Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-226
One-Stage Transcatheter Aortic Valve Implantation and Transcatheter Edge-to-Edge Tricuspid Valve Repair for Multiple Valvular Heart Disease in a High-Risk Patient
By Senthilraj Thangasami, Lim Su Min, Wang Bin, Wang Yan, Xiang Chen, Antonio Felipe Simao
Presenter
Senthilraj Thangasami
Authors
Senthilraj Thangasami1, Lim Su Min1, Wang Bin1, Wang Yan1, Xiang Chen1, Antonio Felipe Simao1
Affiliation
Xiamen Cardiovascular Hospital, China1,
View Study Report
TCTAP C-226
Structural - Tricuspid Valve Intervention
One-Stage Transcatheter Aortic Valve Implantation and Transcatheter Edge-to-Edge Tricuspid Valve Repair for Multiple Valvular Heart Disease in a High-Risk Patient
Senthilraj Thangasami1, Lim Su Min1, Wang Bin1, Wang Yan1, Xiang Chen1, Antonio Felipe Simao1
Xiamen Cardiovascular Hospital, China1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 72/yr male patient presented with acute heart failure characterized by bilateral pedal oedema, ascites and NYHA functional class IV dyspnea. His cardiovascular history included hypertension, dyslipidemia, bronchial asthma and Stage 3 chronic kidney disease. Jugular venous pressure was elevated at 10cm above the sternal angle. on auscultation there was a soft holosystolic murmur at the lower left sternal border with augmentation on inspiration and and an EDM on the left sternal border.
Relevant Test Results Prior to Catheterization
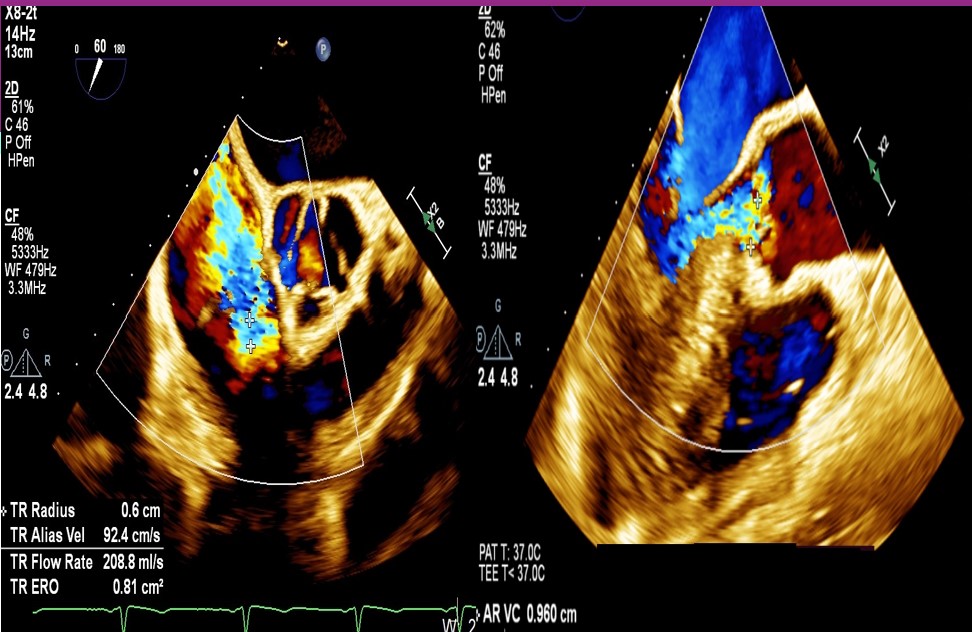
TTE was suggestive of valvular heart disease with severe AR, mild MR and severe TR with chordae rupture and prolapse of anterior leaflet of the tricuspid valve. TEE showed bi-atrial enlargement, left ventricular dilatation with diastolic dimension of 70mm. Left ventricular function was normal with ejection fraction of 70%. Aortic valve was thickened with no calcification of leaflets. Tricuspid annulus dimension measured 47mm, coaptation gap was 4.6mm with regurgitation volume of 65 ml.
