Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-138
Extra Sandwich Fillings: Covered Stent-in-Stent With Wire Entrapment in a Left Main Bifurcation Lesion
By Yen-Yu Hsiao, I Li Su, Chia Sheng Chao
Presenter
Yen-Yu Hsiao
Authors
Yen-Yu Hsiao1, I Li Su1, Chia Sheng Chao1
Affiliation
Antai Medical Care Corporation Antai Tian-Sheng Memorial Hospital, Taiwan1,
View Study Report
TCTAP C-138
Coronary - Complication Management
Extra Sandwich Fillings: Covered Stent-in-Stent With Wire Entrapment in a Left Main Bifurcation Lesion
Yen-Yu Hsiao1, I Li Su1, Chia Sheng Chao1
Antai Medical Care Corporation Antai Tian-Sheng Memorial Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
An 84-year-old woman with hypertension, CKD, diabetes, and Cushing syndrome presented with altered consciousness and dyspnea. On arrival, her vital signs showed BP 112/78 mmHg, HR 125 bpm, and SpO₂ 66% on room air. Physical examination revealed bilateral rales, and distant heart sounds. Chest X-ray revealed bilateral pulmonary congestion, cephalization of vessels, and no consolidation, suggesting heart failure.


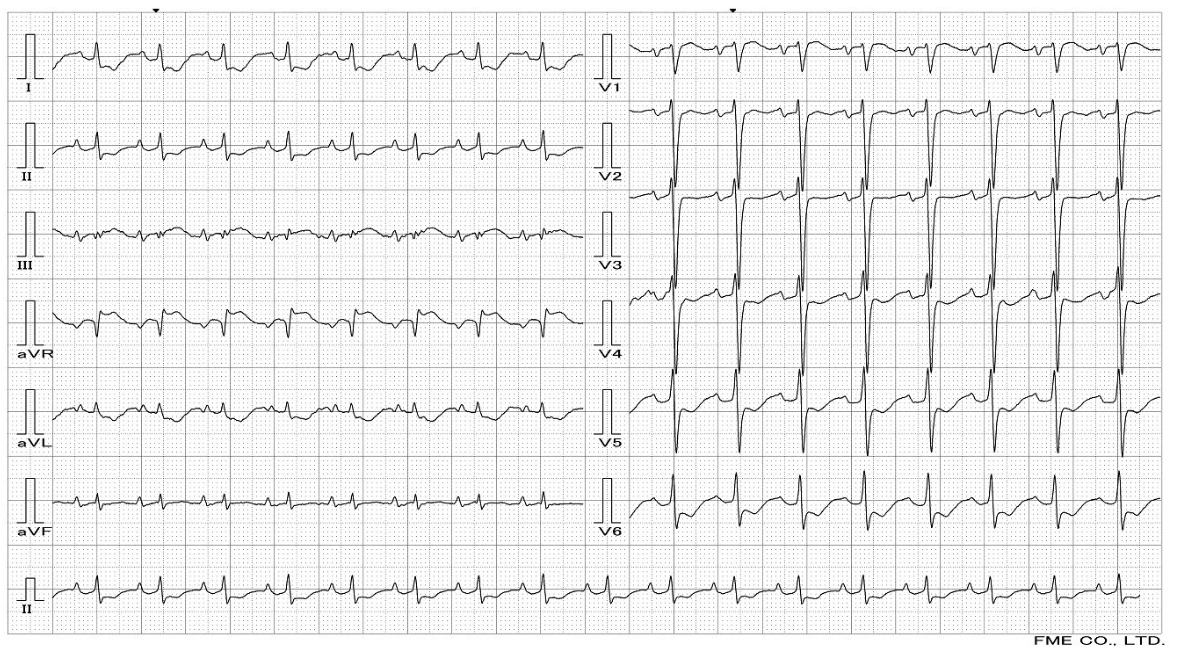
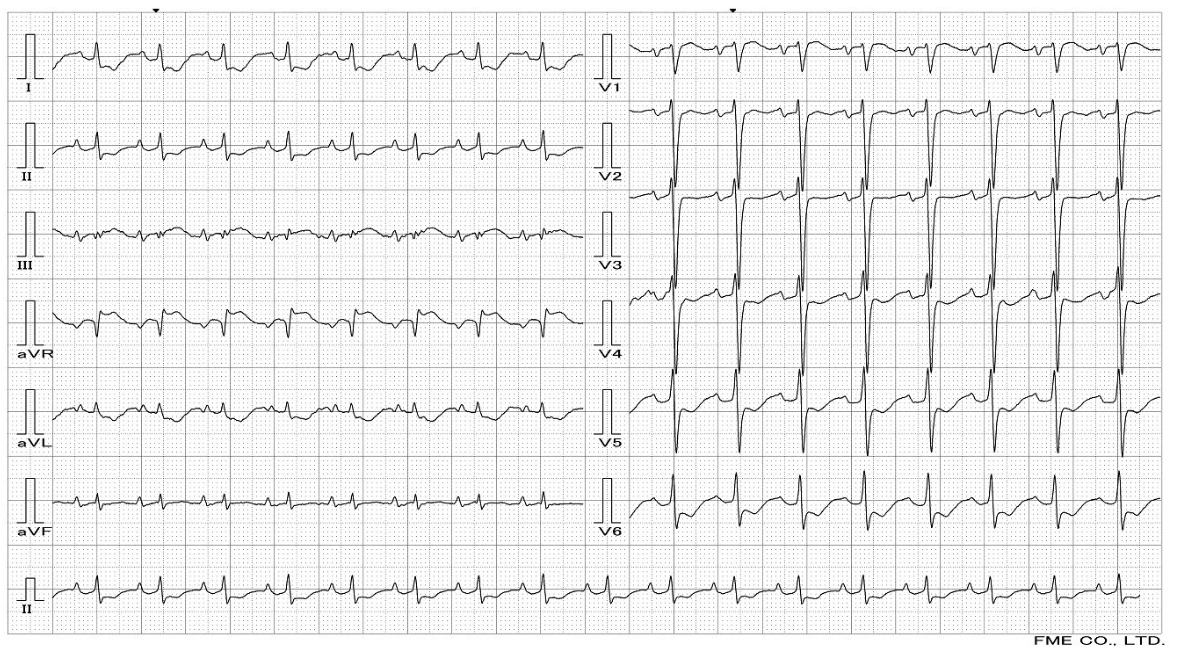
Relevant Test Results Prior to Catheterization
