifudduza Asif1, Rashiduz Zaman1, Rakibul Hassan1, Md Noor Nabi Khondaker2
Labaid Cardiac Hospital, Bangladesh1, Combined Military Hospital, Bangladesh2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
Mr. Y a 55 year old gentleman presented at emergency department with complaints of sudden onset of severe chest pain for 10 hours with SOB. He also complains of exertional dyspnea for 1 month.Risk factors are Smoker, Hypertension , Dyslipidemia.On admission BP 100/70mmhg, P 102, SpO2 97% with 5L O2.Precordium examination: NAD. There are B/L basal crepitation on auscultation.
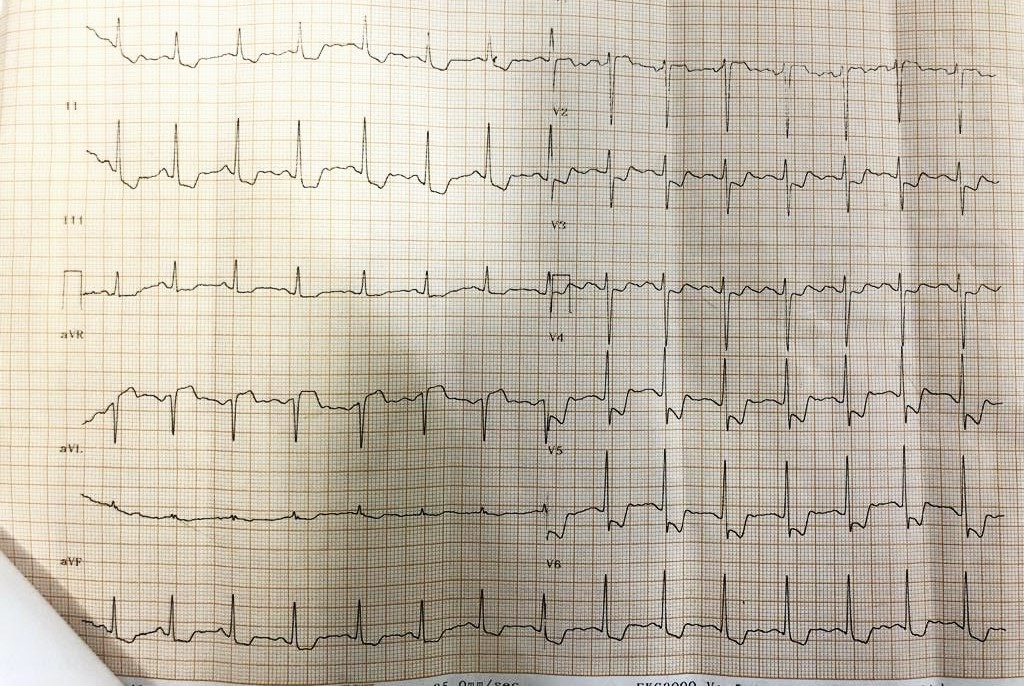