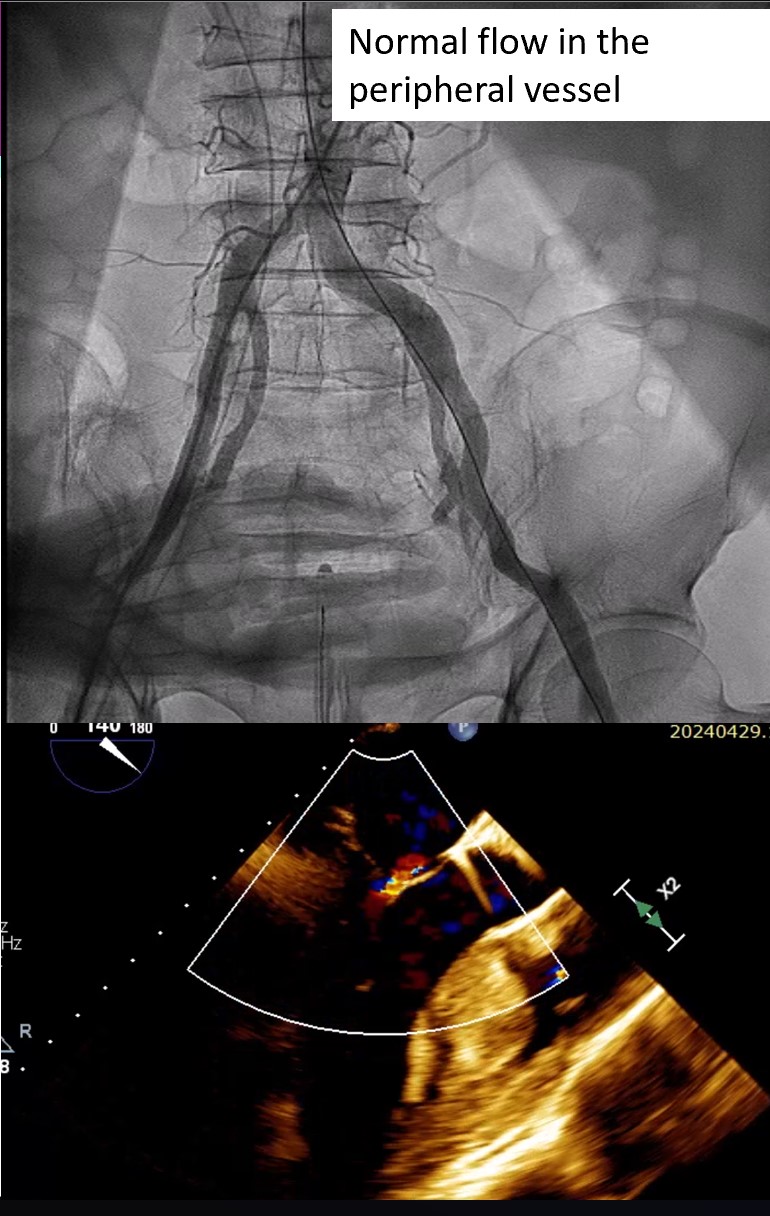
Relevant Catheterization Findings
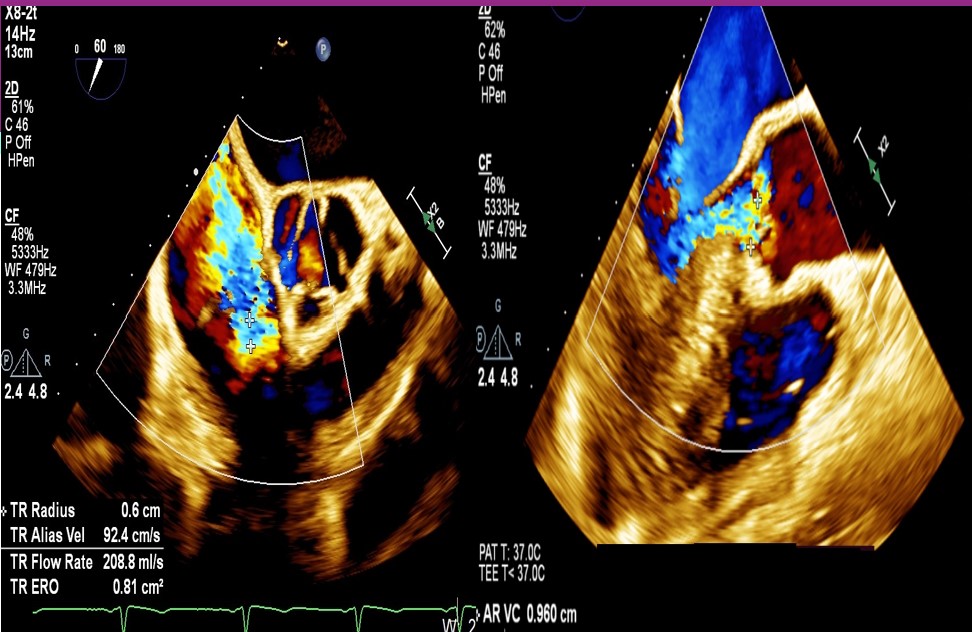
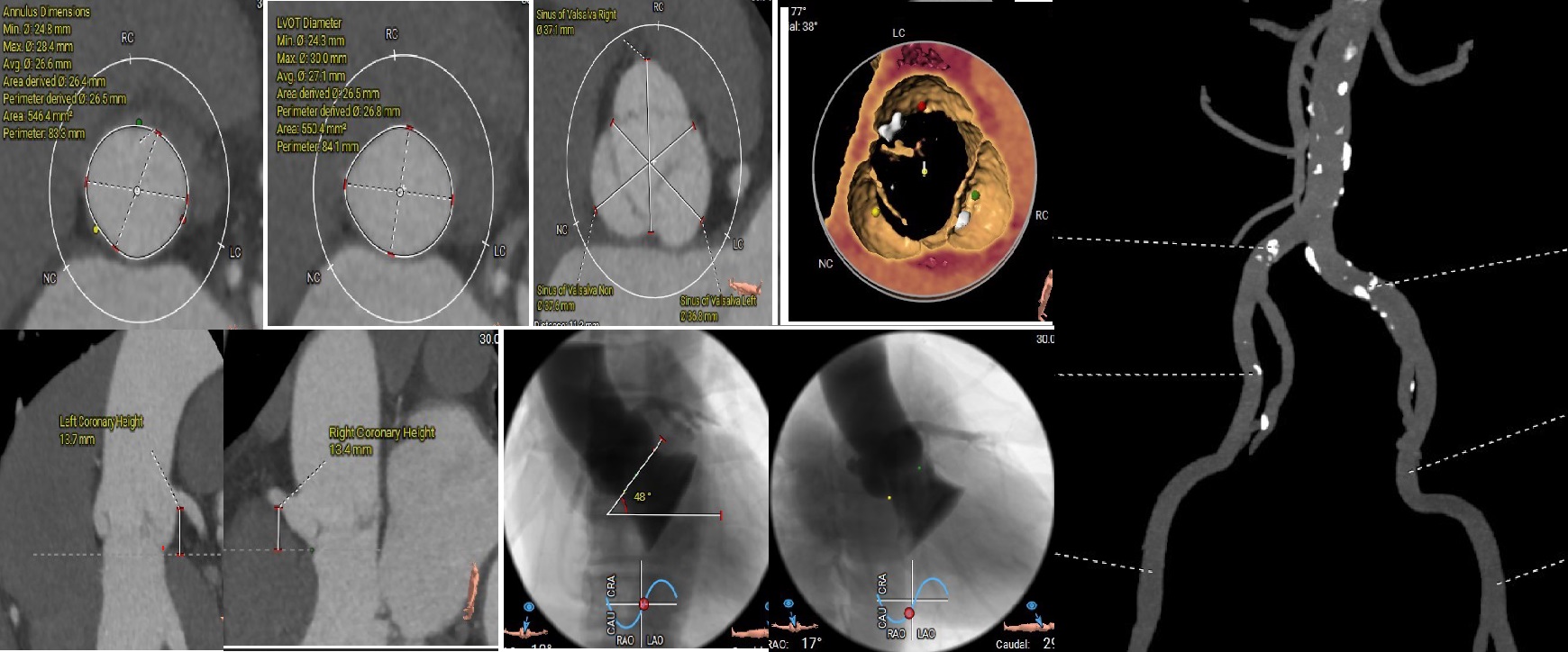
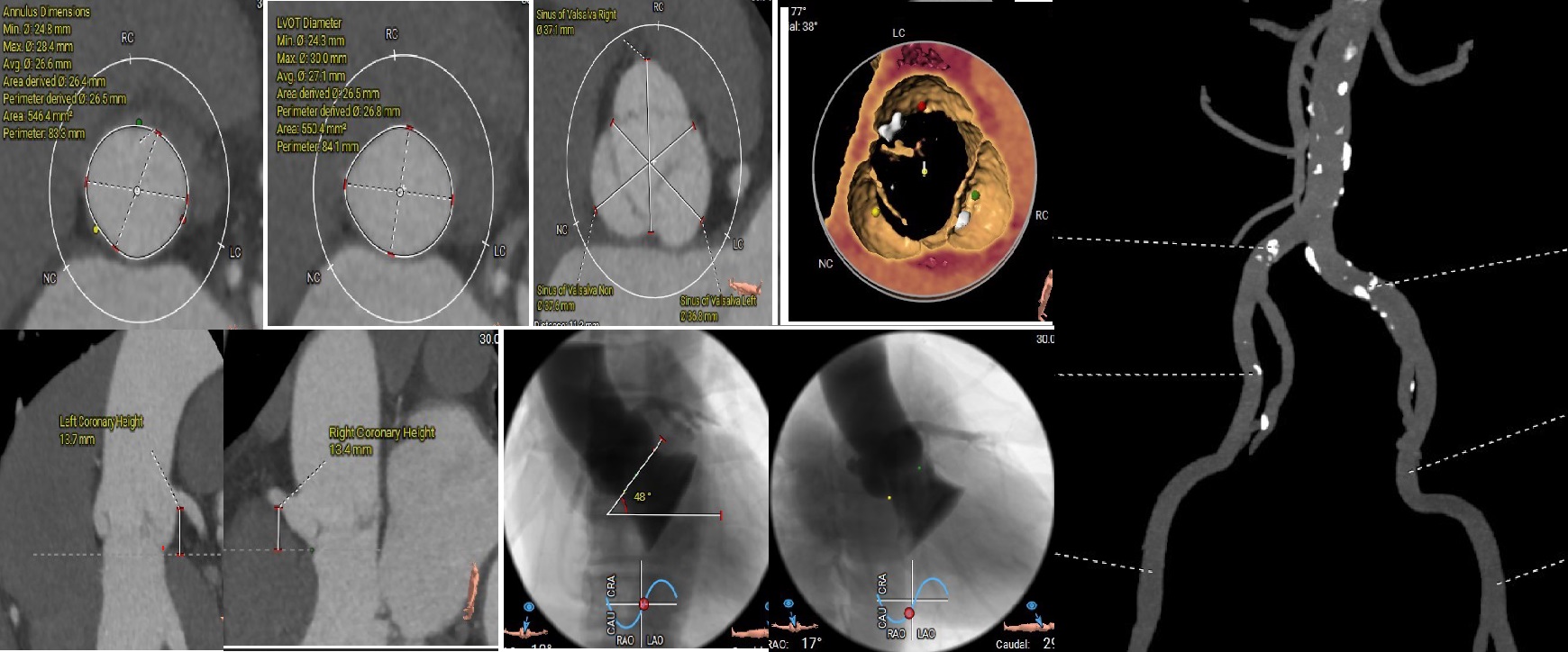
Based on the CTA, 30mm VitaFlow™ system self-expanding valve was decided with oversizing of 20%. Coronary angiogram showed no coronary artery stenosis. Risk analysis showed high risk with Euroscore II of 27%. Multi-disclipinary team decided that a