Her ECG demonstrated ST depressions and T wave inversions in leads V2-V6, I, II, aVL, and aVF, indicating myocardial ischemia, potentially secondary to hypoxia and coronary artery disease. Laboratory results showed elevated Troponin I at 1.55 ng/mL and NT-proBNP at 7310 pg/mL, consistent with acute decompensated heart failure.
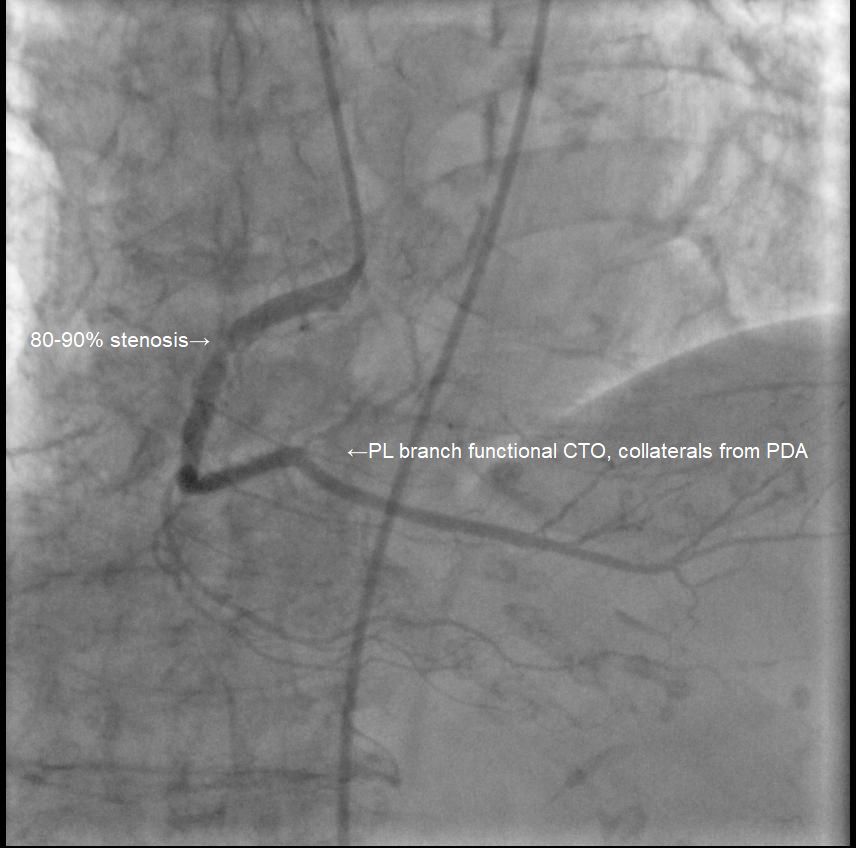
Relevant Catheterization Findings
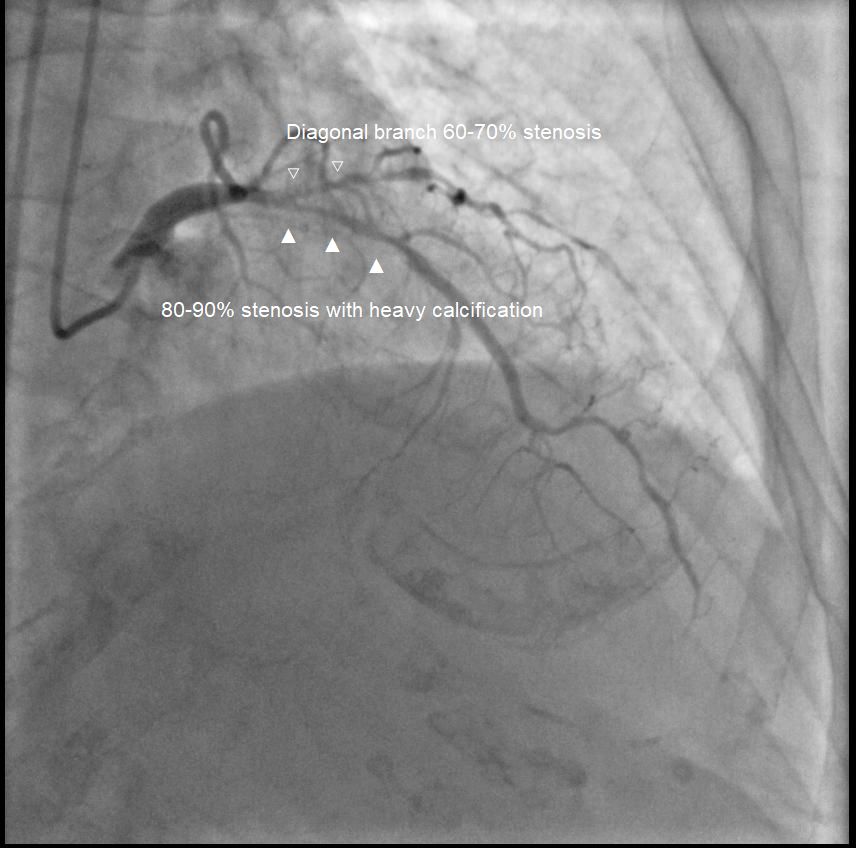
Coronary angiography showed significant stenosis:
Left main 50-60%,
LAD 80-90% (proximal to mid) with heavy calcification, diagonal branch 60-70%,
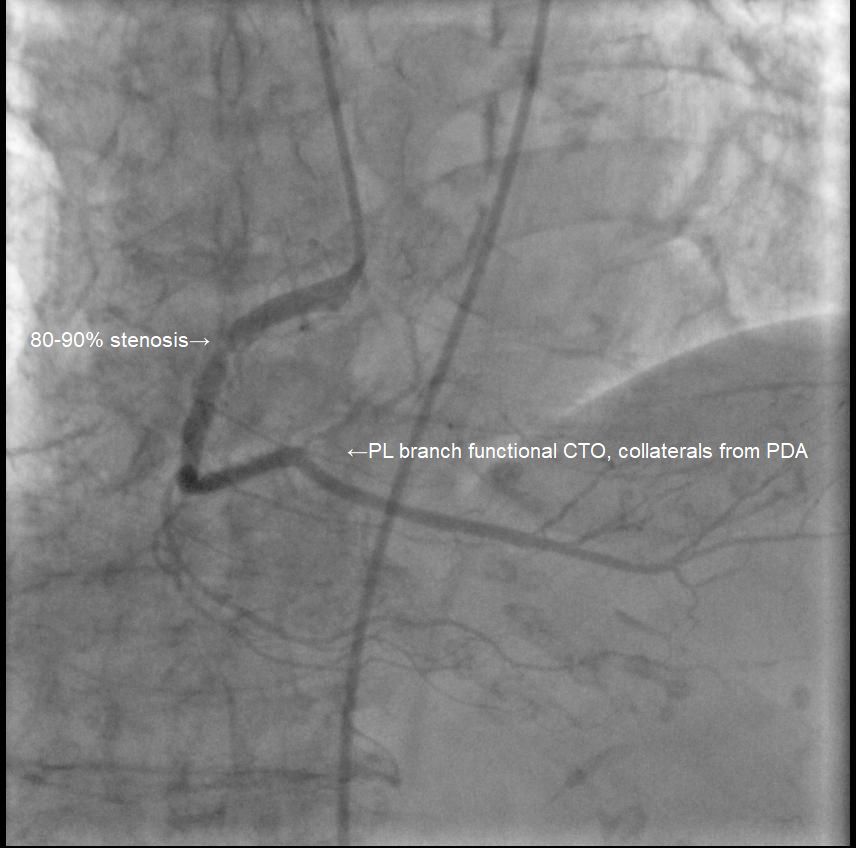