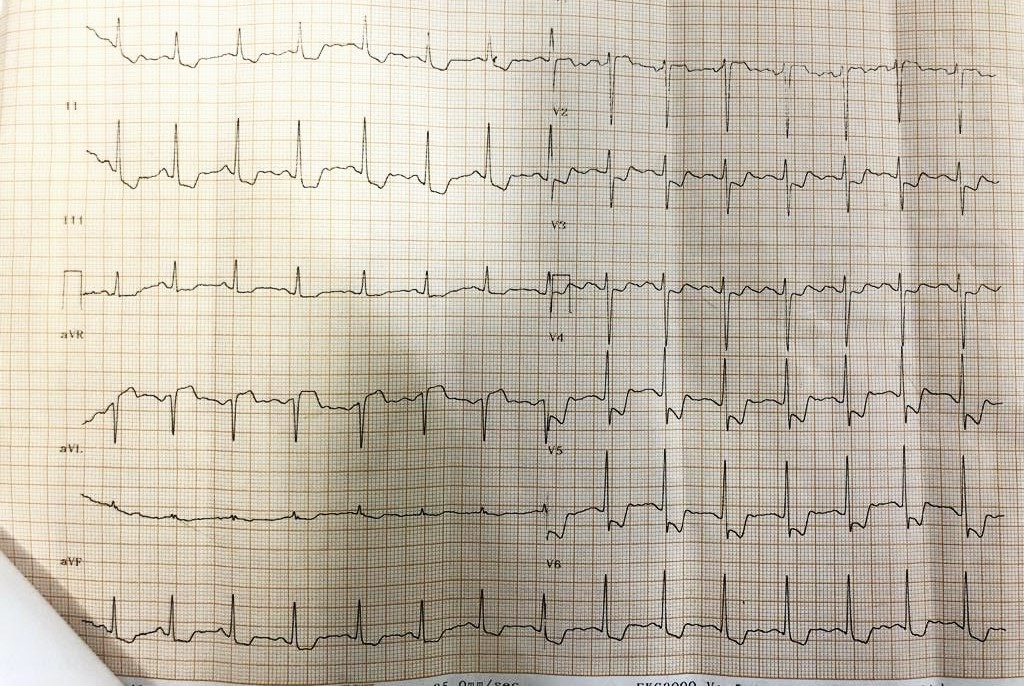
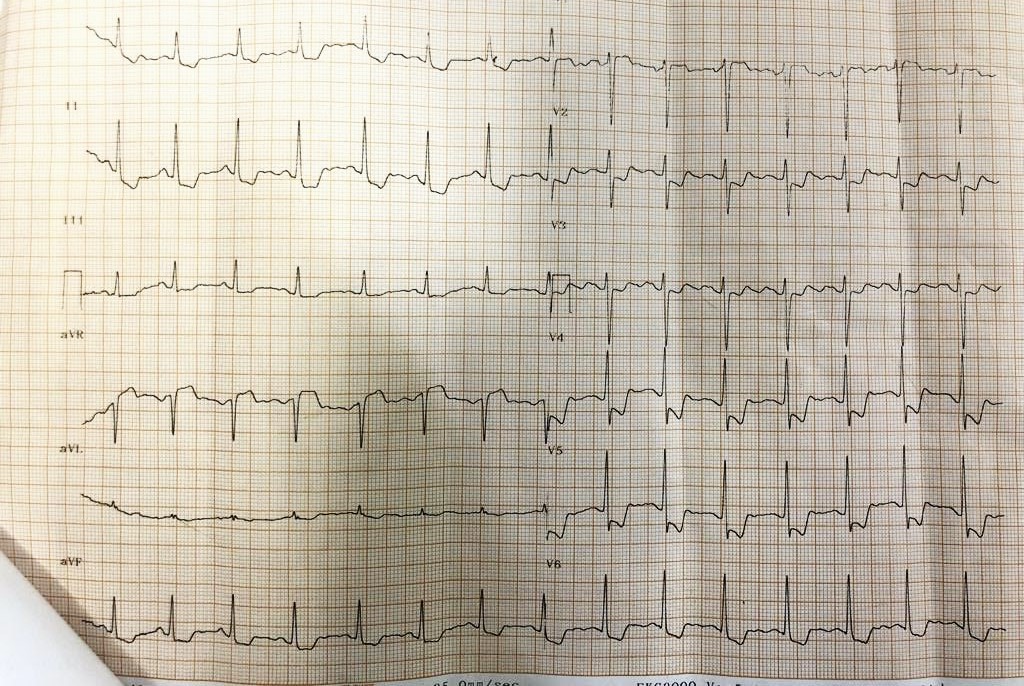
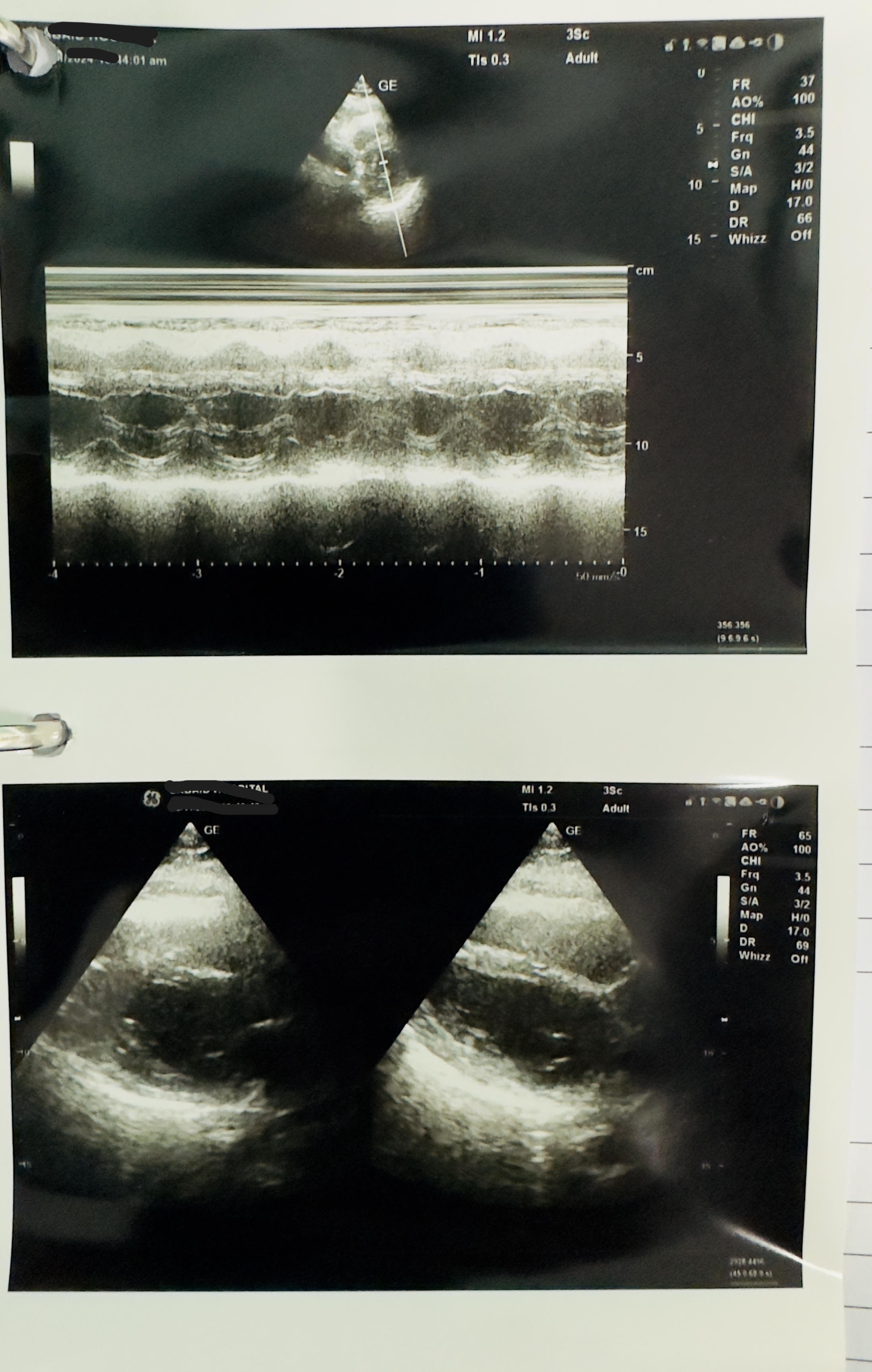
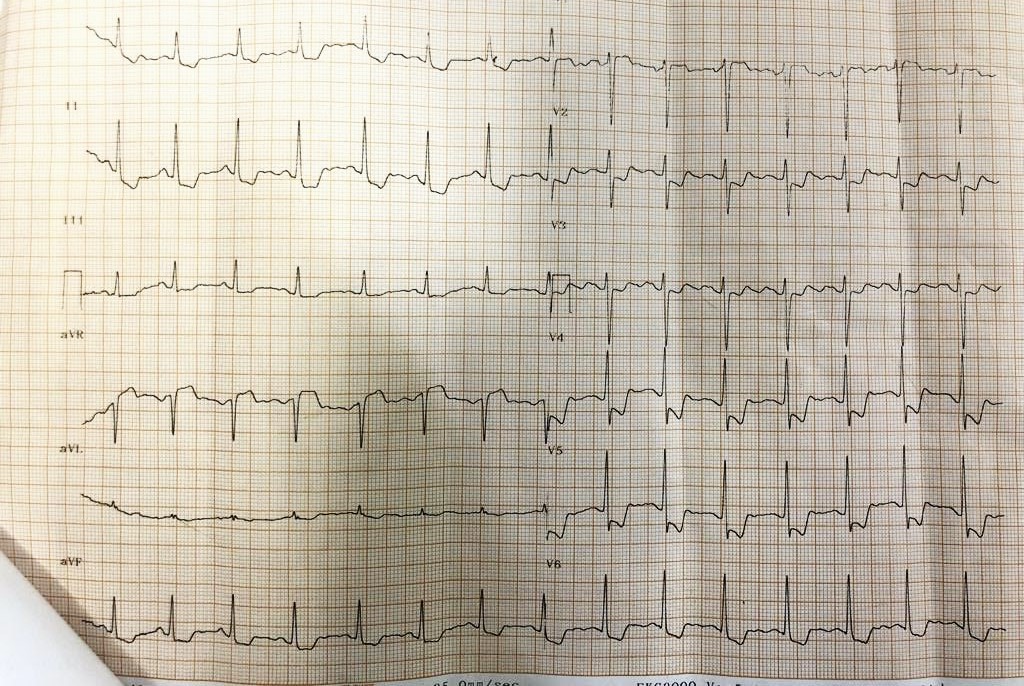
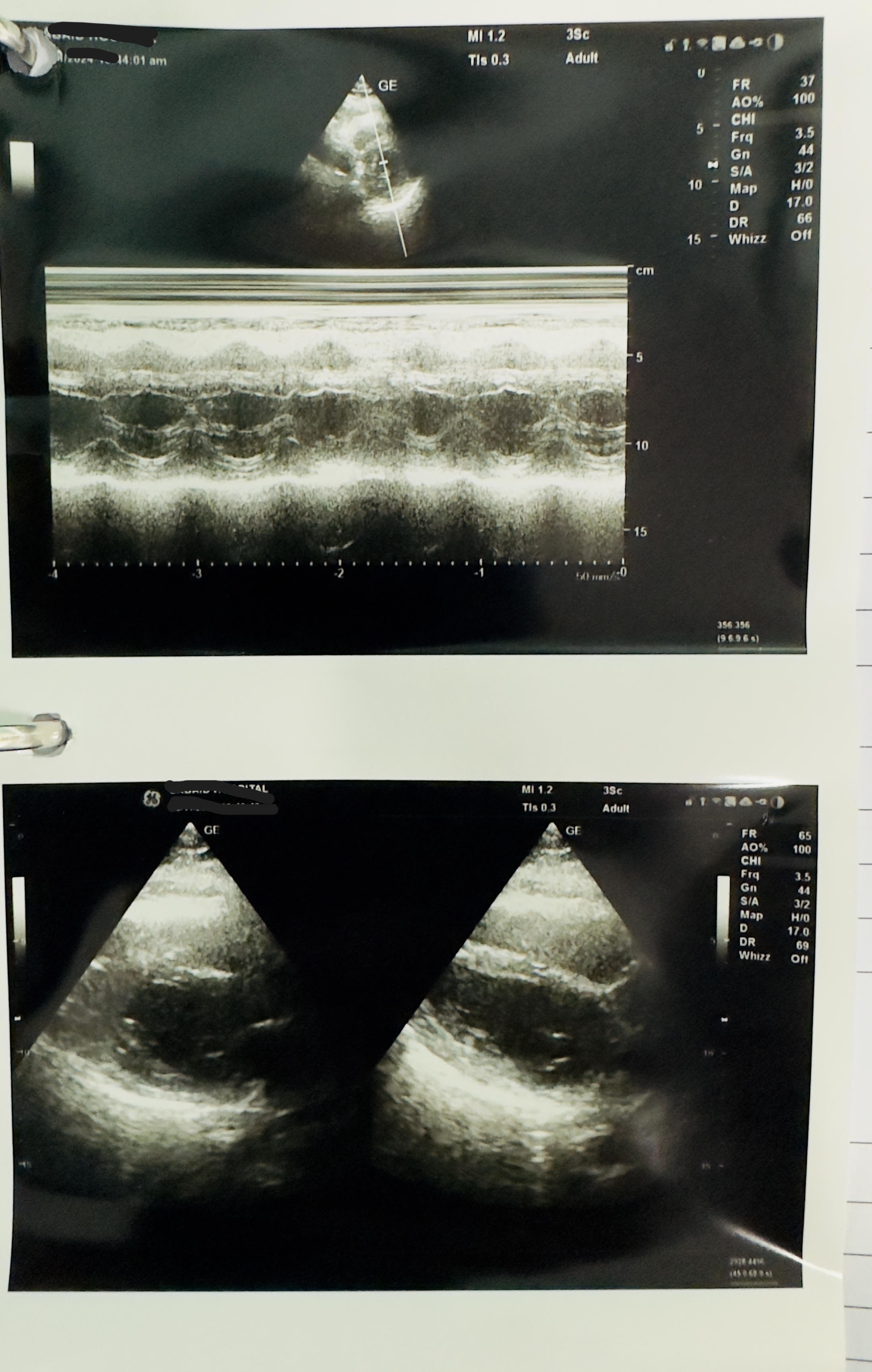
Relevant Test Results Prior to Catheterization
ECG showed Sinus Rhythm, HR 102 bpm, ST elevation in aVR with ST depression in V2 - V6 and lead I, II,III, aVF. Suggestive of Left Main STEMI. Echocardiography (TTE) : No Regional wall motion abnormalities, LVEF 60%. No pericardial effusion.Primary PCI activated .Chest X ray normalComplete blood count and Renal function , liver function test were unremarkable.Cardiac markers were elevated.