single stage percutaneous transcatheter approach would be the optimal treatment option for addressing the AR and TR. Tricuspid TEER followed by TAVI was decided to avoid interference of temporary pacemaker wire during clip deployment.
Interventional Management
Procedural Step
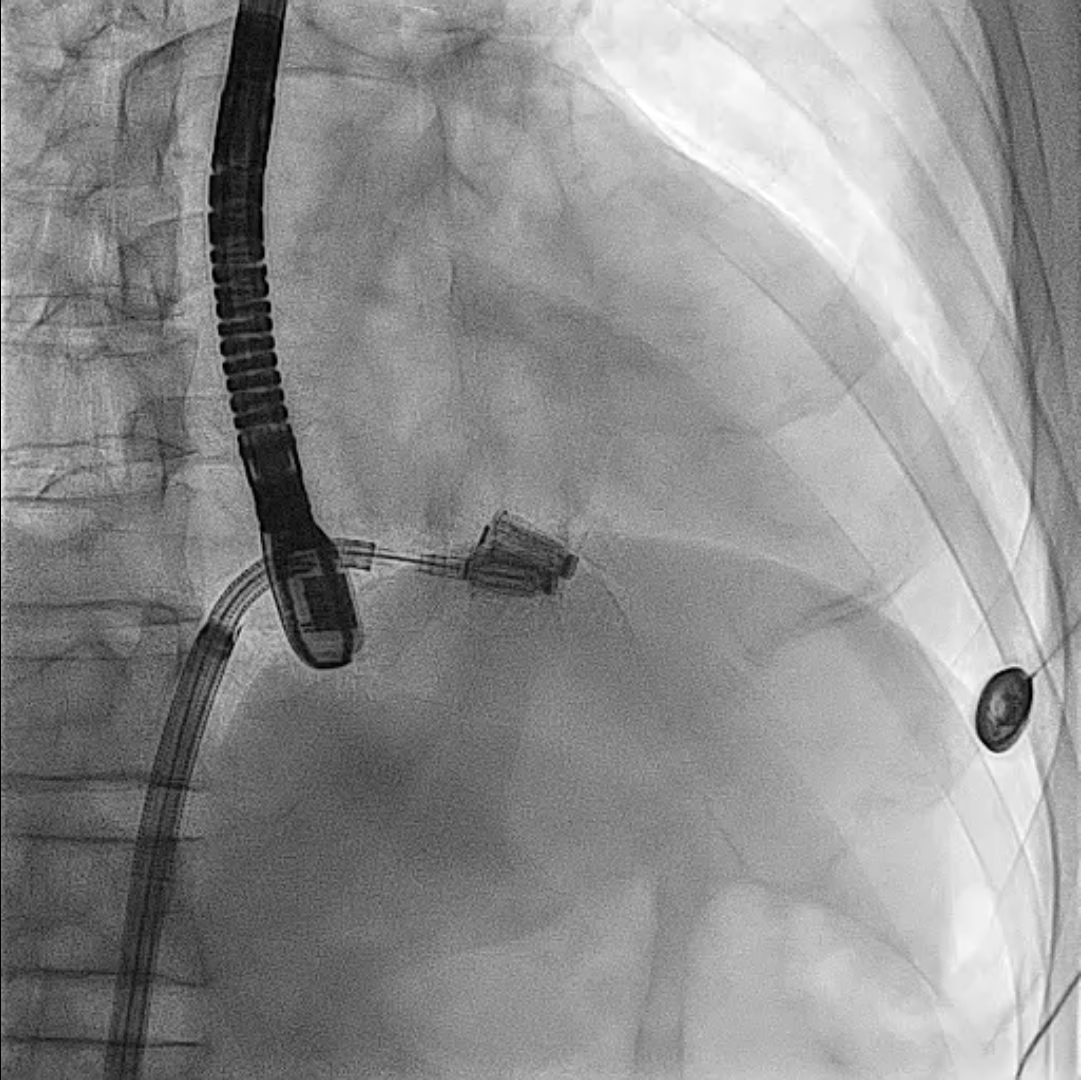
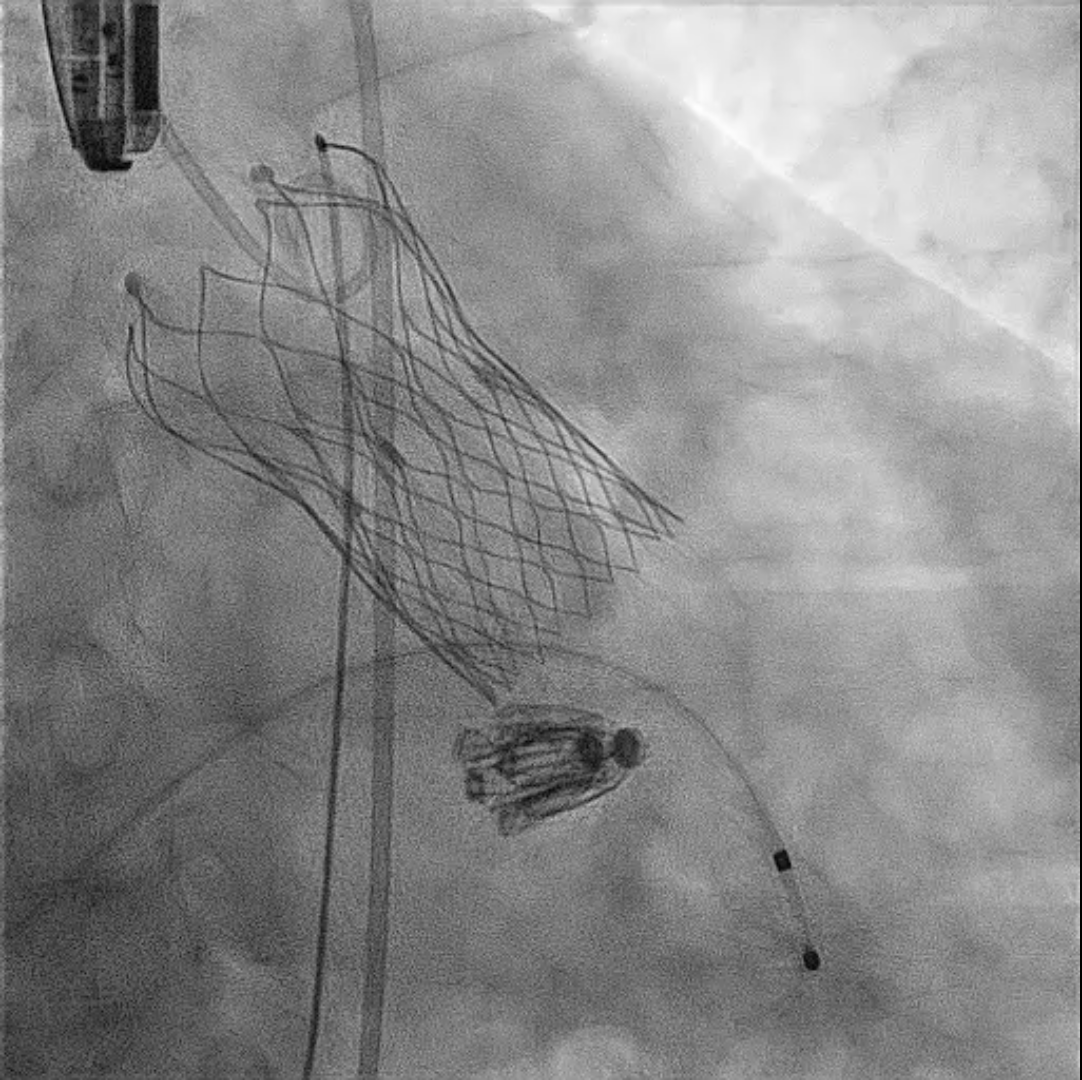
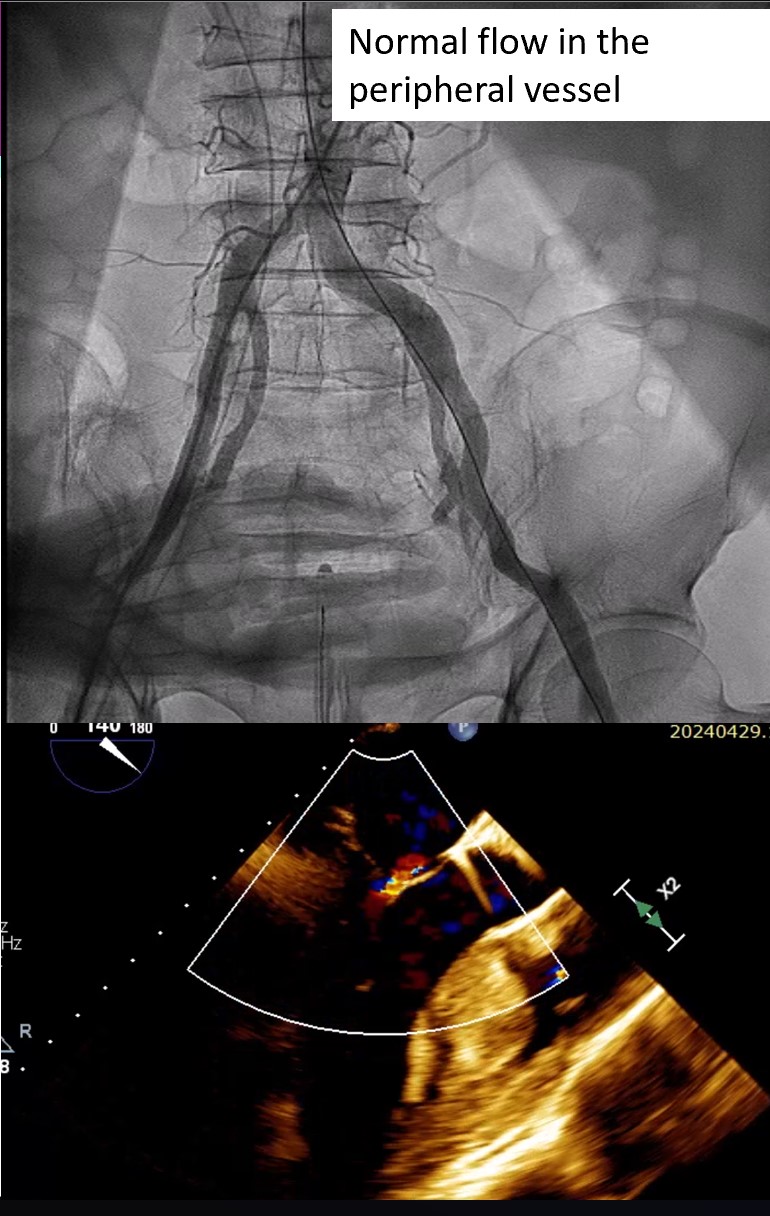
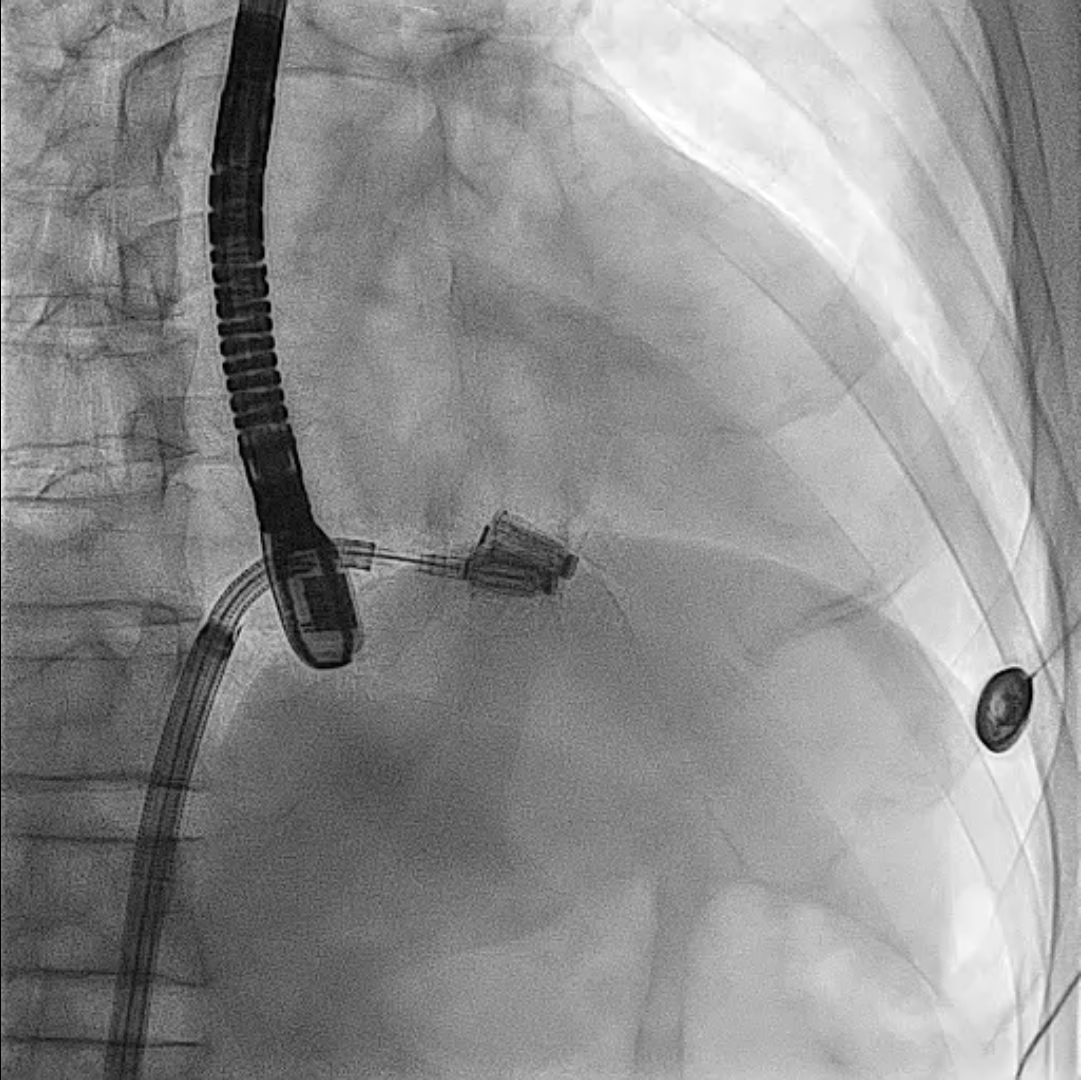