LCx 90-95% (ostium to proximal),
RCA 80-90% (proximal to mid), and PL branch functional CTO, collaterals from PDA, indicating multi-vessel disease.

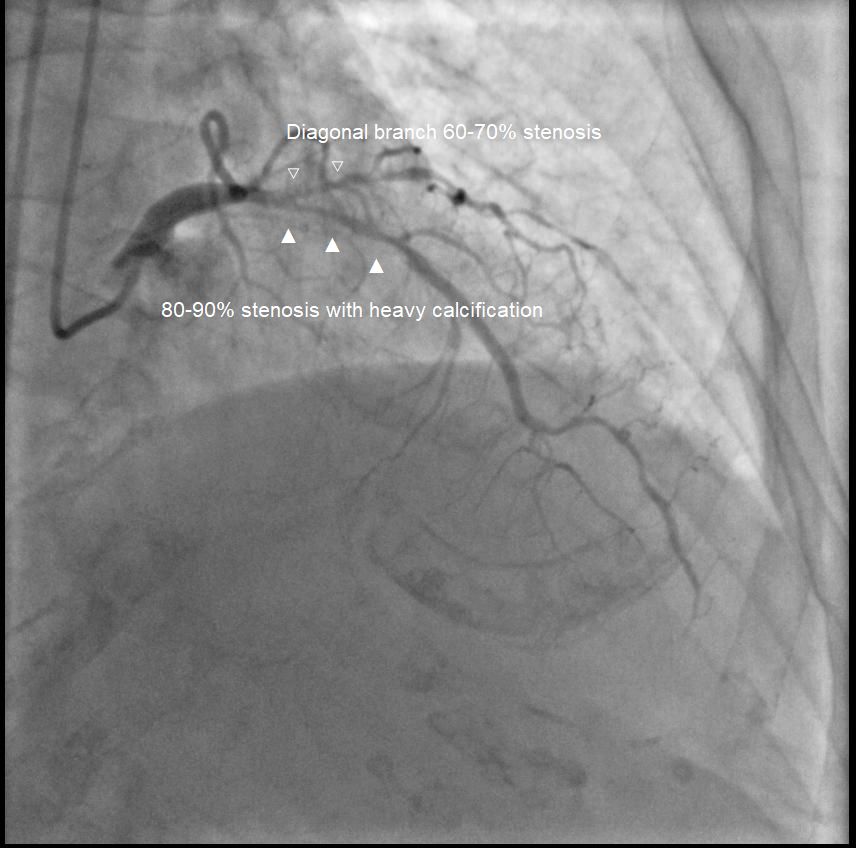
Left main 50-60%,
LAD 80-90% (proximal to mid) with heavy calcification, diagonal branch 60-70%,
LCx 90-95% (ostium to proximal),
RCA 80-90% (proximal to mid), and PL branch functional CTO, collaterals from PDA, indicating multi-vessel disease.

Interventional Management
Procedural Step
Day 1:
IABP via R femoral artery, with 1 : 1 pumping.
7Fr SL 3.5 catheter via L femoral artery to LMCA. Runthrough wire to LAD distal, and Sion wire to D1.