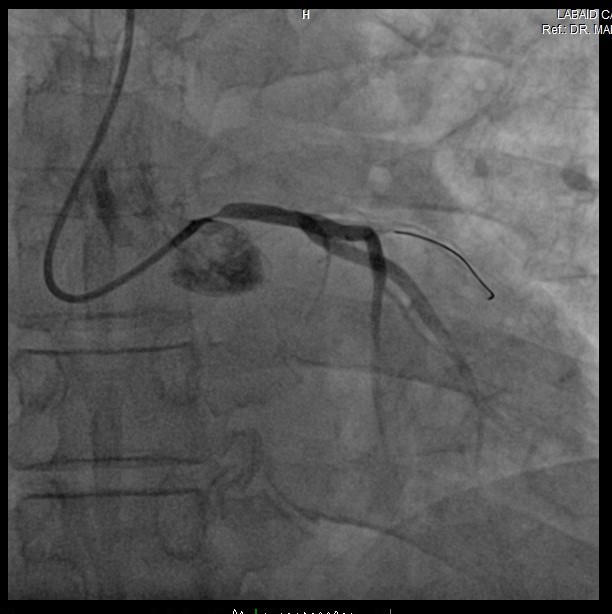
Relevant Catheterization Findings
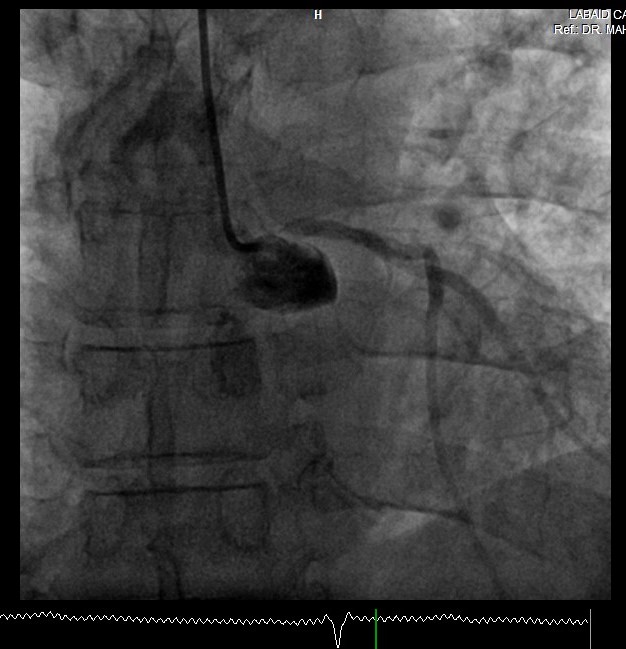
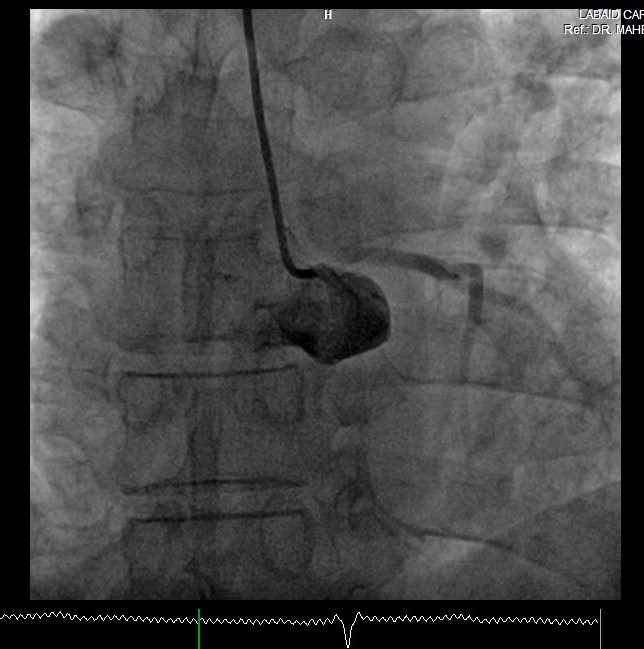
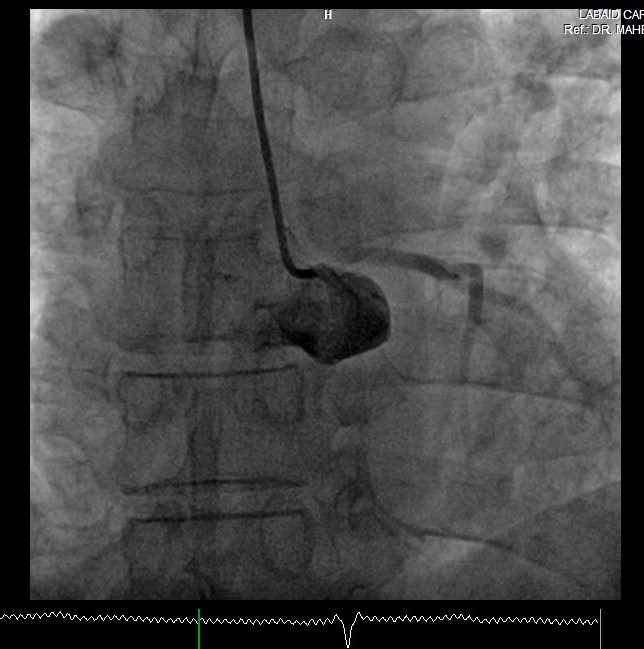
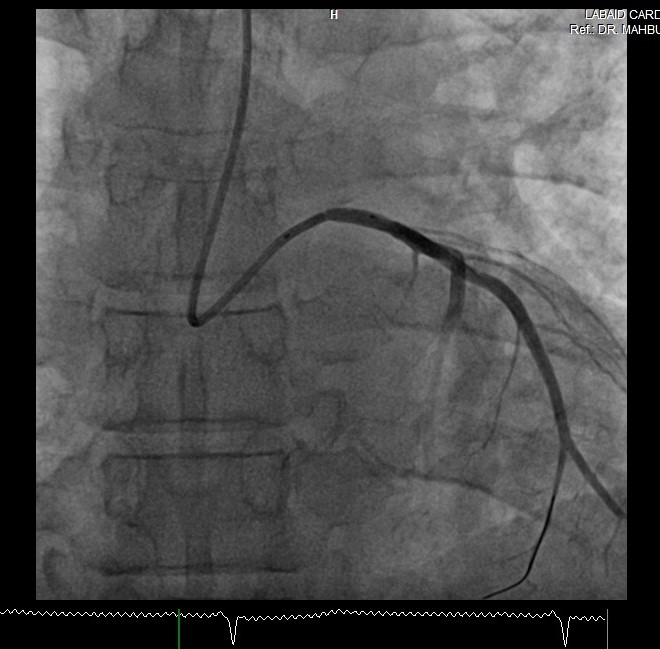
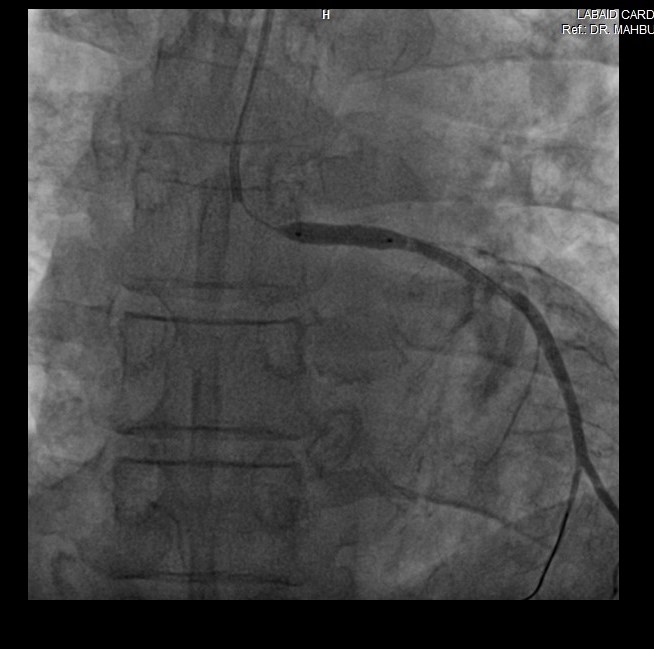
Coronary Angiography was performed via right radial access with terumo radial TIG 5Fr catheter. Coronary artery angiogram revealed right dominance coronary artery system and critical left main ostial stenosis (>95%) with TIMI II flow and other coronary arteries were normal. During procedure blood pressure was always damping when TIG 5Fr catheter engaged into ostial LMCA.