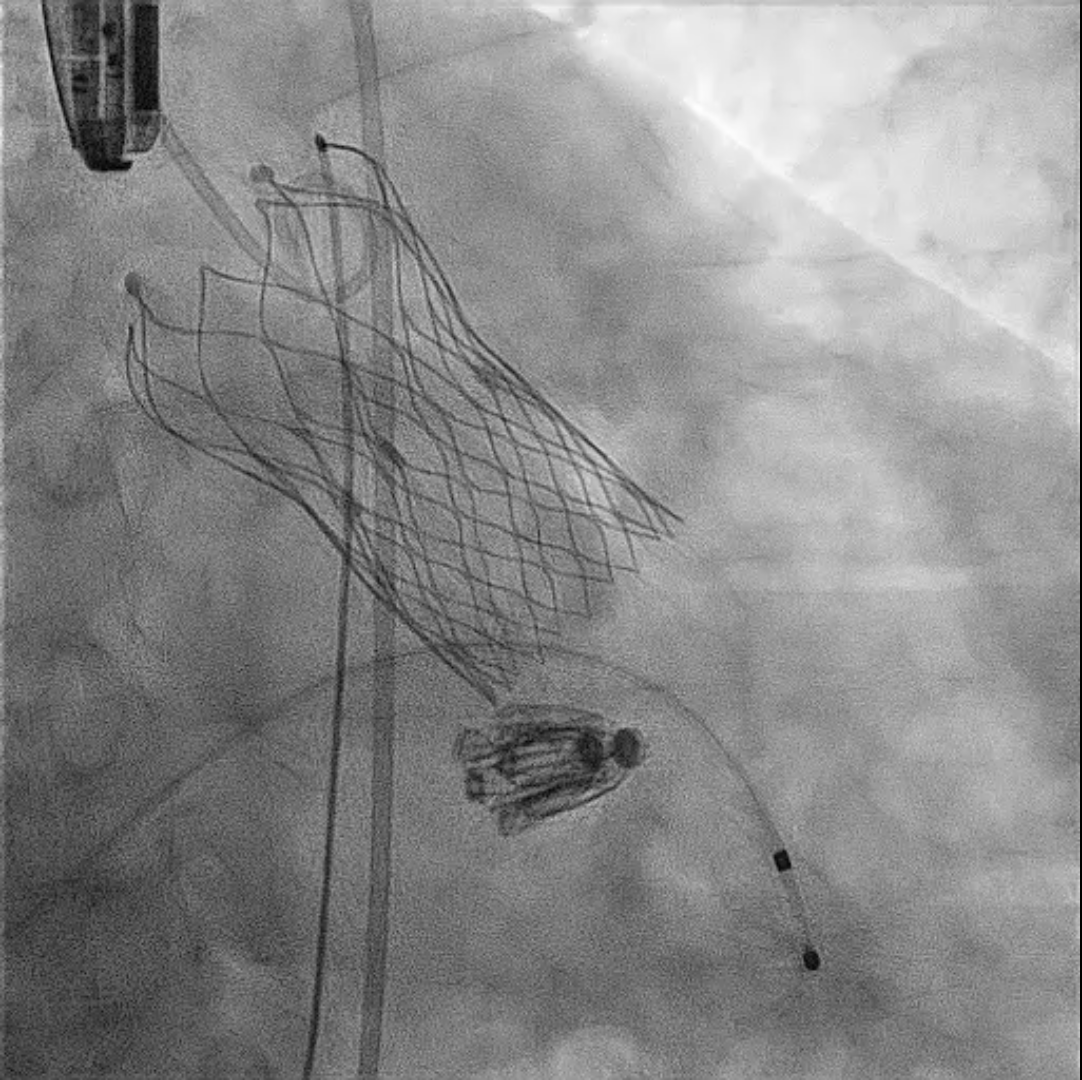
First, through the right femoral vein, the Neoblazar® delivery system (Dawneo Neoblazar, Hangzhou, China) was advanced till the tricuspid valve, and two clips (TMrCLAMP-S) were deployed to grasp the anterior and septal leaflets with a desired outcome reducing to a mild residual TR. Postoperative VC width was 0.2cm with EROA of 0.17cm2 and regurgitation volume of 15mL. The delivery system removed and 18 fr sheath