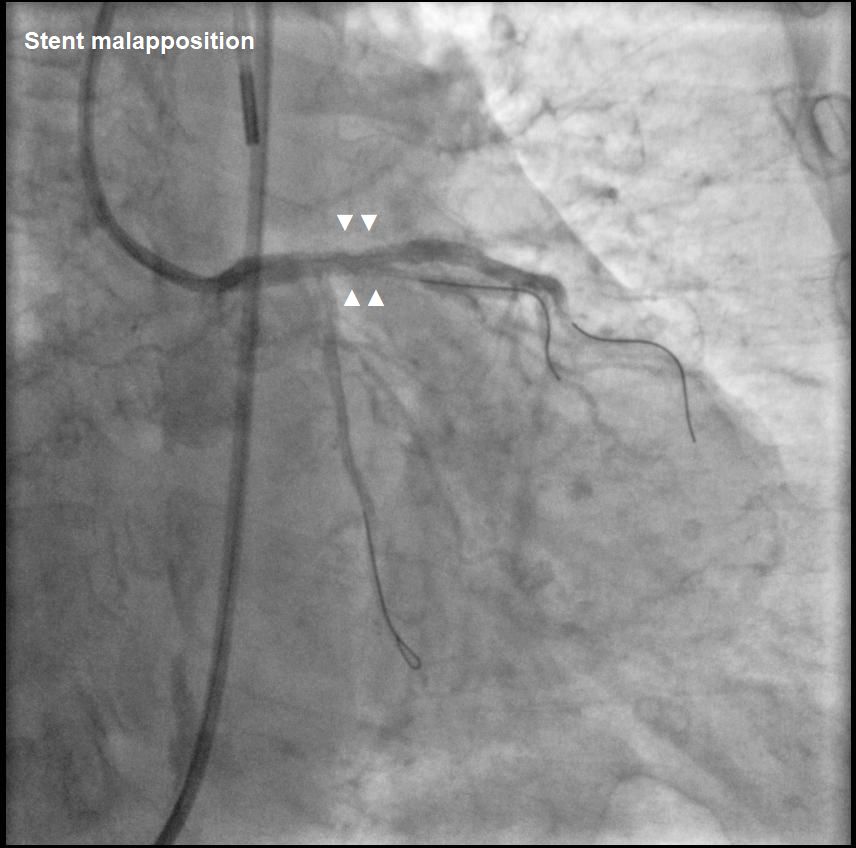
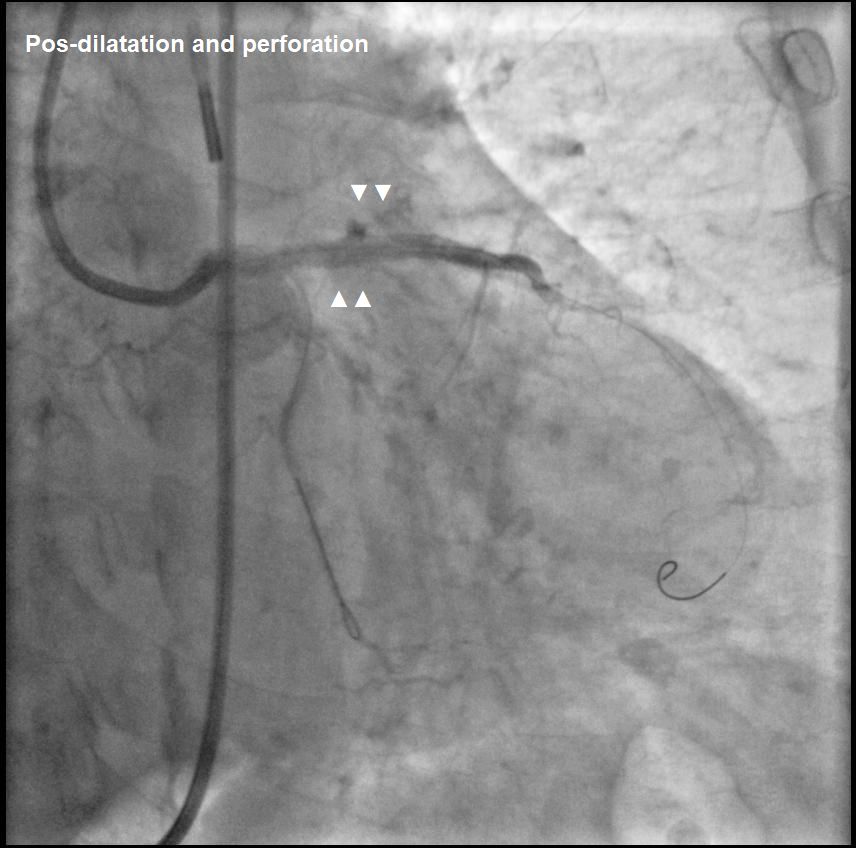
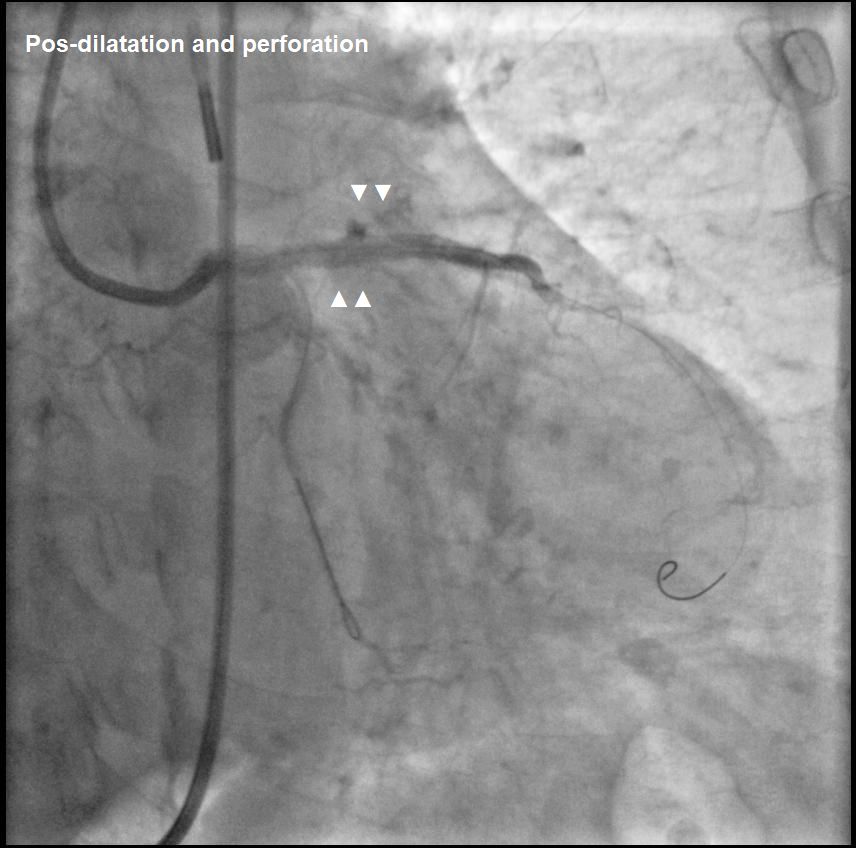
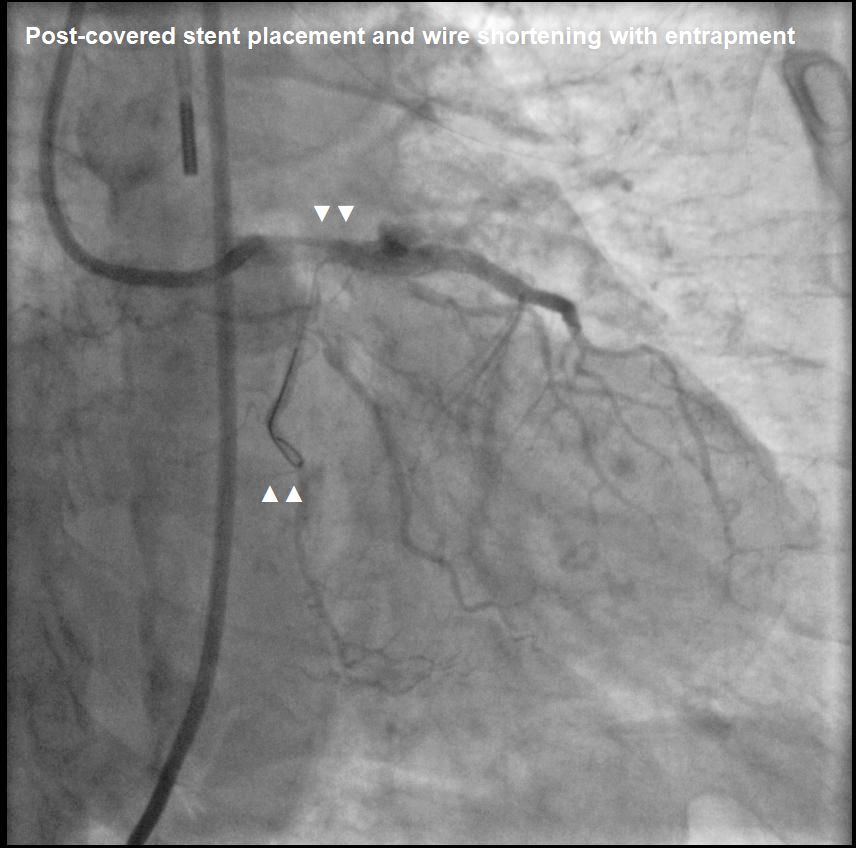
Post-dilatation with NC Sapphire 3.5 × 15 mm.Coronary perforation (Ellis III) in LAD proximal: prolonged inflation with NC Sapphire 3.5 × 15 mm. Persistent perforation treated with covered stent (Abbot Graftmaster) 2.8 × 19 mm.