Interventional Management
Procedural Step
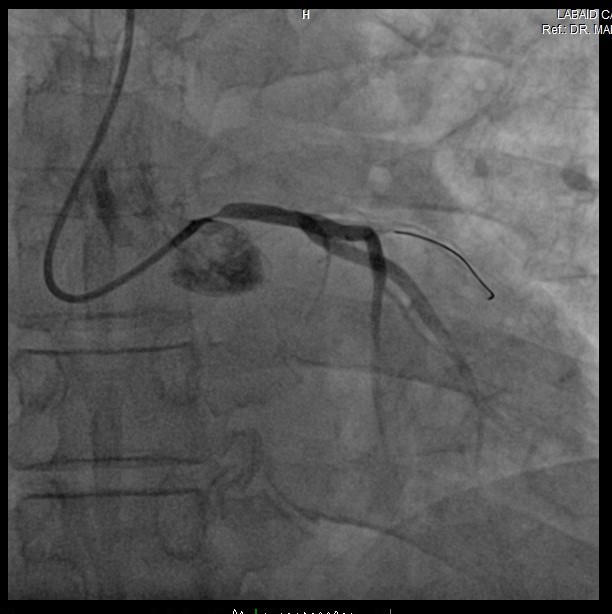
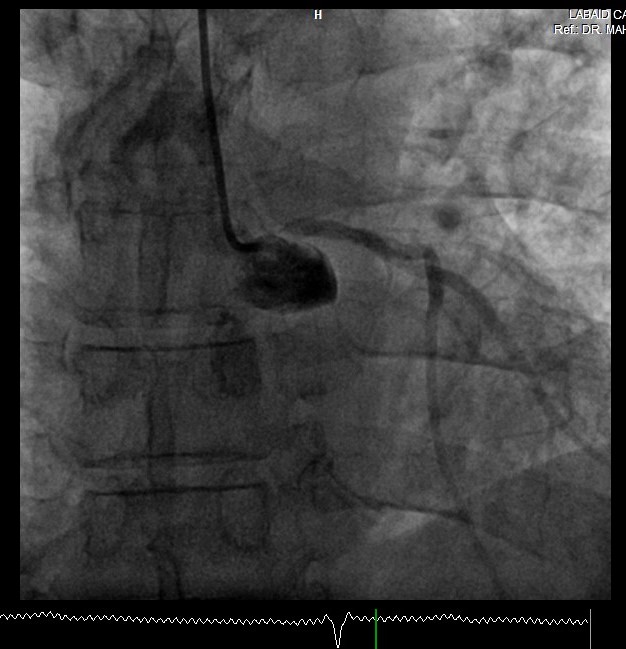
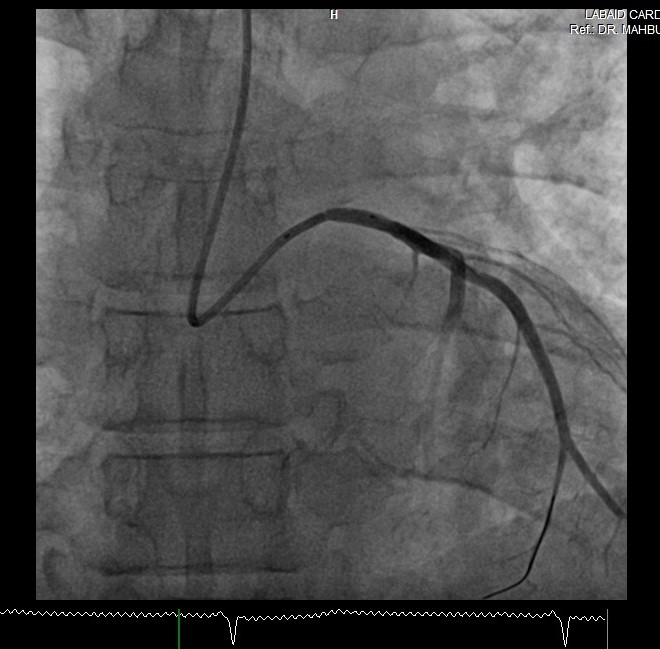
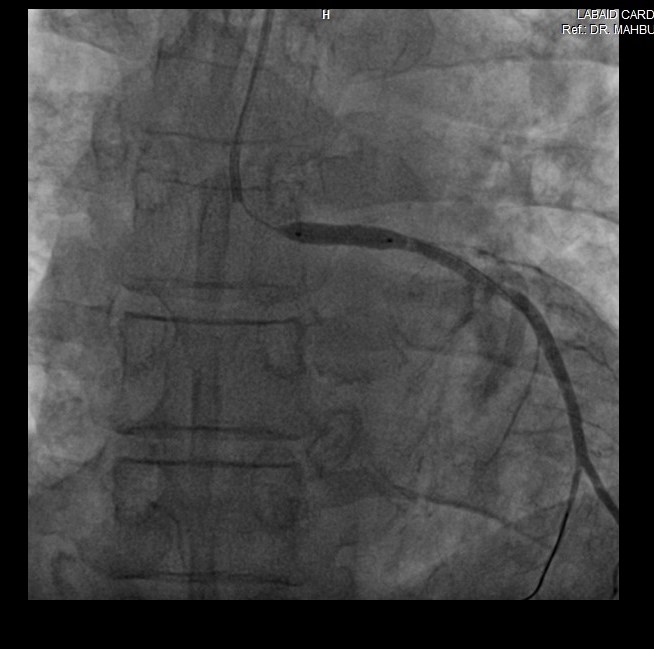
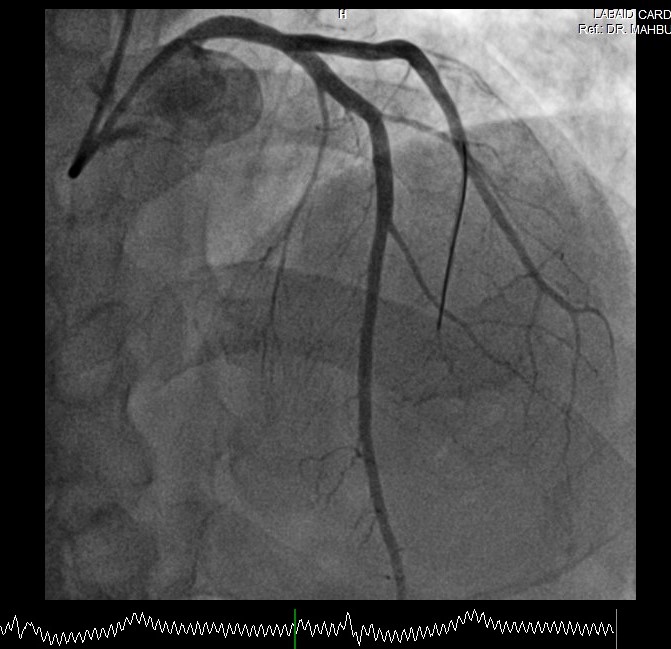
We decided to procced primary percutaneous coronary angioplasty via right radial access by using the 5F XB 3.5 catheter. We used Run through NS floppy wire for crossing left main to left circumflex coronary artery. We used a floating wire technique using workhorse wire Run through NS floppy because to ensure proper stent placement without hemodynamic disturbance due to catheter damping which causes a decrease in arterial pressure to the coronary arteries. Pre dilatation not done due to acute onset of symptoms and high chance of thrombus dislodgement. Direct Stent DSE 4.0 x 15mm was implanted in ostial LM to mid LM Inflated @ 14 Atmospheres pressure. After that we did post dilatation by using semi-compliance balloon (SB) 4.0 x 15mm