exchanged. A 5 fr temporary pacemaker wire positioned through sheath into the right ventricle. Subsequently, the right and left femoral arteries were each accessed with 6-fr sheath and 22 fr sheath respectively. Through the left femoral artery, the TAVI delivery system with a 30mm VitaFlow Liberty™ self-expanding valve system (MicroPort®, Shanghai, China) was advanced across the aortic valve and deployed under transoesophageal and fluoroscopic guidance with rapid ventricular pacing at 140 beats/minute and pacing slowly tapered. The mean valvular gradient after TAVI decreased to 6 mmHg. Then, percutaneous access closure of arterial access was achieved using a pre-closure technique with the suture-mediated ProGlide device (Abbott Laboratories Inc., Chicago, Illinois, United States). The total procedure time was 60min. There were no intraoperative complications. The temporary pacemaker was removed two days later. Predischarge transthoracic echocardiogram showed a normal functioning aortic THV with a mean gradient of 6mmHg and mild residual tricuspid regurgitation.
Case Summary
The presence of TR in patients undergoing cardiac surgery increases operative risk and the persistence of postoperative TR is associated with worse long-term event-free survival. Observed mortality rate in patients with severe TR undergoing AVR is significantly higher than patients undergoing isolated AVR. Mild or moderate degrees of TR, if uncorrected during left-sided heart valve surgery, can progress in ≥25% of patients and result in right heart failure, increased hospitalization for heart failure, and decreased survival. This case illustrates the potential of combining percutaneous transcatheter interventions as an treatment option for high-risk patients with complex valvular condition.