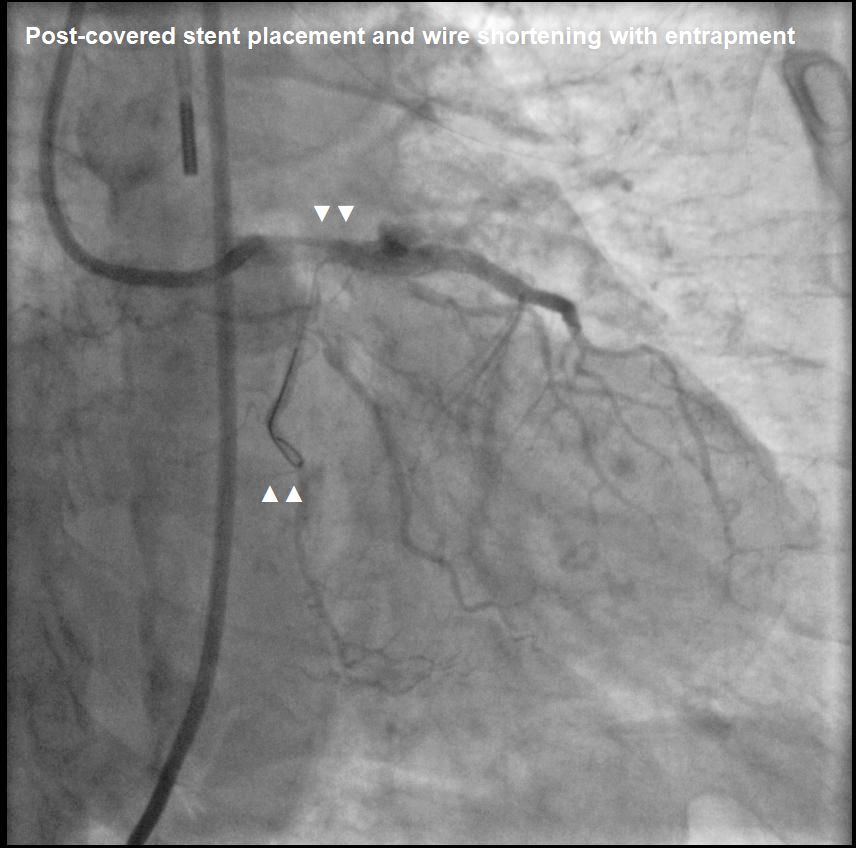
Wire entrapment from LCx to LAD-LM.Median sternotomy, CPB established. LV venting via RSPV & PA. Cardioplegia via root. Aortocoronary bypass to mid-LAD with vein graft. V-A ECMO post-CPB.
7fr SL 3.5 catheter to LMCA. PTCA with Sapphire 2.5 × 20 mm and NC Conqueror 3.5 × 20 mm at LCx to LMCA. BMS (Waltz) 2.5 × 33 mm stent at LCx mid. BMS (Waltz) 3.5 × 18 mm stent at LCx to LMCA.
Post-dilatation with NC Conqueror 2.5 × 20 mm, 3.5 × 15 mm, 4.0 × 12 mm.
Final angiogram: TIMI III flow from LMCA to LCx.