inflated @ 18 ATM. Stent was well apposed and final result angiography was excellent and TIMI III flow without no residual lesion. The procedure was done without any complications. Total inj. heparin10000 unit given and ACT was 310 sec
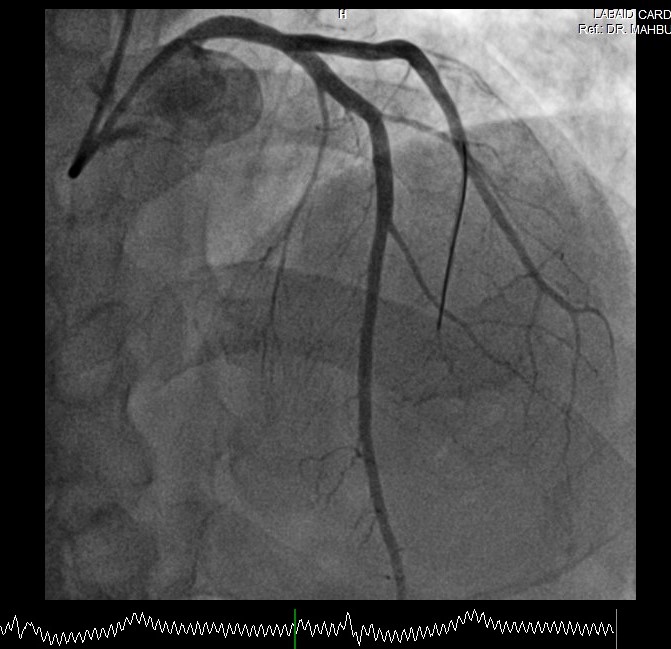
Case Summary
Primary Percutaneous coronary intervention (PPCI) to Ostial left main is one of the challenges that needs a special technique to prevent catheter damping, decrease arterial blood pressure and cardiac complications during procedure. The floating wire technique is one of the main techniques for facilitating aorta-ostial intervention. We report 55 year gentleman with sudden onset severe chest pain and suggestive LM STEMI. In this case, We decided to use the floating wire technique approach for stenting ostial LM coronary to prevent damping hemodynamic pressure during primary PCI to aorta-ostial lesion. The procedure was done without any complications and no residual lesion with TIMI III Flow.