Aorta incised, wire cut near LMCA ostium.
Aortorrhaphy with 5-0 Prolene. CPB weaned, wound closed.
IABP via R femoral artery, with 1 : 1 pumping.
7Fr SL 3.5 catheter via L femoral artery to LMCA. Runthrough wire to LAD distal, and Sion wire to D1.
Post-dilatation with NC Sapphire 3.5 × 15 mm.Coronary perforation (Ellis III) in LAD proximal: prolonged inflation with NC Sapphire 3.5 × 15 mm. Persistent perforation treated with covered stent (Abbot Graftmaster) 2.8 × 19 mm.
Wire entrapment from LCx to LAD-LM.Median sternotomy, CPB established. LV venting via RSPV & PA. Cardioplegia via root. Aortocoronary bypass to mid-LAD with vein graft. V-A ECMO post-CPB.
7fr SL 3.5 catheter to LMCA. PTCA with Sapphire 2.5 × 20 mm and NC Conqueror 3.5 × 20 mm at LCx to LMCA. BMS (Waltz) 2.5 × 33 mm stent at LCx mid. BMS (Waltz) 3.5 × 18 mm stent at LCx to LMCA.
Post-dilatation with NC Conqueror 2.5 × 20 mm, 3.5 × 15 mm, 4.0 × 12 mm.
Final angiogram: TIMI III flow from LMCA to LCx.
Aorta incised, wire cut near LMCA ostium.
Aortorrhaphy with 5-0 Prolene. CPB weaned, wound closed.
Case Summary
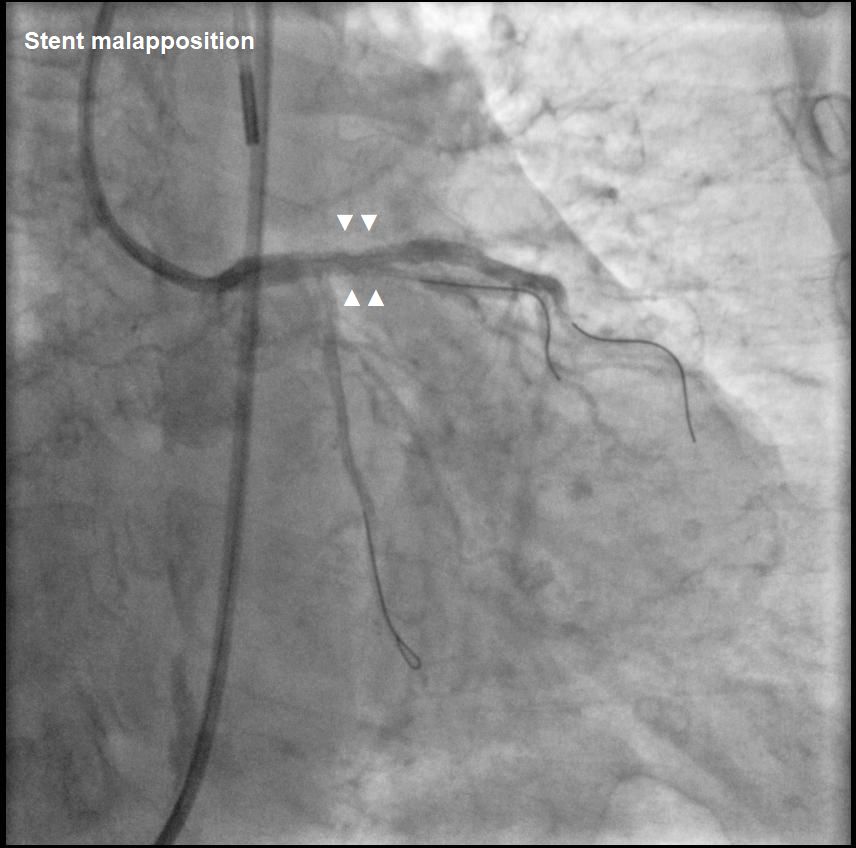
Guidewire entrapment during PCI is rare. In this case, the complication began with stent malapposition in the LAD, followed by post-dilatation that led to vessel perforation. During prolonged balloon inflation, the LCx wire was inadvertently pulled into the LAD, leading to guidewire entrapment when a covered stent was placed. Direct retrieval using a microcatheter was not possible, requiring surgery to cut the guidewire at the LM ostium, with the remaining LCx wire covered by a stent.